Chapter 6 – Brain and Spine
Spine Fracture
ACR – Neurologic – Low Back Pain, Variant 2
Case
T12, ventral, vertebral, compression fracture
Clinical:
History – This 65 year old female experienced severe low back pain after jumping down from the back of a pick-up truck.
Symptoms – Upper, low back pain.
Physical – Bent forward due to back pain. Pain ranked as severe, 7 – 8/10. Range of motion of the spine was very diminished. No neurological symptoms or red flags.
DDx:
Disc herniation
Muscle spasms
Vertebral compression fracture
Imaging Recommendation
ACR – Neurologic – Low Back Pain, Variant 9
Advanced imaging with CT or MR of the spine, neurologic symptoms favour obtaining MR
X-rays are useful for screening and localization

Imaging Assessment
Findings:
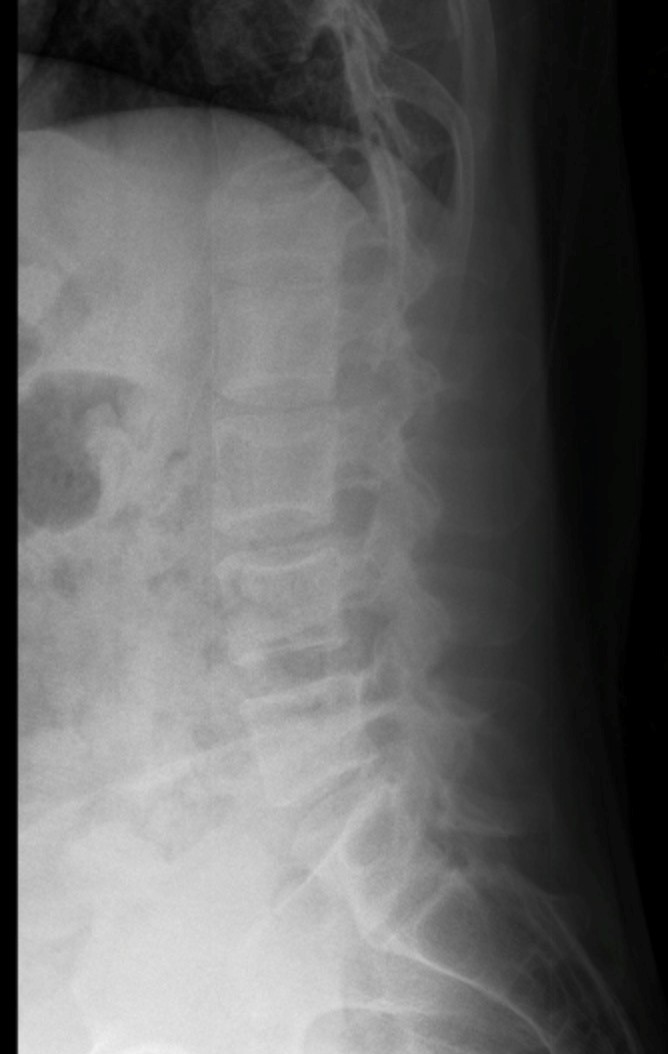
There was a ventral, cranial, end plate, fracture of the T12 vertebral body. This was a mild compression fracture. There was minimal osteopenia of the bones. Nil else.
CT imaging did not reveal any suspicious skeletal lesions.
Interpretation:
Minor compression fracture. Probably osteoporotic.
Advanced spine imaging (CT or MR) can help to rule out malignancy, or infection, if there is clinical concern.
Diagnosis:
T12, ventral, vertebral compression fracture
Discussion:
Vertebral compression fractures can be caused by osteoporosis, direct acute trauma in an otherwise healthy vertebra, and neoplasms. Neoplasms causing vertebral compression fractures include: 1) primary bone neoplasms (hemangiomas, giant cell tumors), 2) infiltrative neoplasms (multiple myeloma, lymphoma), and 3) metastatic neoplasms. Osteoporotic vertebral compression fractures are the most commonly encountered fractures that require surgical and medical treatment and are the focus of this narrative.
Postmenopausal women represent the majority of patients at risk for developing osteoporotic fractures of any type, and vertebral compression fractures represent 25% of osteoporotic fractures. Painful vertebral compression fractures may cause a marked decline in physical activity and quality of life, leading to general physical de-conditioning. This, in turn, may prompt further complications related to poor inspiratory effort (atelectasis and pneumonia) and venous stasis (deep venous thrombosis and pulmonary embolism).
Successful management of painful vertebral compression fractures has the potential for improving quality of life, increasing the expectancy of an independent and/or productive life, and preventing superimposed medical complications. Some have suggested that management of painful vertebral compression fractures may also have a cost benefit for society as a whole; however, assessment of any potential societal benefits is difficult due to the inexactness of methods for quantifying pain-related disability.
Management Overview
The traditional first-line treatment of painful vertebral compression fractures is conservative management, which includes medical management with or without methods of immobility. Most pain-related symptoms from vertebral compression fractures are resolved with this management. Successful medical management also involves appropriate screening for osteoporosis and appropriate follow-up treatment.
Attributions
Figure 6.8A Lateral x-ray of the lower spine, T12 fracture by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figure 6.8B Sagittal CT, reformat, of the lower spine, T12 fracture by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.

