Chapter 8 – Cardiovascular
Aortic Dissection and Aneurysm
ACR – Acute Chest Pain – Suspected Aortic Dissection
Case
Type B Aortic Dissection and Aneurysm
Clinical:
History – The patient reported the sudden onset of a “tearing” pain in his chest that began about one hour ago. It was still present and he rated the pain as 7/10 in severity.
Symptoms: “Tearing” chest pain. Persistent, radiating between his shoulder blades.
Signs: Tachycardia. No murmur detected. No blood pressure disparity detected.
DDx:
Aortic Dissection
Aortic Aneurysm
Myocardial Infarction
Pulmonary Embolism
Imaging Recommendation
ACR Recommendations for Acute Chest Pain – Suspected Aortic Dissection
Chest X-ray
Followed by Contrast Enhanced CT of the Chest, Abdomen and Pelvis, if warranted
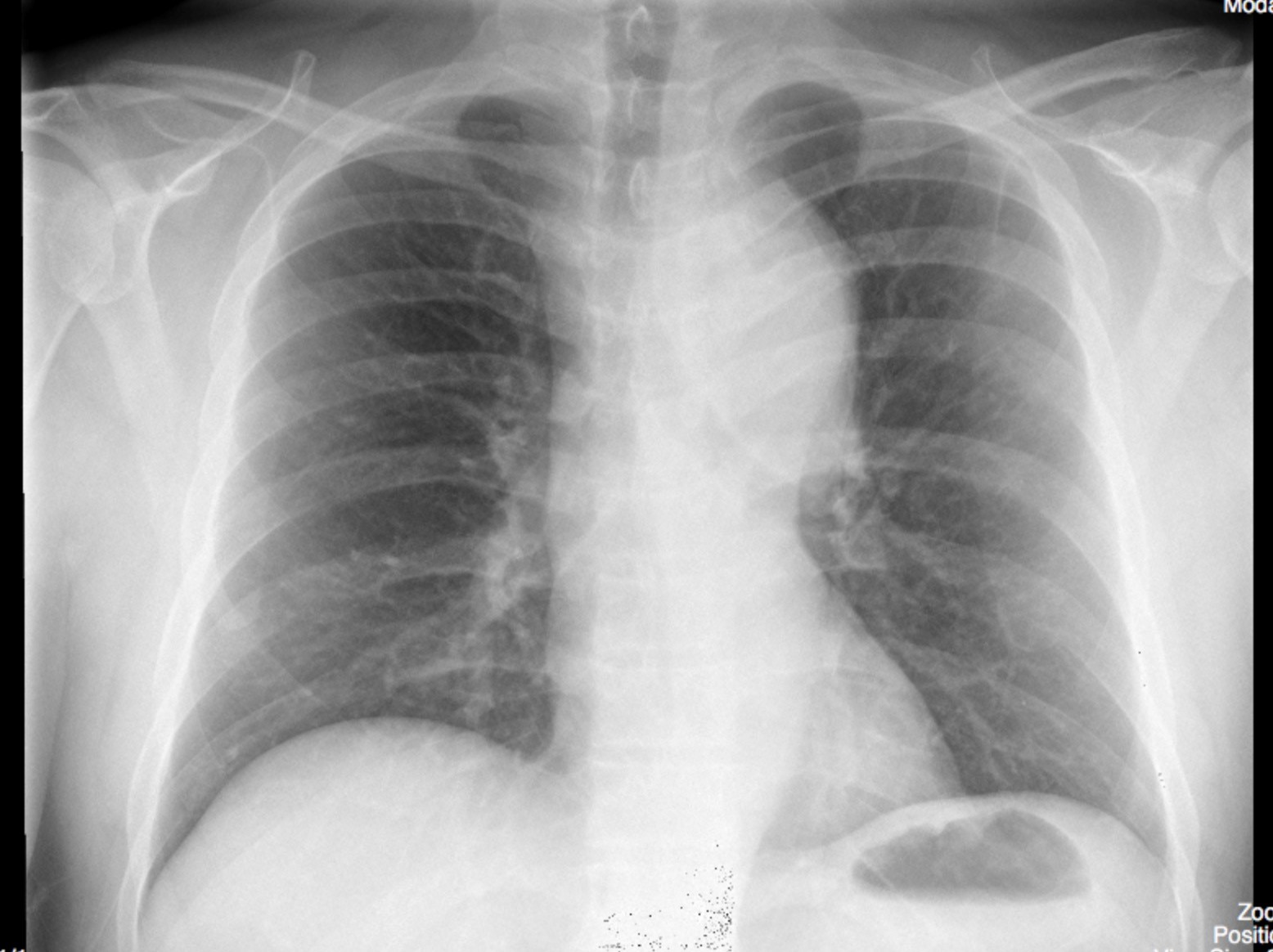
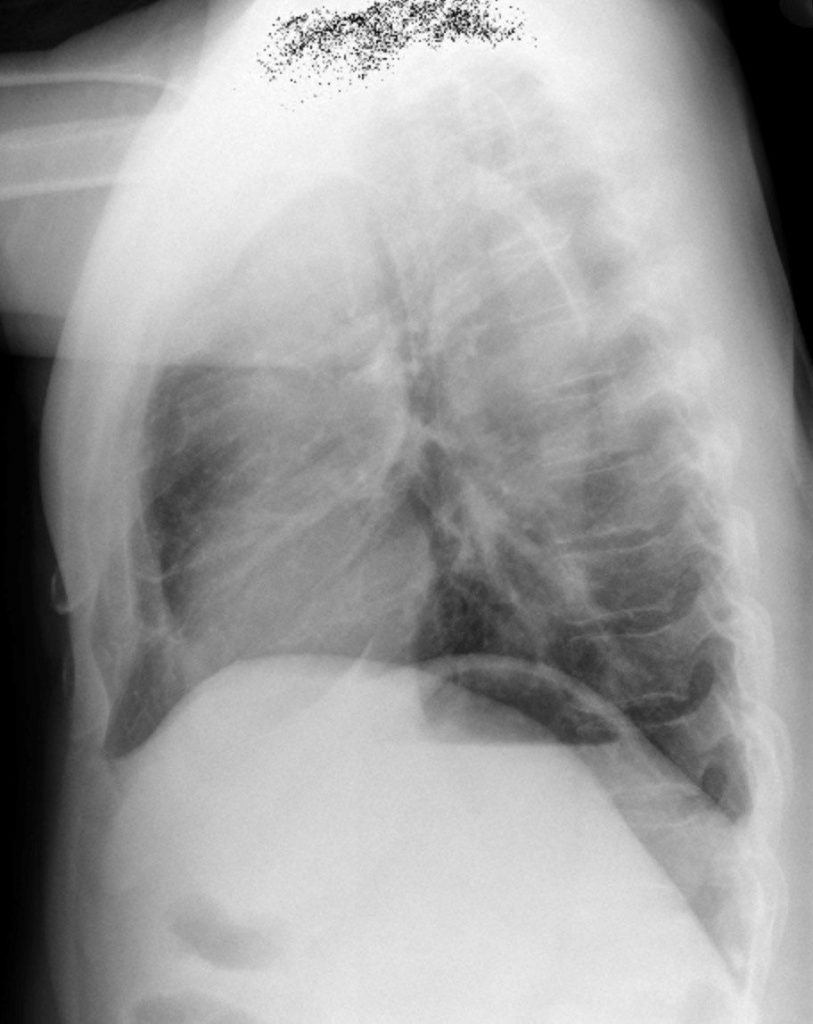
ODIN Link for Enlarged Aorta, Chest x-ray, Figure 8.4A and B: https://mistr.usask.ca/odin/?caseID=20170414181501895
Imaging Assessment
Chest x-ray
