Chapter 3 – Principles of Imaging Techniques
Introduction
Learning Objectives
Knowledge
- Be able to describe the major components of an X-ray unit and explain the process of X-ray generation
- For the following modalities; X-ray, mammography, fluoroscopy, digital subtraction angiography (DSA), CT, Ultrasound, MRI, and Nuclear Medicine, the Student should:
- Be able to describe the physical principles of image formation
- Describe the positioning of the patient for common radiographic techniques (e.g. chest x-ray)
- Recognize factors affecting image quality related to X-ray dose in radiography and fluoroscopy
- Describe the principles of the Doppler effect in ultrasound
- Understand the concepts of spatial, temporal, and contrast resolution
- Describe the Hounsfield Unit (HU) scale and the principle of window level and width
- Relate the contraindications and safety issues for imaging modalities, including the MR environment, with regard to patients and staff
- Explain the basic infrastructure of imaging informatics, including Picture Archiving and Communication Systems (PACS) and Radiology Information Systems (RIS) in the jurisdiction that you work in
Competencies
- Recognize the technological elements displayed when encountering an image (AP chest X-ray, lung level/window for CT, etc.)
- Recognize optimal and sub-optimal image quality in radiography and fluoroscopy
- Identify normal anatomy on radiography, fluoroscopy, DSA, ultrasound, CT, MRI
- Communicate the diagnostic value of imaging modalities for common indications to the patient
- Describe the common processes related to imaging examinations to the patient
- Communicate the risks and benefits of various imaging examinations (including radiography, fluoroscopy, DSA, ultrasonography, CT, MRI, and Nuclear Medicine) to patients and their families
Diagnostic Radiology (Diagnostic Imaging, Medical Imaging, Radiology) is a medical sub-specialty that is overseen by the Royal College of Physicians and Surgeons of Canada and is subject to specialty certification by this organization.
The Diagnostic Radiology Residency is a multi-modality, body system structured, training program that introduces the trainee to all of the major modalities and anatomic regions in preparation for the resident to challenge the national specialty examinations in Diagnostic Radiology, and to have the skills and knowledge to be a knowledgeable general radiologist.
Diagnostic Radiology encompasses a wide variety of modalities, anatomic regions, and clinical conditions. The major imaging modalities that will be discussed in later sections of this chapter, include:
- X-rays (radiographs)
- Mammography
- Fluoroscopy
- Angiography
- Computed Tomography (CT)
- Ultrasound (with Doppler)
- Magnetic Resonance Imaging (MRI)
- Nuclear Medicine (PET/CT)
The first five modalities utilize x-rays generated via an x-ray tube. The mechanical and technical features of the imaging modalities are very different but they all use ionizing radiation administered to the patient from a standardized distance and rely upon the differential absorption of the incident x-rays to create an image.
Ultrasound utilizes high frequency (inaudible) sound while MRI employs magnetic fields and radio waves.
Nuclear Medicine images rely upon the administration of a radioactive pharmaceutical agent that emits alpha, beta, or positron radiation that is captured by external radiation detectors. The anatomic detail of Nuclear Medicine images is very limited but the pharmaceuticals can be designed to concentrate in specific tissues of the body, focusing the bulk of the administered radioactive substance and maximizing the usefulness of the examination, e.g. bone scans are acquired by injecting Technetium 99m (99mTc) bound to diphosphonate. This radio-pharmaceutical is preferentially concentrated in metabolically active bone and maximizes the radiation that is emitted from bone minimizing the background radiation coming from adjacent soft tissues (muscle, fat, etc.).
Resolution of Imaging Modalities
Spatial resolution – This is a measure of the ability of an imaging modality to differentiate objects from each other when the objects are in close proximity. It is also a description of image blur. A standard method of determining the resolution of an x-ray based imaging technology is the line pair detection standard. If lines are created by interposing a radiopaque substance (lead) with a radiolucent substance (air), how many pairs of lines can be distinctly identified per millimeter? CT has a line-pair resolution of 0.7 line-pairs/mm while mammography resolves 7 line-pairs/mm. Image spatial resolution using x-rays can be effected by a wide variety of parameters including some of the following: the incident x-ray dose; the focal spot of the x-ray source; scattering of the incident x-ray beam; the detector array used to detect the transmitted x-rays; and the quality of the viewing monitor.
