Chapter 14 – Musculoskeletal
Elbow Fractures
Case 1
Radial Head Fracture
Clinical:
History – This patient fell forward after tripping on a curb.
Symptoms – Very painful elbow.
Physical – Forearm movements were painful and limited. Tenderness was elicited over the radial head distal to the lateral epicondyle on palpation.
DDx:
Radial, ulnar, or humeral fracture
Elbow dislocation
Soft tissue trauma
Imaging Recommendation
X-ray


Imaging Assessment
Findings:
There was a comminuted radial head fracture. This was an intra-articular fracture. No obvious loose bone fragments in the joint space on the subsequent CT.
Interpretation:
Radial head fracture, intra-articular, comminuted.
Diagnosis:
Radial head fracture, type 3, comminuted.
Discussion:
Radial head fractures are usually caused by a fall on an outstretched hand with a pronated forearm, or with the elbow in slight flexion, or a direct blow to the lateral elbow. Standard radiography is generally adequate, although an oblique or radio-capitellar view may be necessary.
X-ray findings may include:
- A variety of fracture orientations may be seen consisting of a transverse neck fracture, linear or oblique fractures in any plane, triangular or quadrangular fragments.
- There will be a joint effusion.
- There may be impaction and angulation of the radial head.
Radial head fractures are classified using the Mason system:
| Type | Description |
| 1 | Undisplaced fracture, no mechanical obstruction |
| 2 | Presence of displacement, (>2mm) or angulation > 30 degrees |
| 3 | Comminuted fracture |
| 4 | Fracture with elbow dislocation |
Table 14.1 Classification of radial head fractures based on the Mason System
Mason type I fractures are generally treated conservatively and can be managed in the primary care setting. For these fractures, the elbow is placed in a posterior splint for five to seven days, followed by early mobilization and a sling for comfort. There is some evidence supporting the immediate initiation of elbow motion in patients with a Mason type I fracture. Imaging of Mason type I fractures should be repeated after one to two weeks to ensure appropriate alignment. Physical therapy may be added to encourage range of motion.
Orthopedic consultation is generally warranted for treatment of Mason type II through IV fractures.
Case 2
Supracondylar Fracture
Clinical:
History – This 5 year old male fell off the monkey bars.
Symptoms – Painful deformed elbow.
Physical – The elbow was swollen and very tender.
DDx:
Fracture or dislocation of the elbow
Imaging Recommendation
X-rays
Imaging Assessment
Findings:
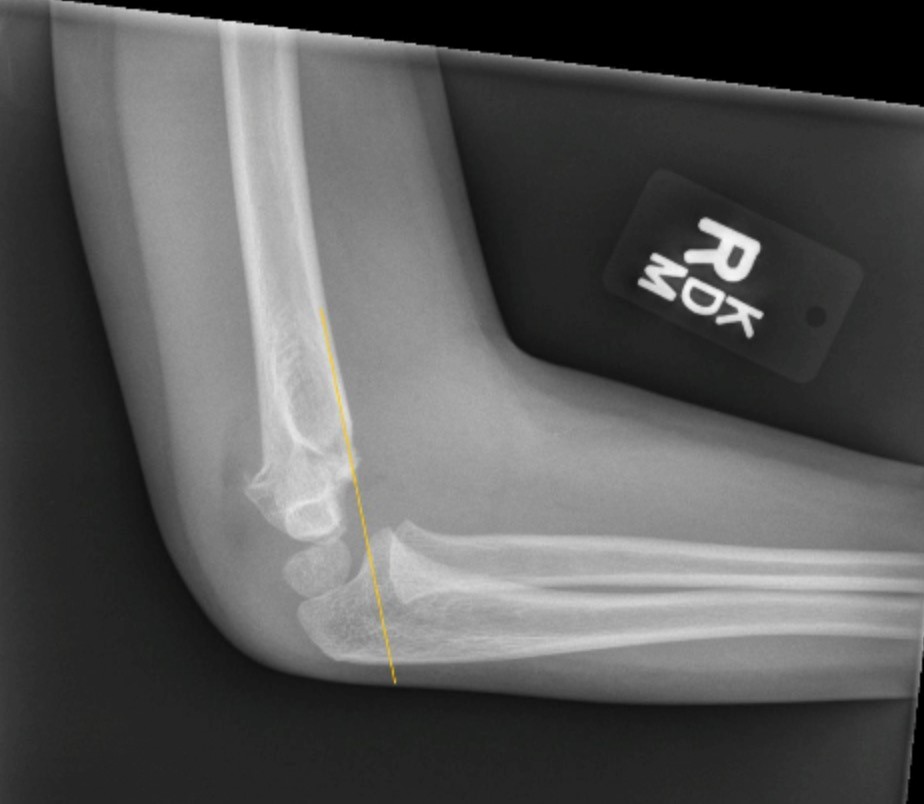
There was a displaced fracture of the distal humerus, with ventral displacement of the anterior fat pad, consistent with a joint effusion.
Interpretation:
Supracondylar humeral fracture. Orthopedic consult was recommended.
