Chapter 6 – Brain and Spine
Intracranial Hemorrhage – Traumatic
ACR – Neurologic – Head Trauma
Case 1
Subdural Hematoma (SDH)
Clinical:
History – This elderly male was more confused than normal and had a more unstable gait since a fall 7 days prior to visiting the ER. The patient was on Plavix related to a previous ischemic stroke.
Symptoms – Confusion and weakness.
Physical – The patient was unaware of his location and the date. He had great difficulty standing without the support of his caregivers. He could not walk.
DDx:
Brain ischemia
Brain tumor
Subdural hematoma
Imaging Recommendation
ACR – Minor, Acute, Closed, Head Injury, Variant 2.
CT of the Head without IV contrast
Imaging Assessment
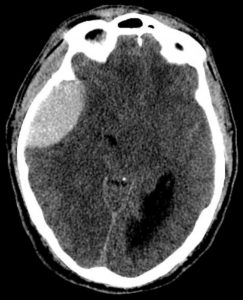
Findings:
There was significant shift of the midline structures to the right. The patient had a mixed density fluid collection in the left subdural space that had regions of water density and regions of higher density within it. There was a layering effect with the brighter fluid posteriorly situated. No large territory infarcts. There was subfalcine herniation of the frontal lobe on the left. No fractures identified.
Interpretation:
Subacute, Subdural Hematoma, Left
Diagnosis:
Subacute, Subdural Hematoma, Left (7 days)
Discussion:
- Subdural hematomas are more common than epidural hematomas and are usually not associated with a skull fracture. They are most commonly a result of deceleration injuries in motor vehicle or motorcycle accidents (younger patients) or secondary to falls (older patients).
- Subdural hematomas are usually produced by damage to the bridging veins that cross from the cerebral cortex to the venous sinuses of the brain. They represent hemorrhage into the potential space between the dura mater and the arachnoid.
- Subdural hematomas usually develop over a longer time period and symptoms and signs may develop slowly.
- An acute subdural hematoma frequently suggests the presence of more severe parenchymal brain injury, with increased intracranial pressure, and the acute subdural may be associated with higher morbidity and mortality.
Imaging findings may include:
- On CT, acute subdural hematomas are crescent-shaped, extra-cerebral bands of high attenuation that may cross suture lines and enter the interhemispheric fissure. They do not cross the midline.
- Typically, a SDH is concave on the inward side towards the brain (epidural hematomas are convex on the inward side).
- As time passes and they become subacute, or if the subdural blood is mixed with lower-attenuating CSF, they may appear isointense (isodense) to the remainder of brain, in which case you should look for compressed or absent sulci or sulci displaced away from the inner table as signs of SDH. For subtle, isodense subdural hematomas, the addition of intravenous contrast for the CT scan may help to enhance the brain gray matter creating a more discernible difference between the gray matter and the non-enhancing subdural hematoma.
- Subdural collections may demonstrate a fluid-fluid level after 1 week, as the cellular matter in the blood settles under the serum.
Case 2
Epidural Hematoma
Clinical:
History – This young male was in a motorcycle accident. He was not wearing a helmet and collided with a parked car at low speed.
Symptoms – He had minor bruising over his right frontal-temporal region. Initially, the patient was able to talk and understood his situation. However, over the next hour he progressed to being obtunded.
Physical – Swelling overlying the right frontal-temporal region. Glasgow coma scale 8. He was non-responsive to verbal commands.
