Chapter 15 – Pediatric
Non-Accidental and Accidental Trauma
ACR – Pediatric – Suspected Physical Abuse
Case 1
Non-Accidental Trauma
Imaging Recommendation
Clinical:
History – This 2 year old child was brought to ER for lethargy and failure to thrive.
Symptoms – None
Physical – The child was undernourished and looked unwell. The child was lethargic and irritable. There were multiple painful bones and joints, especially the knees. There were multiple bruises and abrasions, including bruises on the face. The back of the head was swollen and tender.
DDx:
Suspected non-accidental trauma
Imaging Recommendation
ACR – Pediatric – Suspected Physical Abuse, Variant 3
Skeletal survey (x-rays)
CT Head

Imaging Assessment
X-Rays
Findings:
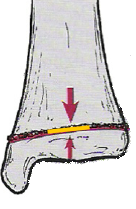
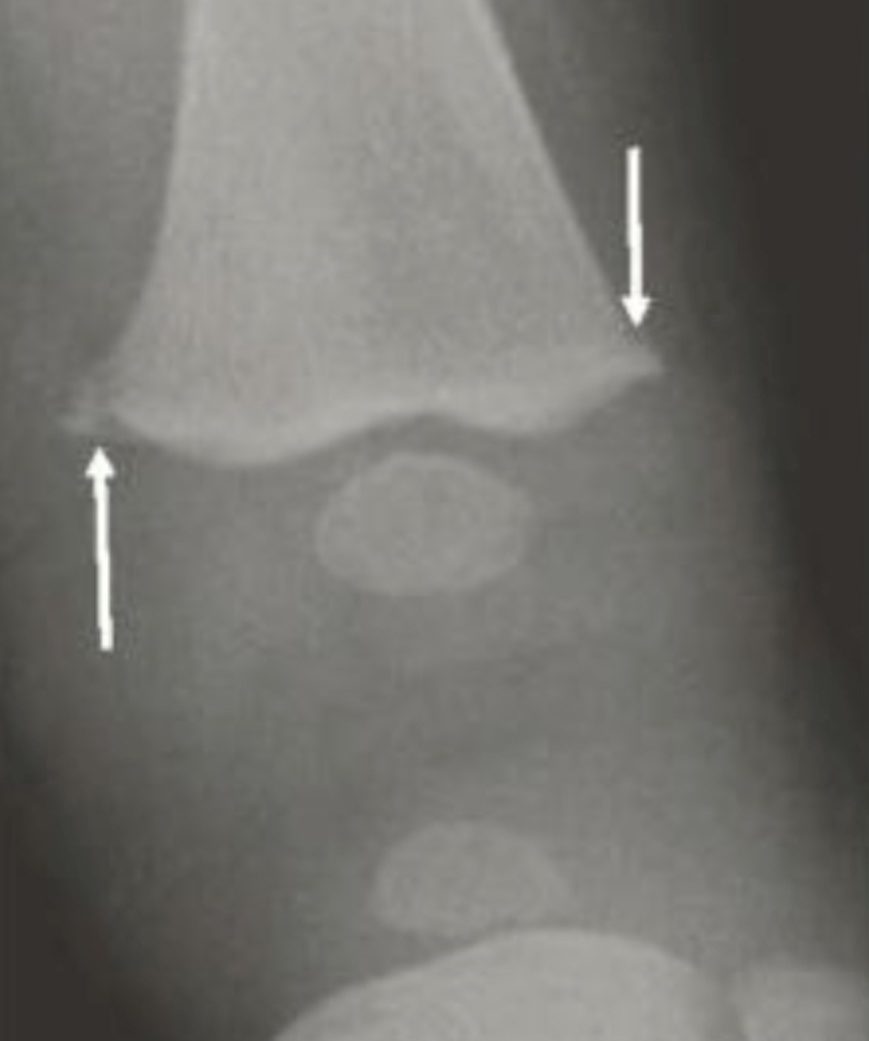
Limited x-rays were initially performed. There were classical, metaphyseal, bucket handle type fractures. This was also seen involving the distal tibia.