Spatial resolution of Ultrasound and Magnetic Resonance is more complex due to the physics of these imaging modalities.
Of all the above modalities Nuclear Medicine has the lowest spatial resolution with PET/CT having a resolution of 2 mm.
Contrast resolution – Contrast resolution relates to the viewer’s ability to differentiate between different intensities displayed on an image. The Computed Tomography (CT) Hounsfield Unit (HU) is an absolute contrast density system with the density value of water fixed at 0 HU. Contrast resolution in MRI is not fixed and is highly dependent upon the sequence acquisition parameters established by the operator, hence the phenomenon of black CSF and white CSF on MR on different MRI sequences. MR has the best contrast resolution of all of the common modalities currently utilized.
Temporal resolution – This refers to the duration of image acquisition in reference to an active or dynamic imaging sequence such are gated cardiac CT or MR. i.e. the faster the image can be acquired at the optimal time in the cardiac cycle the better. A general rule is that improvements in temporal resolution have a negative impact upon spatial resolution i.e. if time period for the gathering of transmitted radiation is too short there will be less data to be used to form the imaging for viewing.
Resolution in Imaging
| Term | Definition |
| Spatial Resolution | Measure of the ability to differentiate objects from one another on imaging, when the objects are within close proximity |
| Contrast Resolution | Ability to differentiate between different intensities on an image |
| Temporal Resolution | The precision of a measurement with respect to time |
Table 3.1 Definitions of three resolutions in medical imaging
Patient Safety in Diagnostic Radiology
Radiation exposure
Earlier in this publication there was guidance regarding the current thinking about using radiation wisely, and cautiously, in medicine and the need for not only being aware of the radiation experienced by the patient for a single imaging examination but to be cognizant of the cumulative radiation burden the patient is exposed to during a period of hospitalization, an acute illness, and over their life time. This is particularly important for CT scanning as this modality has expanded in utilization and the cumulative radiation dose for CT has increased markedly over the last 15 – 20 years.
One is again reminded to keep the As Low as Reasonably Achievable (ALARA) x-ray dosing principles in mind, attempt to follow professional society guidelines for imaging, and attempt to employ the “Imaging Wisely” and “Imaging Gently” recommendations in order to provide optimal patient care and minimize radiation exposure.
Workers in the Diagnostic Imaging field are protected from radiation by leaded equipment and clothing (aprons, collars, gloves, shields, and eyeglasses) to minimize their personal radiation exposure during their work. There are annual established limits for radiation exposure that are monitored by personal radiation detectors that workers are required to wear.
Environmental Safety
Equipment – Patients must be supervised and protected from potential injuries related to the equipment used to gather images while in the imaging department. For example, there are no rails on x-ray machines to prevent patients from falling to the floor. Some x-ray examinations require the patient to stand, therefore, imaging protocols must be modified for patients who are dizzy, obtunded, intoxicated, or have a medical condition that prevents them from standing safely. Care and attention must be paid to identifying these individuals and preventing fall related injuries.
Some imaging equipment is heavy and cumbersome and there is potential for inadvertently bumping the patient or crushing digits or limbs while positioning tabletops and mobile equipment.
Some patient become anxious, dizzy, or syncopal and may faint or lose consciousness during procedures that they are unfamiliar with or are causing them pain. Care must be taken to predict these potential complications and protect the patient.
Infection control – Imaging department are a central hub in busy hospitals and clinics and there is a rapid turnover of large numbers of patient through a limited amount of imaging rooms and equipment. Patient may be actively infected or be carriers of infectious disease, some antibiotic resistant. A high degree of cleanliness and appropriate cleaning techniques must be employed to prevent the spread of infections i.e. table tops, ultrasound probes, railings, bathrooms, etc.
Vascular and Interventional Radiology – There are a wide variety of imaging procedures that are invasive and expose the patient to risks of bleeding, infection, cardiovascular collapse, limb ischemia, etc. This area of the department must be staffed and equipped to monitor and manage these patient’s acute medical needs and there must be enough space available in the procedure rooms for medical, radiological, and nursing staff to be present during an acute care situation. Appropriate recovery facilities must be available to monitor this patient group for delayed complications.
