Chapter 9 – Chest
Pneumothorax
ACR – Chest – Acute Respiratory Illness in Immunocompetent Patient
Clinical:
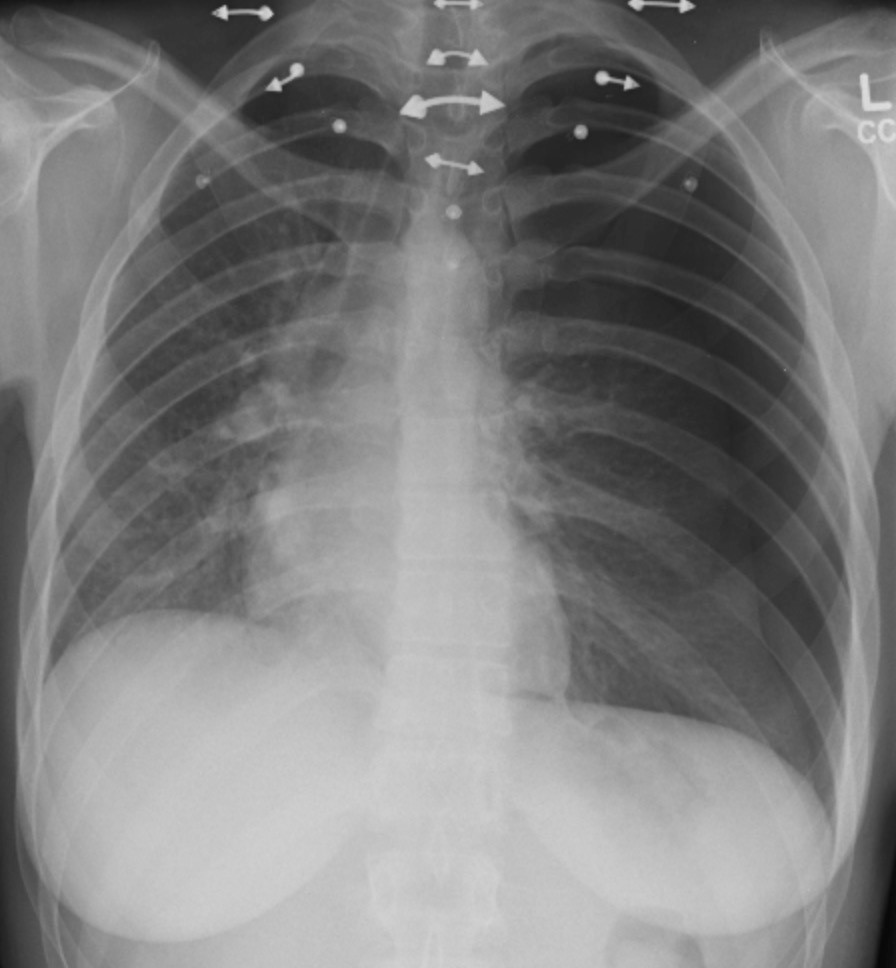
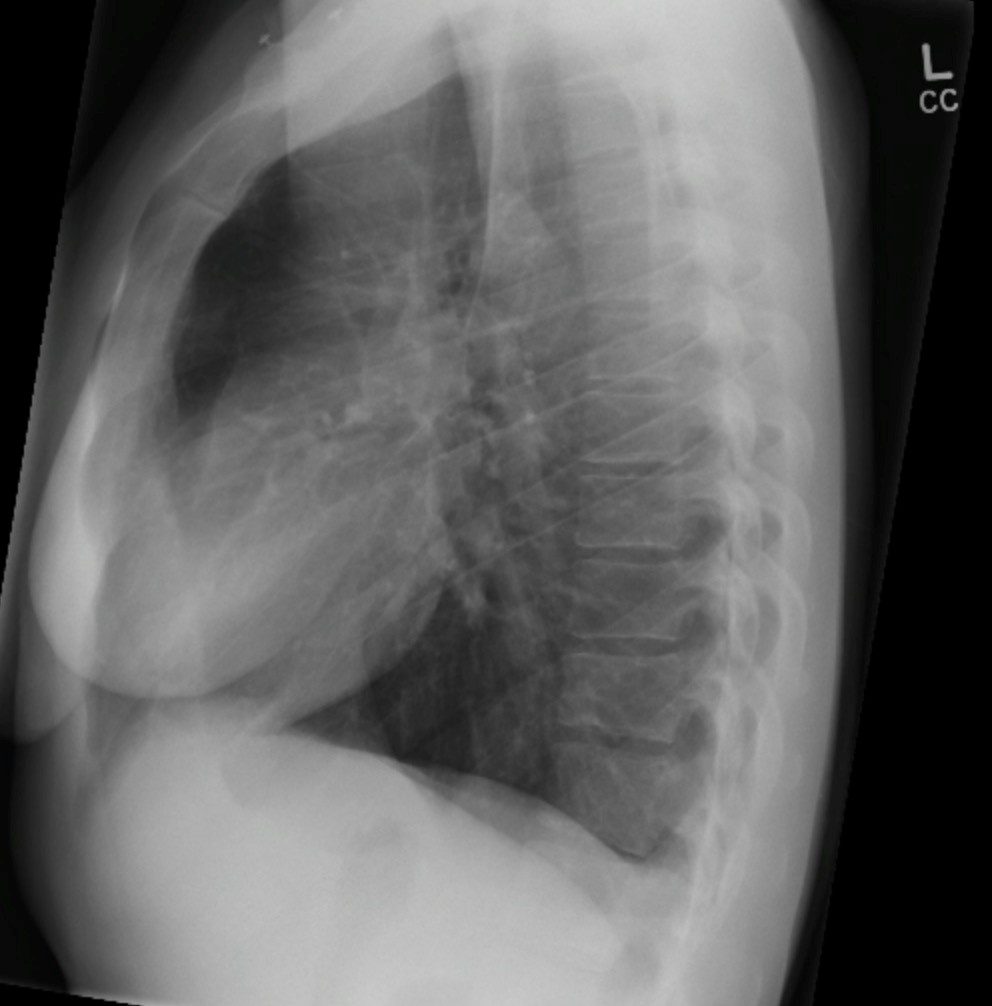
History – This 51 year old male had mild shortness of breath after a failed, left, subclavian venous catheter insertion. Ultrasound had not been used for attempted venous access.