Findings:
There was a left, apical, pleural cap. The upper mediastinum was widened. The aortic knob was very enlarged and had displaced the trachea to the right. The cardiac silhouette was not enlarged. The lungs were clear.
Interpretation:
The findings suggest aortic enlargement with the apical pleural cap due to secondary mediastinal hematoma. Given the history, the possibility of an aortic dissection, causing the aortic enlargement, must also be considered.
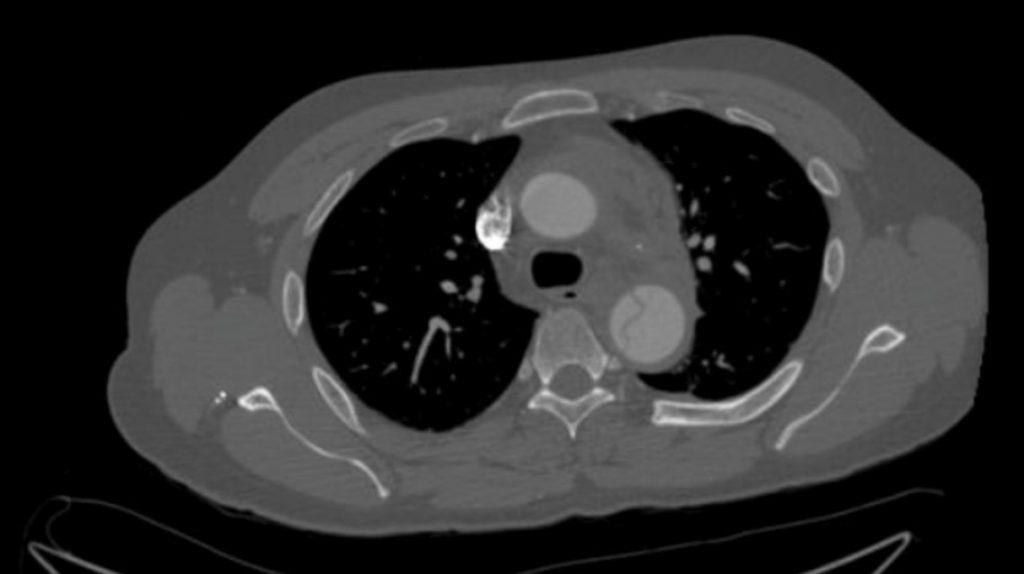
CT
Findings:
Contrast enhancement was visualized in the arterial phase. There was a thin, linear, filling defect in the aorta that originates just distal to the subclavian artery. This linear defect was present to just cranial of the celiac axis and then became non-visible. There was a false lumen in the medial aorta related to the linear filling defect. The findings were consistent with an aortic wall intimal flap and associated dissection that originates just distal to the subclavian artery.
