Chapter 3 – Principles of Imaging Techniques
Magnetic Resonance Imaging (MRI)
Magnetic resonance images (MRI) are created by utilizing a high strength magnetic field and radio waves. All of the protons in the body are aligned in the cranial/caudal axis by the magnetic field of the MR. When a radio wave is broadcast into the body this perturbs the protons. When the radio wave ceases the protons snap back to align with the magnetic field. The protons liberate energy when they snap back into alignment with the magnetic field. This liberated energy is detected by sensor coils surrounding specific regions of the patient’s anatomy i.e. knee coils, head coils, etc. Through a process of complex, computer based, mathematical calculations the emitted energy is converted into pixels for digital image creation, display, and review. An MR machine is seen in Figure 3.40.
Image Appearance
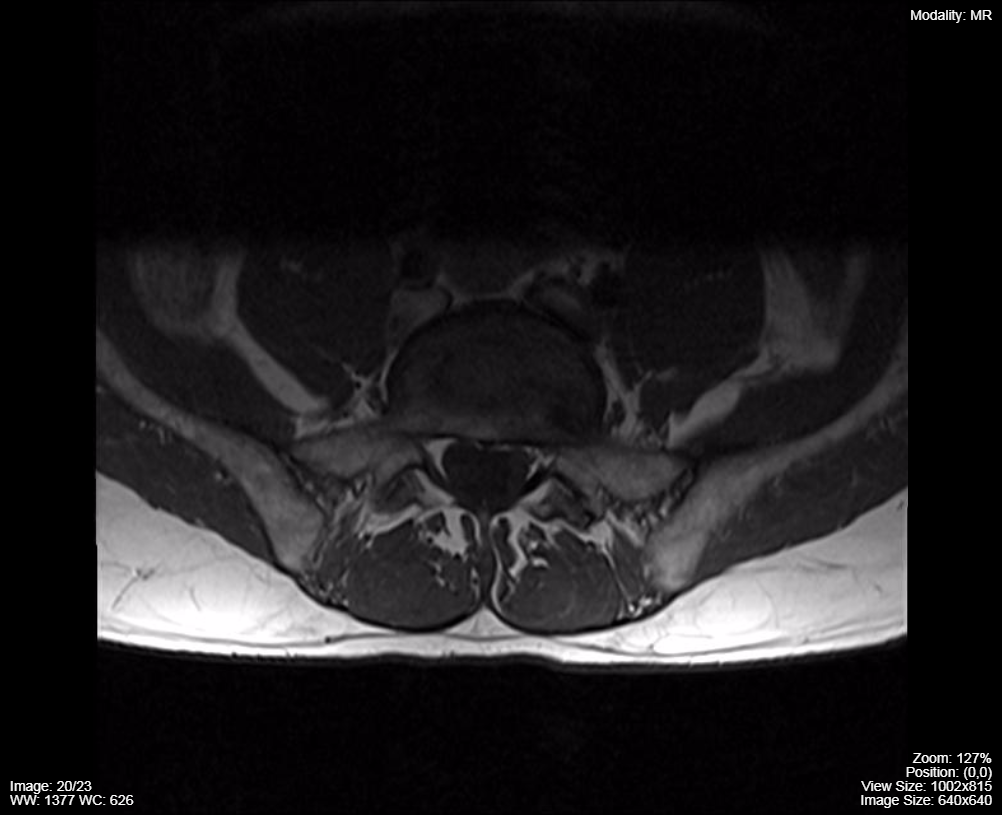
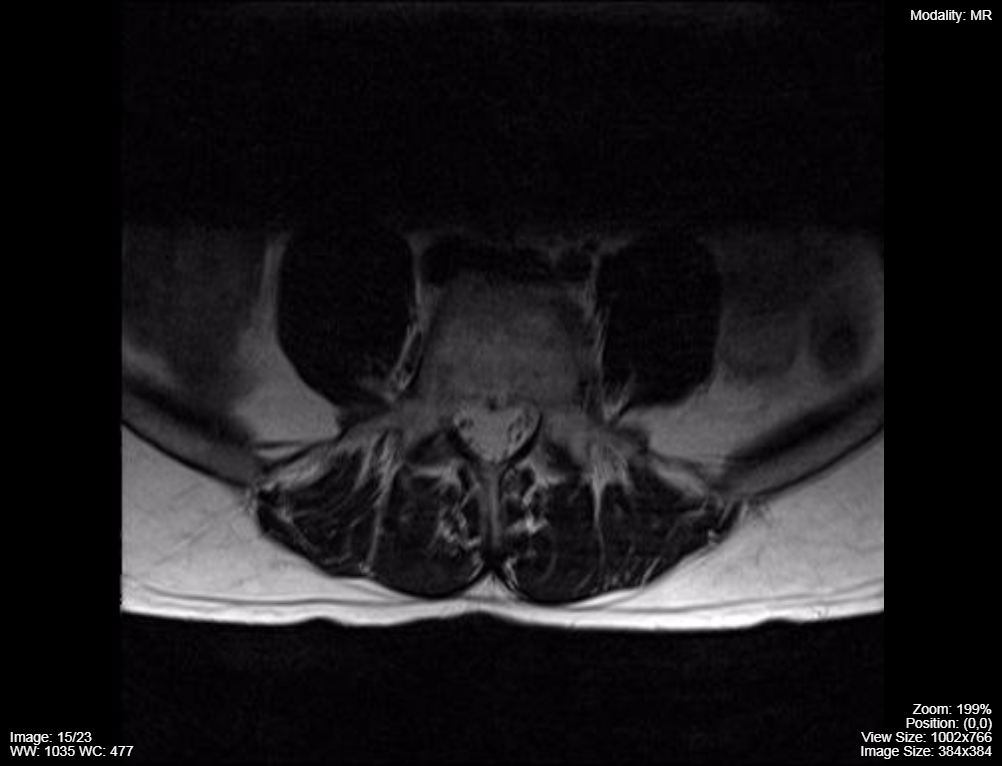
The appearance of different tissue on MR images is described as displaying greater, or lesser, signal in comparison the other anatomy in the region. The signal in question is the energy that the perturbed protons liberated when they fall back into alignment with the magnetic field. The signal intensity of the tissue in question changes based upon the image acquisition parameters set by the MR Technologist, under the direction of a supervising Radiologist. The parameters set result in the acquisition of a set of images called an MR imaging sequence. On one sequence cerebrospinal fluid will appear as black pixels (T1 sequence) while on another sequence it is white pixels (T2 sequence). This difference in tissue appearance can be exploited to determine if pathology is present.