Interpretation:
High suspicion for non-accidental trauma. Full skeletal survey recommended.
Computed Tomography
Findings:
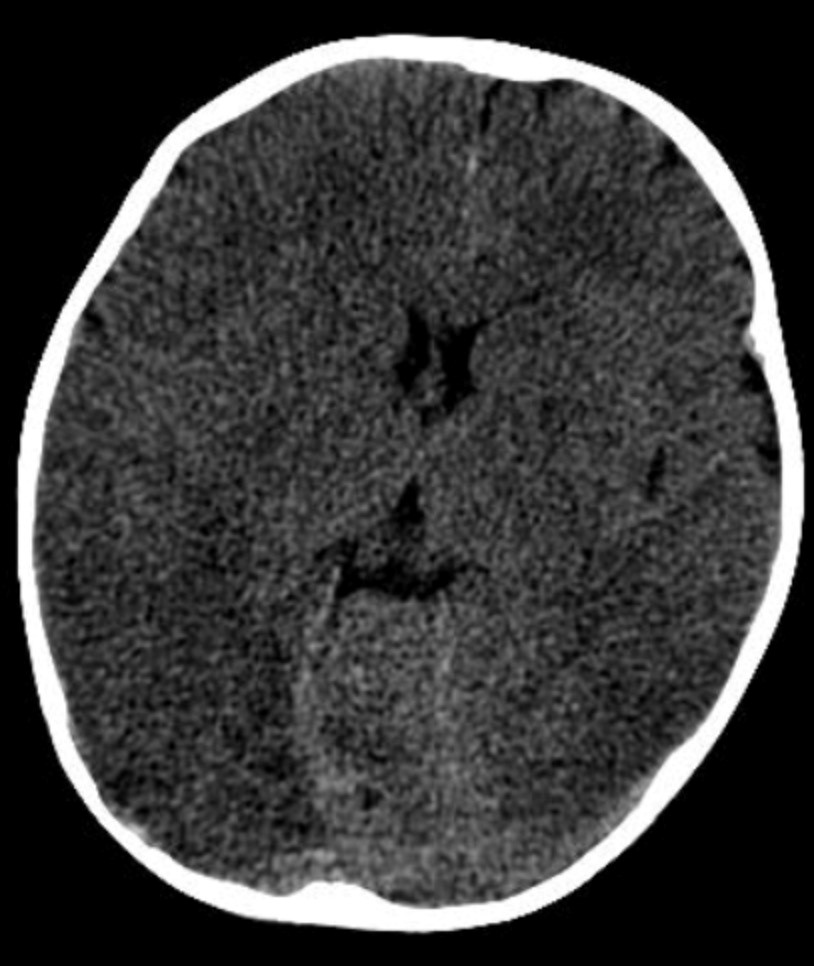
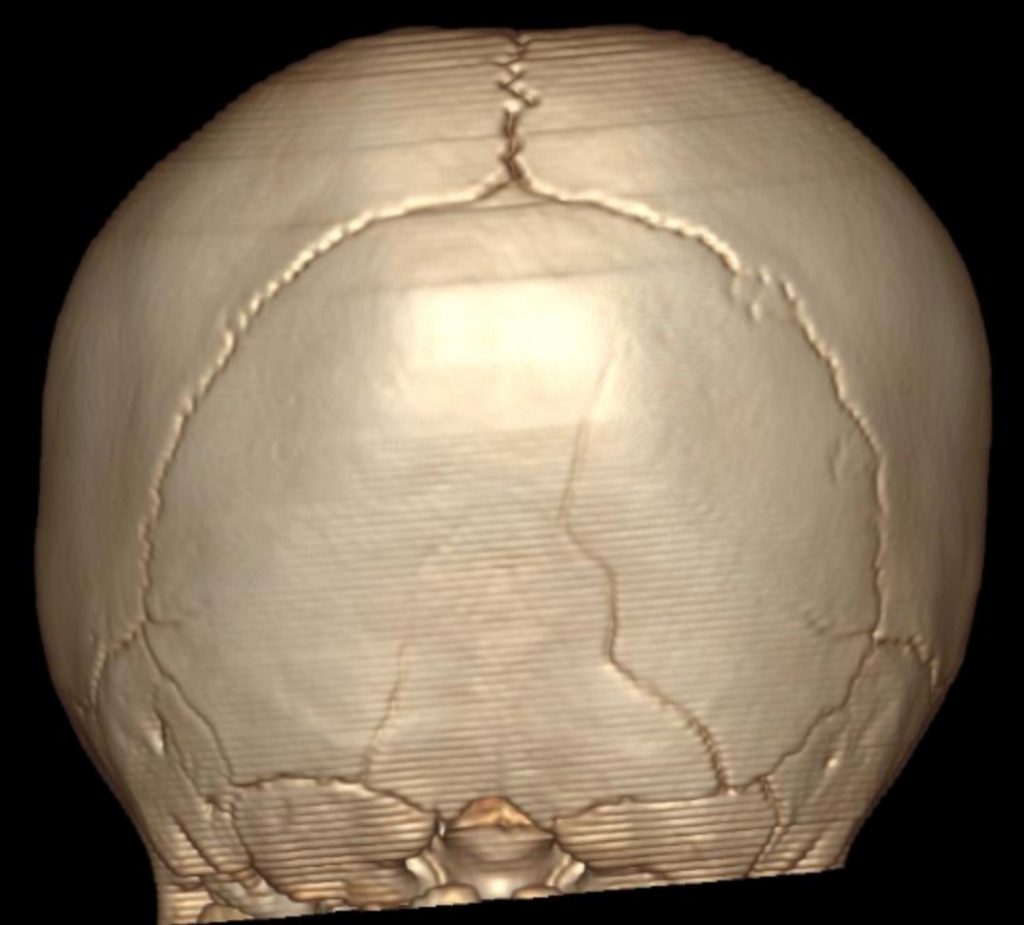
There was generalized cerebral edema. A small subdural hematoma was seen in the right frontal region. Occipital bone fractures were present.
Interpretation:
Probable shaken child syndrome. Non-accidental trauma.
Diagnosis:
Non-accidental trauma
Discussion:
Physically abused children may present with neurological injuries, hollow viscus and solid-organ injuries, superficial and deep soft-tissue injuries, thermal injuries, and/or fractures. Fractures highly suggestive of physical abuse include rib fractures, classic metaphyseal lesions, those unsuspected or inconsistent with the history or age of the child, multiple fractures involving more than one skeletal area, and fractures of differing ages.
In some children, physical examination and history may clearly indicate that physical abuse has occurred. In other children, however, the diagnosis of abuse is not so straight forward and requires clinical, laboratory, imaging, pathological, and forensic evaluation and usually relies on the findings of a multidisciplinary team that includes physicians, social workers, and legal authorities.
Imaging often plays a major role in the detection and documentation of physical injury. The type and extent of imaging performed in a child who is a suspected victim of abuse depends on the child’s age, signs, symptoms, and other social considerations, such as being the twin or sibling of a physically abused infant. Making the diagnosis of child abuse requires differentiation from anatomical and developmental variants and possible underlying metabolic and genetic conditions.
Recommended Imaging:
Skeletal survey:
The radiographic skeletal survey is the primary imaging examination for detecting fractures. The skeletal survey should be composed of frontal and lateral views of the skull, lateral views of the cervical spine and thoraco-lumbo-sacral spine, and single frontal views of the long bones, hands, feet, chest, and abdomen. Oblique views of the ribs should be obtained to increase the accuracy of diagnosing rib fractures, which are strong positive predictors and may be the only skeletal manifestation of abuse.