DDx:
Subdural hematoma
Subarachnoid hemorrhage
Brain parenchymal contusion
Epidural hematoma
Imaging Recommendation
ACR, Moderate to Severe, Acute, Head Injury, Variant 3
CT Head without IV contrast
Imaging Assessment
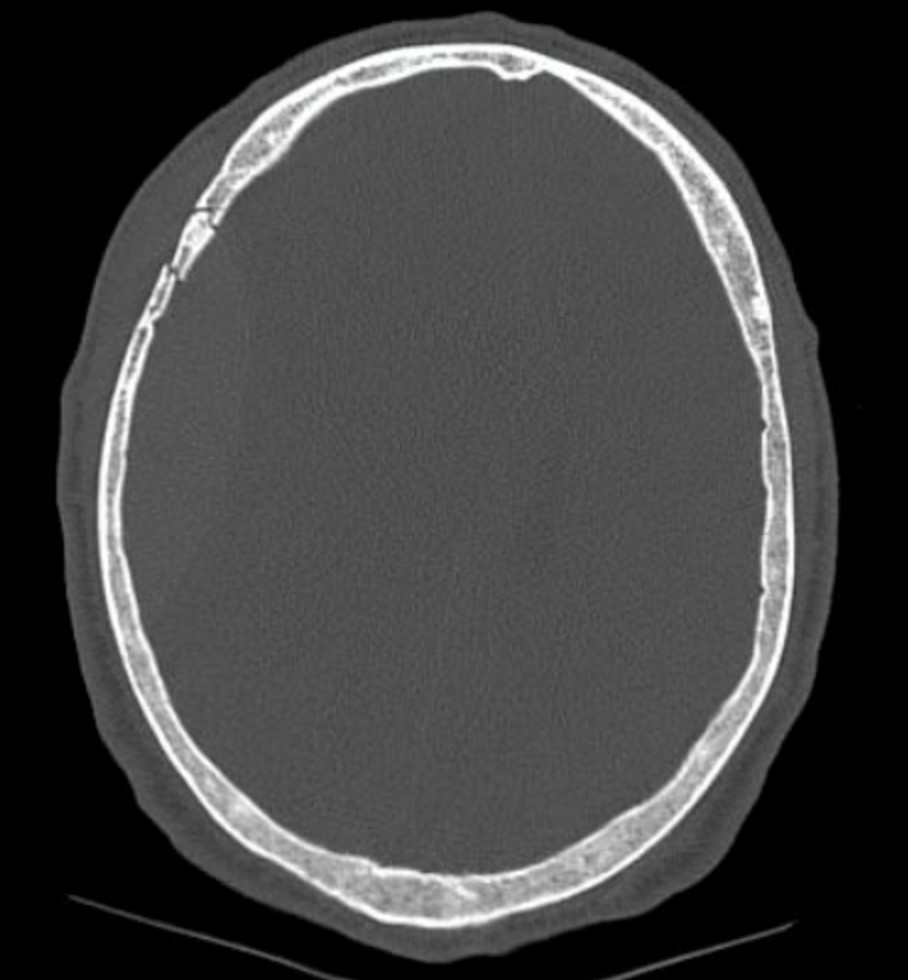
Findings:
There was minor soft tissue swelling overlying the right temporo-parietal region. A temporo-parietal fracture was seen in the right skull. There was a large, lenticular shaped, hyperdense, collection overlying the intracranial right temporal region. There was several areas of hyperdense foci in the deep right brain parenchyma. Severe subfalcine and moderate transtentorial herniation was seen.
Interpretation:
Epidural hematoma with brain parenchymal contusions.
Diagnosis:
Epidural hematoma with brain parenchymal contusions.
Discussion
- Epidural hematomas represent hemorrhage into the potential space between the dura mater and the inner table of the skull.
- Most cases are caused by injury to the middle meningeal artery or vein from blunt head trauma, typically from a motor vehicle accident.
- Almost all epidural hematomas (95%) have an associated skull fracture, frequently the temporal bone. This fracture injures the middle meningeal artery or vein.
- Epidural hematomas may also be caused by disruption of the dural venous sinuses adjacent to a skull fracture.
- Since the dura is normally fused to the calvarium at the margins of the sutures, it is impossible for an epidural hematoma to cross suture lines (subdural hematomas can cross sutures).
- Epidural hematomas can cross the tentorium (subdural hematomas do not).
Imaging findings may include:
- A high density, extra-axial, biconvex, lens-shaped mass, most often found in the temporo-parietal region.
- There is often an underlying skull fracture, it may traverse the groove in the skull for the middle meningeal artery.
Attributions
Figure 6.1A Axial CT of Brain at the level of the septum pellucidum by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC–BY-NC-SA 4.0 license.
Figure 6.1B Axial CT of Brain more caudal compared to Figure 6.1A by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC–BY-NC-SA 4.0 license.
Figure 6.2A Axial CT of Head displaying epidural hematoma by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC–BY-NC-SA 4.0 license.
Figure 6.2B Axial CT of Head displaying epidural hematoma by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC–BY-NC-SA 4.0 license.



