Chapter 6 – Brain and Spine
Tumours of the Brain
Case 1
Meningioma
Clinical:
History – This 90 year old female was being assessed for personality changes and the onset of aggressive behavior over the last year. Her family relayed that this was a slow, progressive change in behavior.
Symptoms – None
Physical – The patient was angry, uncooperative, and combative. No localizing physical findings
Laboratory – Non-contributory
DDx:
Brain Tumor
Meningioma
Silent Infarct
Subdural Hematoma
Imaging Recommendation
CT Head without and with IV contrast


Imaging Assessment
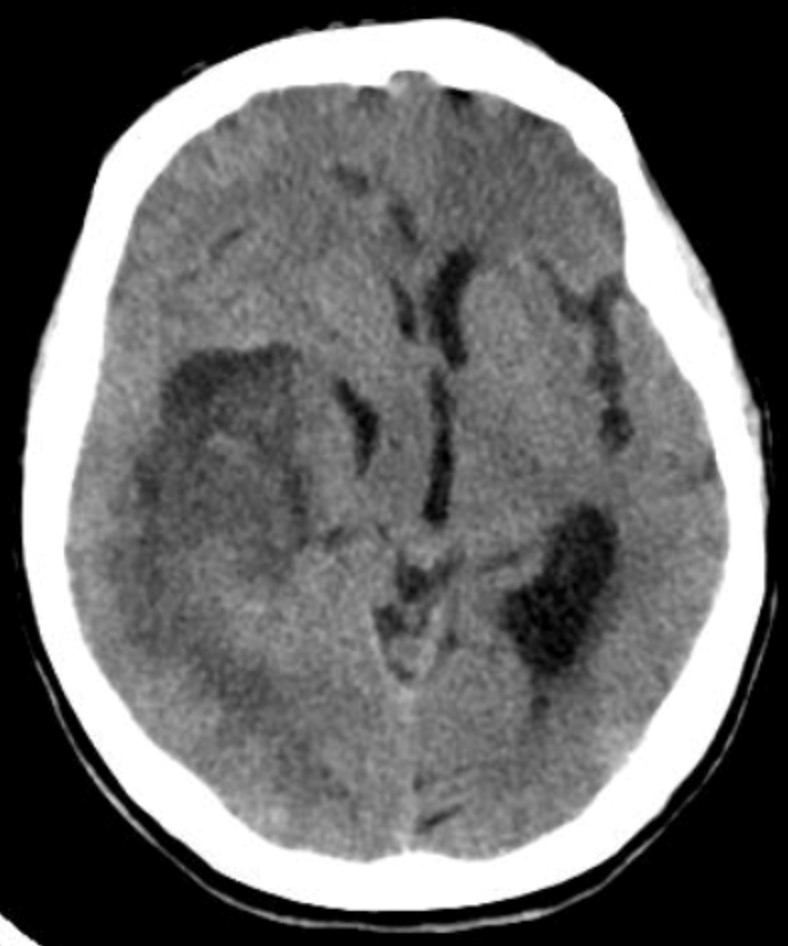
Findings:
A large, peripherally calcified, mass was seen in the right frontal region. There was moderate to severe vasogenic, parenchymal, edema associated with the mass. Moderate mass effect was seen with subfalcine herniation present. The base of the skull was mildly hyperostotic adjacent to the tumour.
Interpretation:
There was a large frontal mass, highly suggestive of a meningioma.
Diagnosis:
Meningioma
Discussion:
Meningiomas are the most common extra-axial mass, usually occurring in middle-aged patients, women > men. Meningiomas are non-glial, intracranial tumours that arise from the meninges. Their most common locations are parasagittal, over the convexities, the sphenoid wing, and the cerebellopontine angle, in decreasing frequency. They tend to be slow-growing with an excellent prognosis if surgically resected, but they may also rarely have more aggressive histology. When multiple, they may have an association with Neurofibromatosis type 2.
CT findings of Meningioma may include:
- On unenhanced CT, over half are hyperdense to normal brain and about 20% contain calcification.
- On contrast-enhanced studies, meningiomas enhance markedly.
- The tumors usually form an obtuse angle with the skull and may have a dural tail of tumour.
- The underlying bone may become dense and hypertrophied.
- If supplied by the middle meningeal artery, there may be enlargement of this artery and its groove in the skull.
- They may induce vasogenic edema in the adjacent brain parenchyma.
Case 2
Glioblastoma
Clinical:
History – This elderly lady was in a Nursing Home.
Symptoms – Obtunded, worsening confusion.
Physical – Semi-conscious. Disoriented. Left arm and leg weakness.