Contrast agents – These substances may be administered to alter or enhance an imaging study. They will be discussed in detail in Chapter 4. These substances may cause anaphylactoid type reactions or effect renal function. They may be harmful if injected into extra-vascular and extra-luminal tissues, or spaces. They must be administered by trained physicians or technologists in consultation with the patient’s medical team.
Magnetic fields – Magnetic Resonance Imaging (MRI) relies upon high strength magnetic fields to obtain diagnostic images. These magnetic forces may be dangerous to patients who have implanted medical devices that contain ferromagnetic components such as, cardiac pacemakers, surgical staples, etc. Movement of these ferromagnetic components may cause serious harm or death i.e. metallic aneurysm clip. In addition, medical monitoring devices, stretchers, instruments, etc. may be actively drawn into the magnetic field injuring staff, technologists, patients, or their family members. All individuals entering into the MRI magnetic field must be screened to prevent adverse events related to encounters with the magnet.
Trips, slips, falls, and back injuries – Busy departments are crowded with beds, stretchers, wheelchairs, gurneys, monitoring devices, cords, tubes, etc. All of these are potential sources for patient and healthcare worker injury. Back injuries incurred related to moving ill patients from their stretcher or bed onto the imaging table are common and account for substantial time lost due to leaves for back injuries. Educational programs and adequate lifting apparatus are essential to minimize these types of work related injury.
Patient Safety Considerations:
- Radiation Exposure
- Environmental Exposures
- Equipment (size, weight, handling)
- Infections
- Contrast Agents
- Magnetic Fields (implanted devices, staples, etc.)
- Trips, Slips, Falls, Injuries
Picture Archive and Communication System (PACS)
The patient images, acquired for clinical use, must be identified, stored, and be retrievable for same day and future use. As most images acquired are in the digital format there must be software and hardware solution available to digitally transport, save, and archive images for retrieval and viewing. This is what PACS is designed for. PACS is more often than not a proprietary solution provided to the imaging centre by a large Information Technology (IT) vendor such as Philips, General Electric, Agfa, etc.
The patient images must be stored in a manner that protects the patient’s confidentiality and thus these systems are secured within complex IT networks with stringent security. Qualified members of the healthcare team, with an approved username and password, can access the images for the purpose of engaging in the care of the patient. Access to the PACS is controlled by local IT staff and via secured networks. In order for you to be actively engaged in image utilization you must apply for access to PACS via the IT department of your facility.
