Chapter 8 – Cardiovascular
Congestive Heart Failure
ACR – Dyspnea – Suspected Cardiac Origin
Case
Congestive Heart Failure
Clinical:
History: This 69 year old female patient was receiving medication for hypertension. No other medications. No previous problems with shortness of breath.
Symptoms: The patient reported progressively worsening exercise intolerance that usually ends with shortness of breath. Walking a block makes her very short of breath. No chest pain reported. The patient sleeps with two pillows as she finds that she wakes up short of breath otherwise. She has mild, ankle, pitting edema.
Signs: The patient had good color and was not cyanotic. The jugular veins in her neck were prominent when lying flat. Auscultation revealed mild rhonchi. She had pitting edema from the feet to the knees, bilaterally. No other findings.
Laboratory:
The hemoglobin was minimally decreased and there was evidence of microcytic anemia. Nil else.
DDx:
Dyspnea of possible cardiac origin.
Imaging Recommendation
ACR – Dyspnea – Suspected Cardiac Origin
Chest X-ray
ODIN Link Congestive Heart Failure images, Figure 8.7A and B: https://mistr.usask.ca/odin/?caseID=20160318160706756

Imaging Assessment
Chest x-ray:
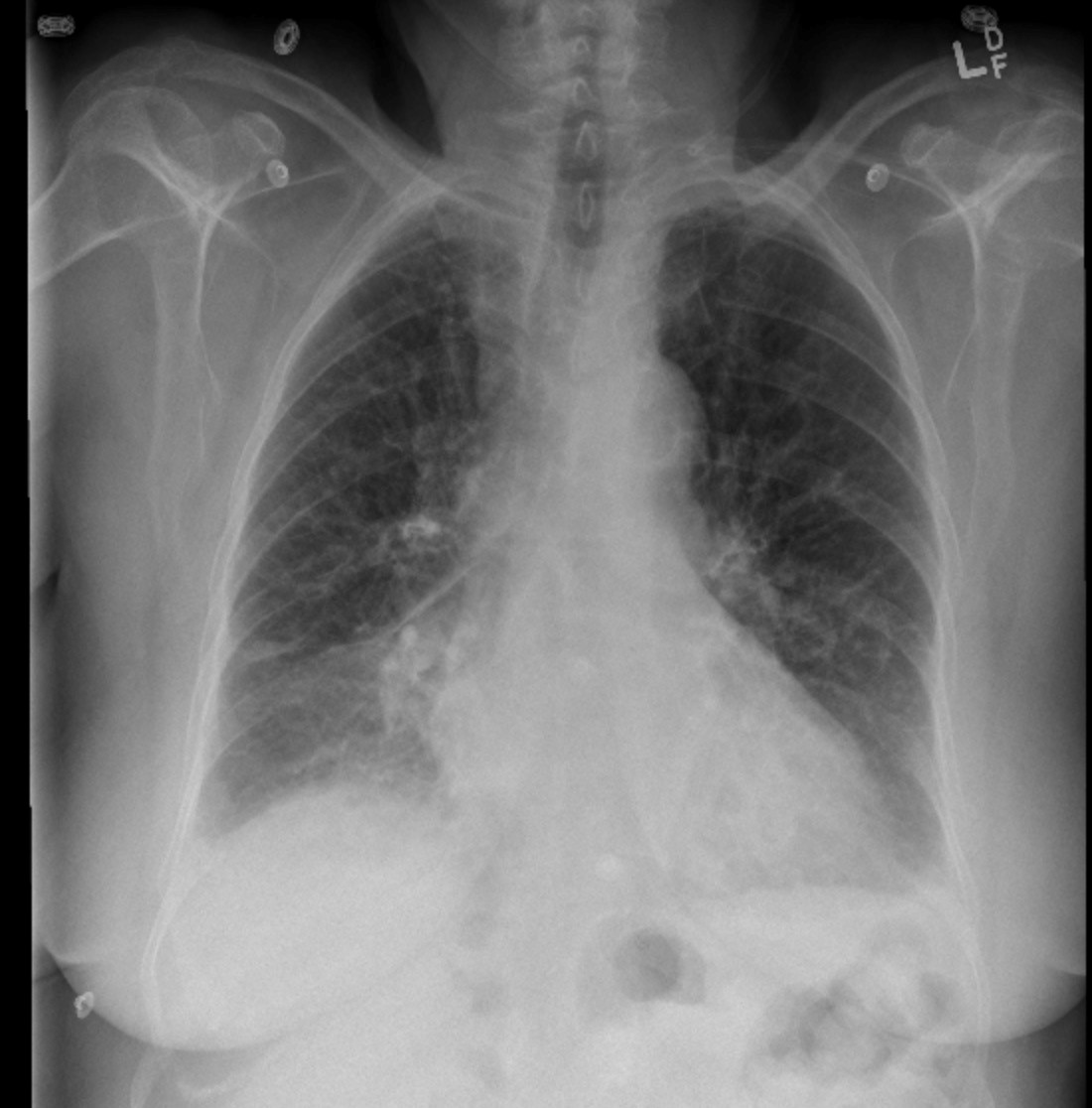
Findings:
The cardiac silhouette was enlarged. There was bronchial wall cuffing and prominence of the upper lobe vessels consistent with vascular redistribution and interstitial edema. The lower lobe vessels were also partially obscured due to the interstitial edema and possibly mild alveolar edema. Subpleural edema resulted in prominence of the lung fissures. Small-moderate, bilateral, pleural effusions were seen.
Interpretation:
Cardiac silhouette enlargement with secondary findings of Congestive Heart Failure.
Diagnosis:
Congestive Heart Failure
Discussion:
Causes:
- Ischemic heart disease
- Hypertension
- Cardiomyopathy
- Cardiac valvular lesions, such as aortic stenosis and mitral stenosis
- Arrhythmia
- Thyrotoxicosis
- Severe anemia
- Left-to-right shunt
The changes of congestive heart failure are progressive when myocardial functionality is impaired. The early changes occur in the interstitial tissues but spread to the alveolar space and the pleural space.
Pathophysiology:
The myocardium is incapable of ejecting sufficient blood to keep up with the demands of the body for oxygenated blood. Starling’s equation becomes altered and there is often a pressure imbalance that results, creating back pressure into the pulmonary circulation. This may be due to hypertension and increased afterload or myocardial damage from ischemia, or cardiomyopathy.
X-ray findings may include:
- Thickened interlobular lung septa (Kerley lines)
- Pulmonary vascular re-distribution (upper lobe vessel enlargement)
- Peri-hilar haziness
- Bronchial wall cuffing (thickening)
- Subfissural edema
- Pleural effusions
- Alveolar edema
Attributions
Figure 8.7A PA Chest x-ray displaying CHF by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC–BY-NC-SA 4.0 license.
Figure 8.7B Lateral Chest x-ray displaying CHF by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.

