Chapter 6 – Brain and Spine
Ischemic Stroke
ACR – Neurologic – Cerebrovascular Disease
Case
Ischemic Stroke
Clinical:
History – This patient had right sided weakness for 5 hours.
Symptoms – Right sided weakness.
Physical – Hemiparesis on the right. Diminished right reflexes.
DDx:
Stroke
Transient Ischemic Attack (TIA)
Imaging Recommendation
ACR – Cerebrovascular Disease, Variant 3
CT Head without IV contrast

Imaging Assessment
Findings:
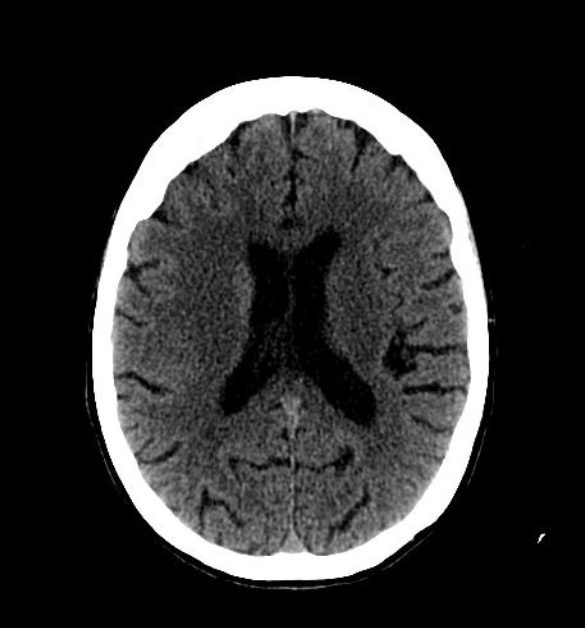
The left basal ganglial region and the left caudate head were of abnormally low density. There was also loss of the grey matter/white matter differentiation in the left frontal region. The left middle cerebral artery was hyperdense compare to the right suspicious for arterial thrombosis. No intracranial hemorrhage.
Interpretation:
Ischemic stroke in evolution. Possible middle cerebral artery thrombosis.
Diagnosis:
Ischemic stroke.
Discussion
Stroke is a nonspecific term that usually denotes an acute loss of neurologic function. It often occurs when the blood supply to an area of the brain is lost or compromised.
The diagnosis of stroke is usually made clinically. Patients with suspected stroke are imaged to determine if there is another cause for the neurologic impairment besides a stroke (e.g., a brain tumor), to attempt to determine the distribution and severity of the stoke on imaging, and to identify the presence, or absence, of brain parenchymal blood to distinguish ischemic from hemorrhagic stroke. CT can determine whether, or not, hemorrhage is present and may help to determine whether, or not, thrombolytic therapy will be instituted. CT may identify the infarct and characterize it in regards to its vascular distribution.
- Strokes are divided into two large groups: ischemic or hemorrhagic. Ischemic strokes are more common. The classification is important because rapid treatment of ischemic stroke with tissue plasminogen activator (t-PA) or another form of intra-arterial recanalization can improve the prognosis.
- A common cause of ischemic strokes are intra-arterial emboli, the emboli may arise from the heart, the aorta, the common carotid bifurcation or the internal carotid artery bulb.
- The other possible cause of stroke is thrombosis, representing in situ occlusion of the carotid, vertebrobasilar, or intracerebral circulation from an atheromatous lesion or large embolus from the central arterial circulation.
- Most acute strokes are initially imaged by obtaining a non-contrast-enhanced CT scan of the brain (within 24 hours of the onset of symptoms), mostly because of its availability.
CT findings of an Ischemic stroke may include:
- The findings depend upon the amount of time that has elapsed since the original ischemic event.
- 0 – 12 hours, imaging may be normal.
- 12 to 24 hours, indistinct area(s) of low attenuation in a vascular distribution.
- > 24 hours, better circumscribed low density lesion(s) with mass effect due to associated edema, that peaks 3 to 5 days after and usually disappears by 2 to 4 weeks.
- > 4 weeks, mass effect disappears. There is now a well-circumscribed, low-attenuation lesion with no contrast enhancement. There may be volume loss in the brain with concomitant prominent CSF spaces in the involved region.
Attributions
Figure 6.3A Axial CT of the Head displaying findings of an ischemic stroke by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC–BY-NC-SA 4.0 license.
Figure 6.3B Axial CT of Head displaying findings of an ischemic stroke by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.