MR Image Appearance:
- T1 Sequence – Cerebrospinal fluid appear as black
- T2 Sequence – Cerebrospinal fluid appears as white
Image Acquisition
Magnetic Resonance Imaging (MRI or MR), has the physical appearance of a Computed Tomography machine, i.e. it has a long tube with a tabletop that transports the patient into the centre of the tube for imaging. Patients lie on their back (supine) in the MR machine just like CT. The patient does not need to move or be re-positioned in the scanner to improve, or alter, the appearance of the patient’s anatomy. The patient does need to be prone for breast imaging, but that is the only examination that requires altered patient positioning.
The body region of interest for MR is surrounded by a coil that creates the radio waves and captures the radio waves used to create the images. There are different coils for different anatomic regions i.e. knee, head, breast, etc.
There are MR machines that do not have a tube or bore configuration called open magnets. They are designed to image children, obese patients and claustrophobic patients. These units are less frequently deployed in clinical practice.
MRI can acquire images in any plane of anatomic orientation, but these must be acquired as separate imaging sequences with unique technical parameters set for each sequence. Therefore, the more MR sequences planned, the longer the examination will take. This is unlike CT where the creation of images in alternative anatomic planes is performed by software manipulation of the pixels after image acquisition.
Safety
MRI is for the most part a very safe imaging modality. Some examinations may require intravenous contrast agents (Gadolinium based) and patients with known hyper-sensitivity to these agents should not have MR with contrast. Gadolinium based contrast agents may also cause renal injury in some patients who have predisposing poor renal function. One should consult with the imaging centre prior to booking a patient with diminished renal function for a contrast enhanced MR.
This imaging modality utilizes very high strength magnetic field to generate images. There are potential hazards related to missile type incidents where ferromagnetic objects are rapidly drawn into the MR magnet. In addition, implanted objects in patients such as cochlear implants, pacemakers and leads, aneurysm clips, and other medical devices may interact with the magnetic field. Patients require rigorous screening by the referring medical team and by the MR team to prevent serious adverse events related to magnetic field related injuries.
Contraindications to MRI:
- Known hyper-sensitivity to Gadolinium based agents
- Renal insufficiency
- Claustrophobia
- Implanted metallic medical device (cochlear implants, pacemakers and leads, aneurysm clips)
MRI depicts exquisite anatomic detail and provides the best depiction of anatomy of any of the imaging modalities. As with CT, the appearance of MR images can be modified by the addition of contrast agents.
MRI can also be used to visualize blood moving in vessels and it can also acquire images that analyze the molecular composition of tissue i.e. MR spectroscopy. There are also some MR imaging sequences that can detect differential metabolic activity in tissue and this can be applied to brain activity assessment i.e. functional MR (fMRI).
Hence, MRI has become one of the most important and versatile imaging tools in the Medical Imaging Department. It is particularly valuable for Neurologic and Musculoskeletal imaging. (Figures 3.41, 3.42)
T1 Axial MRI
T1 Sagittal MRI

T2 Sagittal MRI

Attributions
Fig 3.40 Magnetic Resonance Imaging Machine by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Fig 3.41A Lumbar Spine MRI T1 Sequence – Dark Cerebrospinal Fluid, Axial Plane by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Fig 3.41B Lumbar Spine MRI T1 Sequence – Dark Cerebrospinal Fluid, Sagittal Plane by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Fig 3.42A Lumbar Spine MRI T2 Sequence – White (bright) Cerebrospinal Fluid, Axial Plane by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Fig 3.42B Lumbar Spine MRI T2 Sequence – White (bright) Cerebrospinal Fluid, Sagittal Plane by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.