Diagnosis:
Supracondylar Humeral Fracture
Discussion:
Simple supracondylar fractures are typically seen in younger children (90%, and are uncommon in adults. These fractures are more commonly seen in boys. These injuries are almost always due to accidental trauma, such as falling from a moderate height with a hyper-extended elbow (e.g. bunk bed or monkey-bars).
Mechanism
The fracture results in an intra-articular fracture line, and when displaced there is posterior displacement of the distal humeral component.
Radiographic classification
| Type I | Undisplaced |
| Type II | Displaced with intact cortex |
| Type III | Complete displacement |
Table 14.2 Radiographic classification of supracondylar humeral fracture
X-ray findings may include:
- Lateral and AP radiographs are usually sufficient, and in many instances demonstrate an obvious fracture.
- Often, however, no fracture line can be identified. In such cases assessing for indirect signs is essential:
a) Anterior fat pad sign (sail sign): the anterior fat pad is elevated by a joint effusion and appears as a ventral, lucent triangle on the lateral projection
b) A visible posterior fat pad may also be seen but this is less common
b) Anterior humeral line should intersect the middle third of the capitellum in most children.
Treatment and prognosis
Although in many cases the fracture is easily seen, in some instances all that may be seen is soft tissue swelling or an anterior fat pad sign. Even in the absence of an obvious fracture, the patient needs to be treated with a cast. Repeating radiographs after inflammation has subsided may be helpful in demonstrating the fracture; this is typically done 7-10 days later.
Management by Type
Type I (undisplaced) fractures are stable and can be treated with a cast for approximately 3 weeks.
Type II usually require reduction (especially when angulation is more than 20 degrees). Traditionally these fractures were treated with casting, however, increased risk of ischemic contracture (Volkmann contracture), has led to a higher frequency of percutaneous pinning and cast immobilization.
Type III fractures can sometimes be treated similarly to type II (closed reduction and percutaneous pinning) although frequently the fracture is held open by interposed soft tissues requiring open reduction.
Attributions
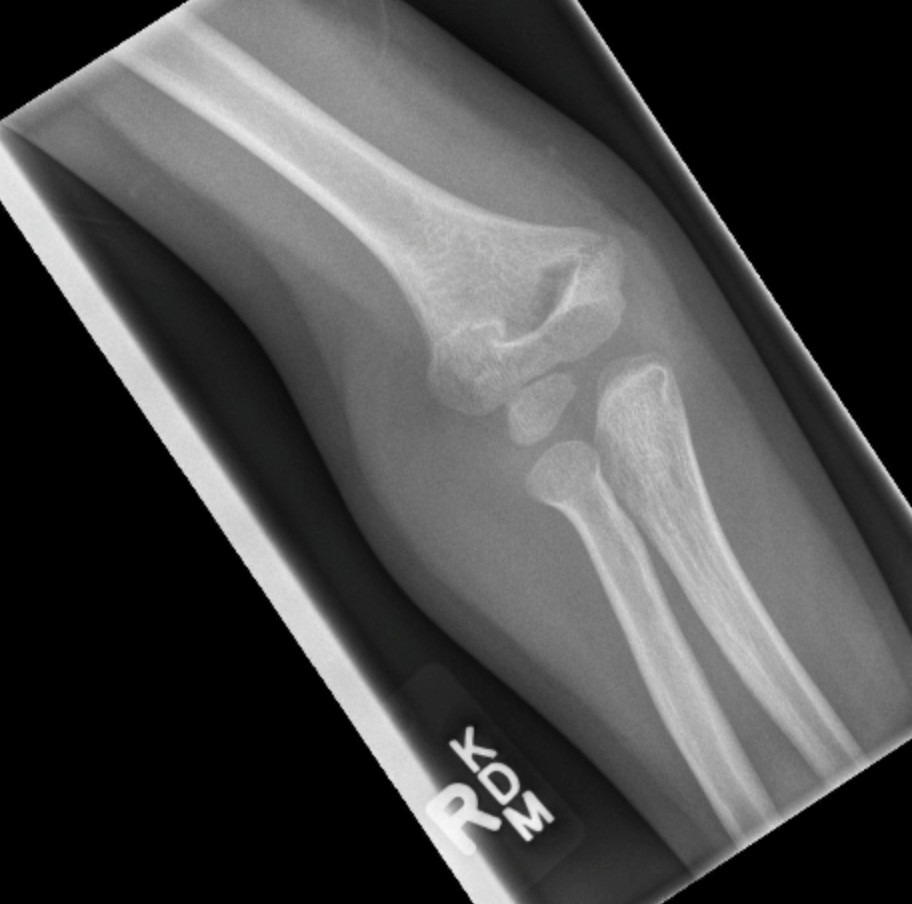
Figure 14.7A X-ray of the elbow displaying a radial head fracture by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figure 14.7B 3D imaging of the elbow with a radial head fracture by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figure 14.8A X-ray of the elbow displaying a humeral fracture by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figure 14.8B Lateral x-ray of the elbow displaying a humeral fracture. The anterior humeral line has been drawn on the image by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.