Symptoms – Mild shortness of breath.
Physical – He had muffled, to absent, breath sounds on the left.
Diagnosis – Iatrogenic pneumothorax related to a failed venous catheter insertion.
DDx:
Pneumothorax
Atypical Pneumonia
Hemothorax
Imaging Recommendation
ACR – Chest – Acute Respiratory Illness in Immunocompetent Patient, Variant 4
Chest X-ray
Case 1
Pneumothorax – Small Left


Image Assessment
Findings:
The left lung was mildly hyperinflated. There was a visible pleural line in the apex of the left hemithorax. This line was convex outward. There were no visible lung markings beyond this pleural line.
Diagnosis:
Small left pneumothorax
Discussion:
Pneumothorax may be associated with trauma, a recent medical procedure, mechanical lung ventilation, or may occur spontaneously. Typically, air leaks out of the lung due to puncture, tear, or rupture in the visceral pleura. This air accumulates between the two pleural layers. Less commonly, there is an open wound in the chest wall that allows air to enter the pleural space.
Most pneumothoraces are caused by trauma. Lung injury may be caused by a projectile (low velocity – knife or high velocity – bullet). Alternatively, the chest wall is injured causing fractures of ribs that lacerate the pleura. Trauma can also cause a tear of the bronchus or lung leading to a pneumothorax.
Small pneumothoraces are often asymptomatic, but as they enlarge the patient may become short of breath and develop pleural pain. There may be distant breath sounds and less often an audible pleural rub.
X-ray findings may include:
- Ipsilateral hemithorax may be more lucent.
- The visceral pleura may be seen as a visible white line with lucency beyond this.
- This pleural line is convex outward.
- There are no visible lung markings beyond the pleural line.
- The ipsilateral lung may demonstrate atelectasis as the lung collapses.
- If an air/fluid level is seen in the pleural space due to bleeding, infection, chyle, or transudate this is a clue to the presence of pneumothorax as air rises to create the air/fluid level.
- If the pneumothorax becomes larger it may push the mediastinum into the contralateral hemithorax (tension pneumothorax).
- On a supine radiograph the costophrenic angle may become deeper and be more prominent. Also, the cardiac margin may become more distinct as air rises up ventrally.
Case 2
Pneumothorax – Moderate (right)
Clinical:
History – This 6 month old patient had been resuscitated for an acute respiratory arrest on the ward. He had been ventilated by a face mask and CPR had been performed. A chest x-ray was requested after resuscitation.
Symptoms – Shortness of breath.
Physical – He had muffled, to absent, breath sounds on the right.
Diagnosis – Pneumothorax, post-resuscitation.
Imaging Recommendation
ACR – Chest – Acute Respiratory Illness in Immunocompetent Patient, Variant 4
Chest X-ray

Image Assessment
Findings:
There was a visible pleural line in the right hemithorax. This line is convex outward. There was a small pleural effusion on the left seen in the apex of the chest due to the supine position.
Diagnosis:
Moderate right pneumothorax. Probably related to baro-trauma during resuscitation.
Case 3
Pneumothorax – Tracheal Deviation – Tension (left)
Clinical:
History – This 36 year old female had left chest pain and shortness of breath after a piercing (body adornment) was inserted into the left anterior chest wall.
Symptoms – Shortness of breath. Left chest pain. Anxiety.
Physical – She had muffled, to absent, breath sounds on the left. The trachea was markedly deviated to the right. The patient was in distress.
Diagnosis – Tension pneumothorax, caused by a piercing traversing the parietal and visceral pleural, lacerating the underlying lung.
Imaging Recommendation
ACR – Chest – Acute Respiratory Illness in Immunocompetent Patient, Variant 4
Chest X-ray
Attributions
Figure 9.19A AP Chest x-ray, Pneumothorax, Small by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figure 9.19B Lateral Chest x-ray, Pneumothorax, Small by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figure 9.20 PA Chest x-ray, Pneumothorax, Moderate by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figure 9.21A AP Chest x-ray, Pneumothorax, Tension by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figure 9.21B Lateral Chest x-ray, Pneumothorax, Tension by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.

