Chapter 15 – Pediatric
Pyloric Stenosis
ACR – Pediatric – Vomiting in Infants Up to 3 Months of Age
Case
Probable HPS
Clinical:
History – This three month old male had developed non-bilious vomiting.
Symptoms – There was repetitive, projectile vomiting in the recent few days. The child was loosing weight.
Physical – There was suspicion for a palpable olive.
Laboratory – Metabolic alkalosis was identified.
DDx:
Pylorospasm
Hypertrophic Pyloric Stenosis
Annular Pancreas
Imaging Recommendation
ACR – Pediatric – Vomiting in Infants Up to 3 Months of Age, Variant 4
Ultrasound

Imaging Assessment
Findings:
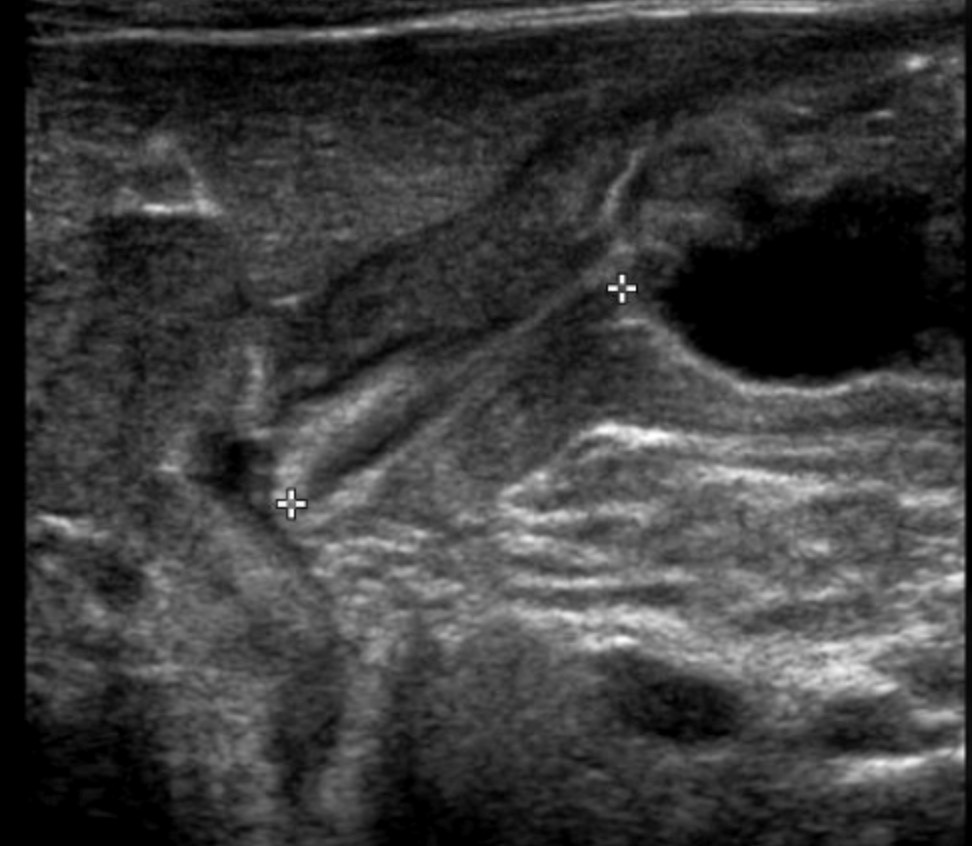
The stomach was filled with fluid. The short axis and long axis measurements of the pyloric channel were at the upper limits of normal. There was hyperperistalsis of the stomach. Fluid was not seen leaving the stomach and entering the duodenum.
Interpretation:
High suspicion for hypertrophic pyloric stenosis (HPS).
Diagnosis:
Probable HPS.
Discussion:
The most common conditions to produce acute non-bilious vomiting during infancy are gastroesophageal reflux (GER), viral gastroenteritis, pylorospasm, and hypertrophic pyloric stenosis (HPS). HPS is typically suggested by forceful bile-free emesis in a previously healthy infant around 6 weeks of age. Forceful vomiting may be reported in patients with GER, particularly in overfed patients.
When a classical “olive” of hypertrophied pyloric muscle is palpated, the diagnosis of HPS can be made clinically, and the patient can be sent to surgery for a pyloromyotomy (Heller’s myotomy) without the need for imaging examinations.
Recent advances in laparoscopic surgery suggest that accurate measurements of pyloric muscle thickening are useful in the planning of surgery, even when the diagnosis is clinically evident. When no “olive” is palpated, imaging by US or an UGI series can be performed for diagnosis.
X-ray findings may include:
- Abdominal radiography may show gastric distension with HPS.
- On occasion, mass impression of the thickened pyloric muscle on an air-filled gastric antrum may be noted.
- However, radiographs are most often not helpful in the diagnosis of HPS.
Upper Gastrointestinal Series findings may include:
- Though the contrast UGI series is excellent for diagnosing obstructive causes of vomiting in this age group it has the limitation of using ionizing radiation and therefore is less ideal than US as an initial screening test if HPS is a strong consideration.
- When doing an UGI in cases of HPS one can note the mass impression of the hypertrophied pyloric muscle on the barium-filled antrum (“shoulder sign”) or the filling of the proximal pylorus (“beak sign”) or the entire elongated pylorus (“string sign”) with barium.
- Because of the delayed gastric emptying present in cases of HPS the demonstration of the beak and string signs can be difficult to identify, often requiring considerable fluoroscopic time with a resultant increase in radiation exposure.
Ultrasonography findings may include:
- US has become a standard and highly accurate method for diagnosing HPS without the need for radiation exposure.
- It allows real-time imaging of the pyloric muscle and channel.
- The diagnosis of HPS is based on imaging of a constant elongated, thick-walled pylorus with no passage of gastric content.
- The diagnosis is supported by measurements of pyloric channel length and muscle thickness.
- Muscle thickness of ≥4 mm with an a length of >18 mm are considered positive for HPS, but measurements between 3 and 4 mm may also be positive, particularly in the premature or younger neonate.
- Muscle thickness measurement may be obtained on transverse or longitudinal views of the pylorus.
For some patients there is overlap of these measurements, most notably between patients with pylorospasm and patients with evolving HPS. Diagnostic caution with careful clinical follow-up has been suggested for the diagnosis of pylorospasm to avoid the possibility of under diagnosing cases evolving into HPS. Pylorospasm is said to be the most common cause of gastric outlet obstruction in this age group and, unlike HPS, it is treated conservatively.
Attributions
Figure 15.8A Abdominal ultrasound of the pylorus, longitudinal measurement by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figure 15.8B Abdominal ultrasound of the pylorus, transverse measurement by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.