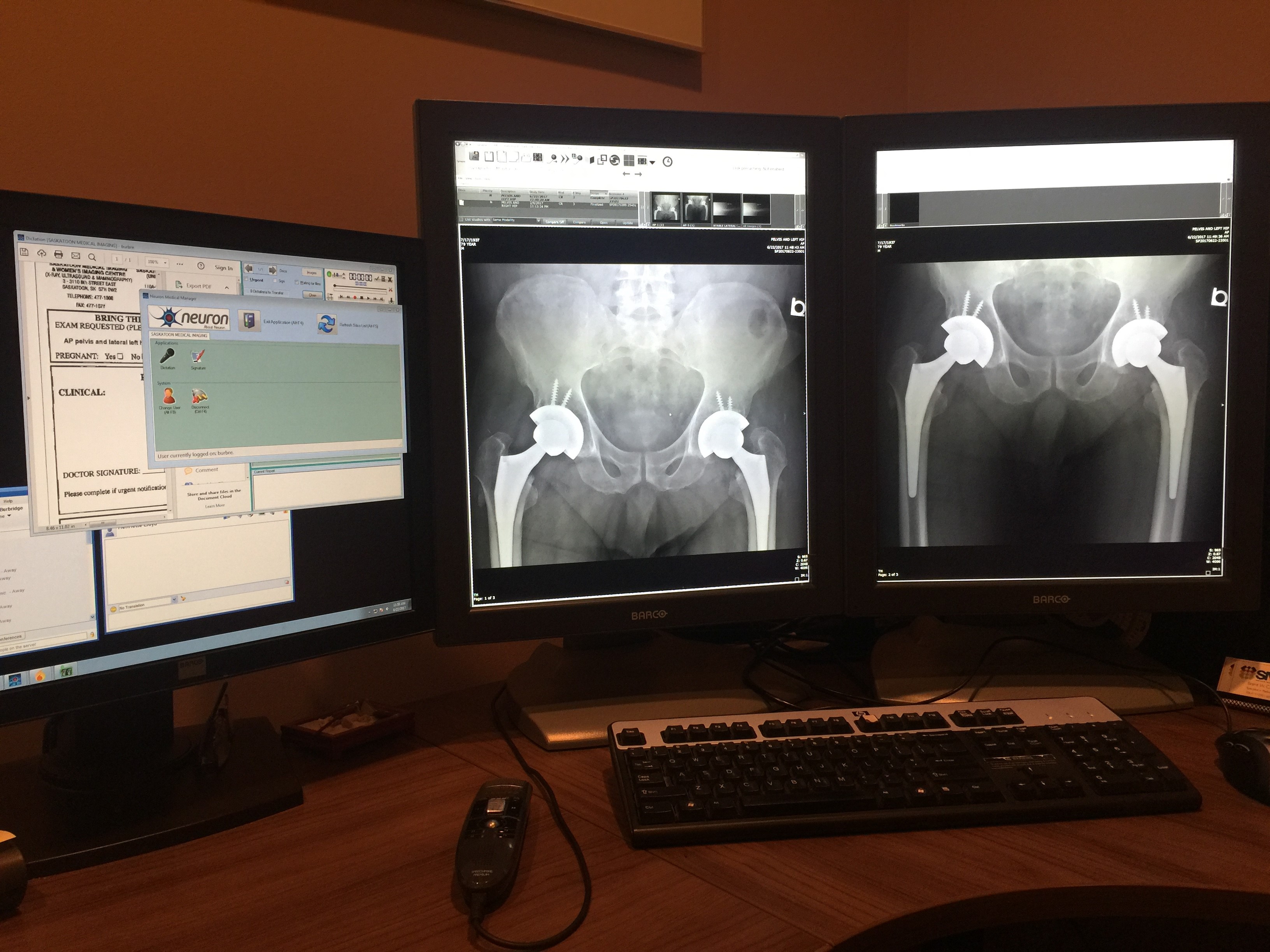
The PACS offers a methodology for searching for patients and their imaging studies. This is usually done using a unique patient identifier such as a hospital number and/or a provincial health number. Thus, one can find new and old imaging studies by searching the PACS database and having them displayed on a PACS compatible viewing station with appropriate monitor resolution for accurate image interpretation. A PACS image review station is depicted in Figure 3.1.
Radiology Information System (RIS)
The software and hardware required to generate requests for patient imaging, schedule imaging studies and reviewing the radiologist interpretation of the imaging studies is usually handled via the RIS. This system is integrally linked to PACS and also requires username and password credentialing to protect patient confidentiality. Clinicians most often use this system to request imaging examinations and to review the reports of previous imaging studies.
Requesting Imaging
The RIS used at your local health care facilities will have a mechanism for requesting imaging examinations. It may be a digital, software driven, online, order entry module that facilitates the requisition of imaging examinations or it may rely upon some other form of communication with the scheduling component of the system e.g. facsimile, hand-written requests, postal service, etc. Most facilities will have established standardized request forms for specific types of procedures i.e. MRI, PET/CT, etc. Figure 3.2 provides an example of a MRI request form.
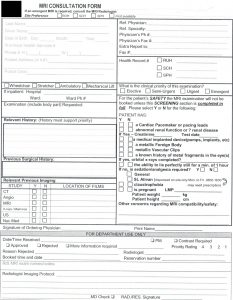
In addition, local imaging facilities will have established policies surrounding the mechanism to be used for requesting elective, urgent, or emergency, imaging studies. Some of the above strategies work well for non-emergent imaging but usually urgent or emergent examinations should be requested by contacting the resident(s), or radiologist(s) on duty for that modality. The identity of the radiologist(s) on duty is known by the hospital switchboard and the Diagnostic Radiology Department.
As a healthcare provider it is your responsibility to ascertain the methods used for requesting imaging studies in your jurisdiction and understand how to contact the appropriate imaging facilities, and personnel, in your area.
Attributions
Fig 3.1 PACS Imaging Viewing Station (Workstation) by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC–BY-NC-SA 4.0 license.
Fig 3.2 Sample MRI Request Form by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC–BY-NC-SA 4.0 license.