The images should be obtained using high-detail imaging systems and coned to the specific area of interest for each of the body parts, with separate views of each arm, forearm, thigh, leg, hand, and foot to improve image quality and diagnostic accuracy.
Fractures most often involve the long bones and ribs, with lesser involvement of the skull and clavicles and even less frequent involvement of the pelvis, spine, hands, and feet. It has therefore been questioned whether the radiation exposure outweighs the potential benefit of imaging the pelvis, spine, hands, and feet on initial skeletal survey.
CT Head without contrast:
Unenhanced computed tomography (CT) of the head is the examination of choice to evaluate children with suspected abusive head trauma (AHT). These include children who had skeletal survey for suspected child abuse, children with neurological changes, and children with facial injuries raising concern for abuse. Multi-planar reformations and 3-D volume rendering of the skull increase sensitivity for fracture and intracranial hemorrhage.
Imaging findings may include:
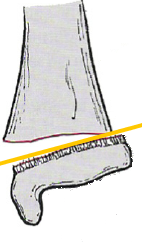
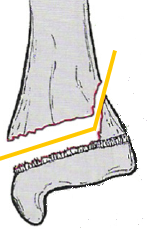
- Metaphyseal corner fractures – small, avulsion-type fractures of the metaphysis, caused by rapid rotation of ligamentous insertions; corner fractures are considered diagnostic of physical abuse. They parallel the metaphysis and can have a bucket-handle appearance.
- Rib fractures,especially multiple fractures, and/or fractures of the posterior ribs (which rarely fracture, even by accidental trauma).
- Head injuries are the most common cause of death in child abuse under the age of two years. Findings include subdural and subarachnoid hemorrhage and cerebral contusions.
- Skull fractures tend to be comminuted, bilateral, and may cross suture lines.
Case 2
Skeletal trauma – growth plate injury
Salter – Harris Skeletal Injuries
Clinical:
History – Injured her knee ski-doing.
Symptoms – Painful knee.
Physical – The patient was limping and reluctantly put weight on the leg. Minimal knee swelling was seen and there was some minimal bruising present.
DDx:
Contusion
Femur fracture
Tibial fracture
Imaging Recommendation
X-rays


Imaging Assessment
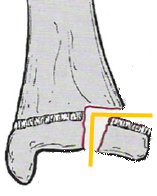
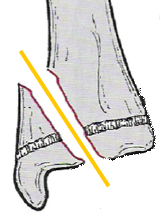
Findings: The femoral growth plate was widened. There was a metaphyseal fracture that exited laterally. Minimal swelling was noted.
Interpretation:
Salter-Harris type 2 fracture of the distal femur.
Diagnosis:
Salter-Harris, type 2, fracture
Discussion:
- The epiphyseal plate (physis or growth plate) is the weakest part of the bone and is prone to shearing injuries.
- The Salter-Harris classification is a means of categorizing epiphyseal plate fractures and provides clues to their prognosis.
- All such fractures, by definition, involve or extend through the epiphyseal plate and therefore all such fractures occur in children before the epiphyseal plate fuses.
Salter-Harris, type II fracture:
- Most common Salter-Harris fracture—85%.
- Involves both the epiphyseal plate and the metaphysis.
- A corner of metaphysis that is usually fractured produces the “corner sign”.
- Rarely produces complications.
Salter-Harris Classification of Growth Plate Injuries (Description, Frequency, and Prognosis):
Table 15.1 Description, frequency, and prognosis of Salter-Harris Classification of Growth Plate Injuries by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Attributions
Figure 15.1A X-ray of pediatric fractures associated with non-accidental trauma by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figure 15.1B X-ray of pediatric fracture associated with non-accidental trauma by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figure 15.2A CT scan of the head and brain revealing brain infarction and edema by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figure 15.2B 3D rendering of the skull demonstrating skull fractures in a child by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figure 15.3A X-ray of the pediatric knee revealing a distal femoral fracture by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figure 15.3B Lateral x-ray of the knee associated with a femoral fracture by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.