DDx:
Brain infarction
Subdural hematoma
Brain tumor
Imaging Recommendation
ACR – Cerebrovascular Disease, Suspected Intracranial Hemorrhage, Variant 12
CT Head without and with IV contrast
Imaging Assessment
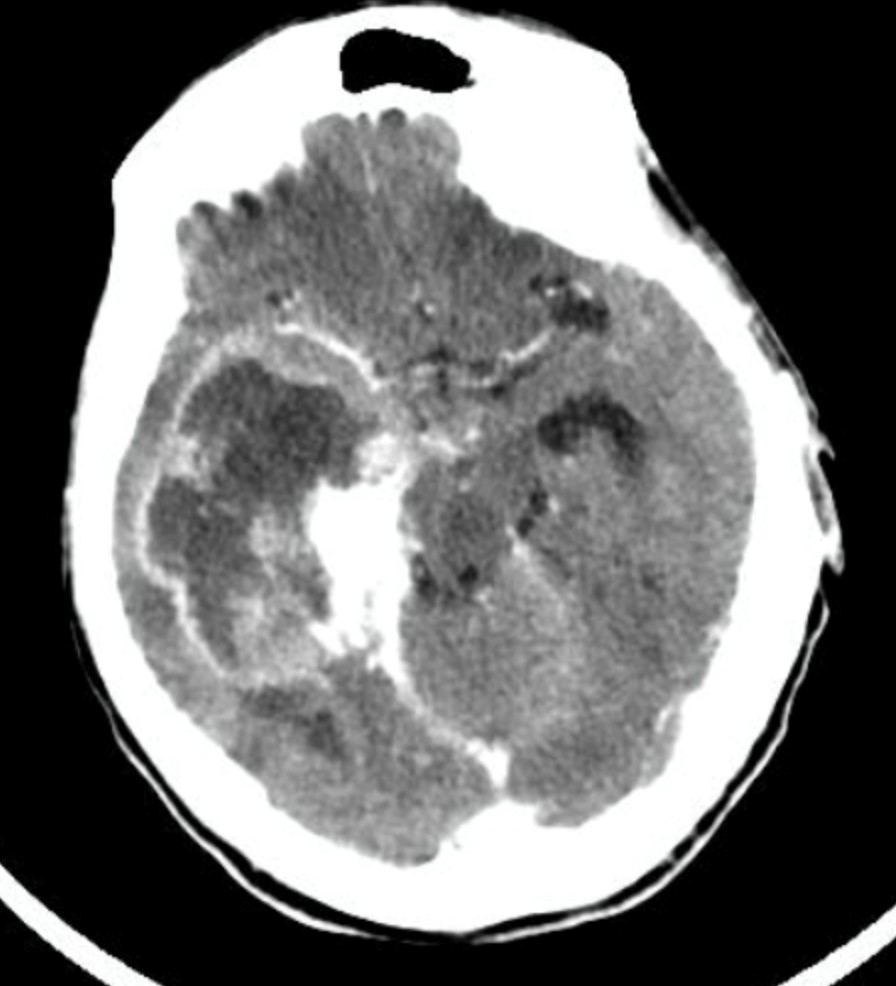
Findings:
There was a large complex mass in the right parietal-occipital region with central low density. There was mild vasogenic edema of the adjacent brain. Subfalcine herniation was noted. There was effacement of the ipsilateral, lateral ventricle and dilation of the contralateral, lateral ventricle. There was a very inhomogeneous pattern of contrast enhancement with prominent rim or ring enhancement seen surrounding the margin of the mass. This was a solitary lesion.
Interpretation:
Brain Tumor with edema and central necrosis.
Diagnosis:
Glioblastoma Multiforme, Biopsy Proven
Discussion:
Gliomas are the most common primary, supratentorial, intra-axial mass in an adult. They account for 30% of brain tumors of all types and 80% of all primary malignant brain tumors.
Glioblastoma multiforme accounts for more than half of all gliomas, astrocytomas about 20%, with the remainder split among ependymoma, oligodendroglioma, and mixed glioma (e.g., oligoastrocytoma).
Glioblastoma multiforme occurs more commonly in males between 65 to 75 years of age, especially in the frontal and temporal lobes.
It has the worst prognosis of all gliomas. It infiltrates adjacent areas of the brain along white matter tracts, making it difficult to resect, but like most brain tumors, it does not produce extra-cerebral metastases.
Imaging findings of a Glioblastoma Multiforme may include:
- As the most aggressive of tumours, glioblastoma multiforme frequently demonstrates necrosis within the tumor.
- The tumour infiltrates the surrounding brain tissue, frequently crossing the white matter tracts of the corpus callosum to the opposite cerebral hemisphere, producing a pattern called a butterfly glioma.
- The tumour is often associated with considerable vasogenic edema, mass effect, and enhances with contrast, at least in part.
Attributions
Figure 6.4A Axial CT of Head, without contrast, displaying a Meningioma by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figure 6.4B Axial CT of Head, with contrast, displaying a Meningioma by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figure 6.5A Axial CT of Head, without contrast, displaying a mass suspicious for malignancy by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figure 6.5B Axial CT of Head, with contrast, displaying contrast enhancement suspicious for a Glioblastoma by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.