Additionally, there was a small protuberance of the aorta on the lateral aortic knob which was associated with mediastinal hematoma. This may well represent a pseudoaneurysm related to the dissection. No other significant findings.
Interpretation:
Type B aortic dissection with a secondary aneurysm and pseudoaneurysm with mediastinal hematoma.
Diagnosis:
Type B Aortic Dissection
Discussion:
A tear in the aorta between the intima and the media allows blood to dissect the wall for varying lengths of the aorta, usually between the intima and media at the site of the tear but the pulsatile blood then usually dissects into the media at the junction of the inner 1/3 and the middle 1/3. The dissection may rarely perforate the media and enter in to the adventitia, possibly resulting in pseudoaneurysm formation. In general, patients with aortic dissection most commonly are hypertensive, but they may have an underlying condition that can predispose to dissection, i.e.:
- Cystic medial degeneration
- Atherosclerosis
- Marfan syndrome
- Ehlers-Danlos syndrome
- Trauma
- Syphilis
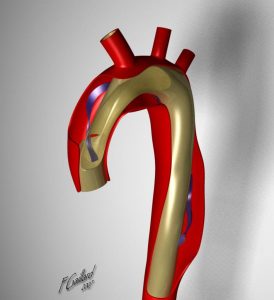
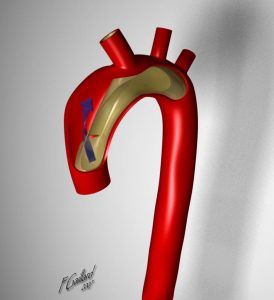
Aortic dissection most often originates in the ascending aorta (Stanford type A)(DeBakey II), extending into the descending aorta (Stanford A)(DeBakey I), or they may only involve the descending aorta (Stanford type B)(DeBakey III).
 |
 |
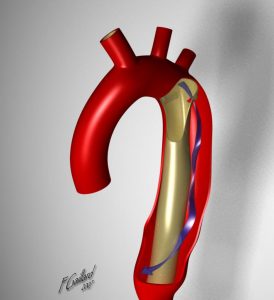 |
| DeBakey I | DeBakey II | DeBakey III |
| Stanford A | Stanford A | Stanford B |
Table 8.1 Classification of Aortic Dissection
Conventional radiographs are not diagnostically reliable, but they may point to the diagnosis when several imaging findings occur together, especially in the proper clinical setting.
Aortic Aneurysm
An aneurysm represents a region of the aorta that is larger than normal size by more than 1.5x. If the aneurysm has all three layers of the arterial wall it is a true aneurysm. It may be concentric (fusiform) or eccentric (saccular) in shape. The aneurysm may be partially calcified and may contain thrombus in some cases. If the aneurysm lacks all three layers of the aorta it is a false or pseudo-aneurysm. Pseudo-aneurysms for the most part represent a tear of the aortic wall with the resulting hematoma contained by the adjacent soft tissues.
The most common cause of aneurysms are atherosclerosis and hypertension. Some are associated with syndromes and other conditions such as Marfan syndrome or syphilis. Dissections of the aorta may also present with imaging findings of aneurysm.
When aneurysms reach a certain diameter they are more prone to rupture. For example, an abdominal aortic aneurysm larger than 5 cm in diameter has an annual risk of rupture of roughly 10%. This increases to an annual risk of 25% for abdominal aortic aneurysms larger than 6 cm in diameter. Imaging plays a major role in the detection, characterization, and follow-up of aortic aneuryms.
X-ray findings of Dissection may include:
- “Widening of the mediastinum” – this has low sensitivity as it is often difficult to diagnose on portable, supine radiographs and it is present in only 20 – 25% of those with dissection.
- Double aortic knob
- Irregular aortic knob
- Left pleural effusion due to a hemothorax.
- Displacement of intimal calcification (1cm or >) is possible. Comparison to previous x-rays may help to determine if this sign is present.
Dissection Classification
Dissection in Ascending Aorta Only; known as:
- Standford Type A
- DeBakey II
Dissection in Ascending and Descending Aorta; known as:
- Standford Type A
- DeBakey I
Dissection in Descending Aorta Only; known as:
- Standford Type B
- DeBakey III
Attributions
Figure 8.4A Chest x-ray: AP, enlarged aortic knob by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figure 8.4B Chest x-ray: Lateral, enlarged ascending and arch aorta by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figure 8.5 Contrast enhanced Computed Tomography of the Chest, Abdomen and Pelvis, intimal flap seen associated with aortic dissection by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figures in Table 8.1: DeBakey I, DeBakey II, and DeBakey III, courtesy of Dr Yuranga Weerakkody and A.Prof Frank Gaillard, Radiopaedia https://radiopaedia.org/articles/aortic-dissection and were originally published under a CC-BY-NC-SA 3.0 license.

