Chapter 10 – Gastrointestinal and Abdominal
Appendicitis
ACR – Right Lower Quadrant Pain
Case
Acute Appendicitis
Clinical:
History – This patient felt unwell and had nausea. She had been unwell for 48 hours.
Symptoms – The patient reported abdominal pain that began in the centre of the abdomen but had migrated to the right lower quadrant. Temperature was 39.5 C.
Physical – The abdominal exam revealed moderated tenderness in the right lower quadrant associated with guarding and rebound tenderness. No discernible mass.
Laboratory – The white blood cell count was elevated.
DDx:
Appendicitis
Abdominal abscess
Ovarian pathology
Imaging Recommendation
These differ for Adults, Children, and Pregnant Women.
Adults – CT Abdomen and Pelvis, Variant 1
Children – Ultrasound Abdomen first, CT if inconclusive, Variant 4
Pregnant Women – Abdominal X-ray’s are less appropriate



Imaging Assessment
Computed Tomography:
Findings:
There was a tubular structure, contiguous with the cecum, in the right lower quadrant with a calcification within it. This was a blind ending structure that was dilated and thick walled distal to the calculus. There was a small bubble of gas within this next to the calculus. No other findings.
Interpretation:
Inflamed appendix with an appendicolith. Consistent with appendicitis.
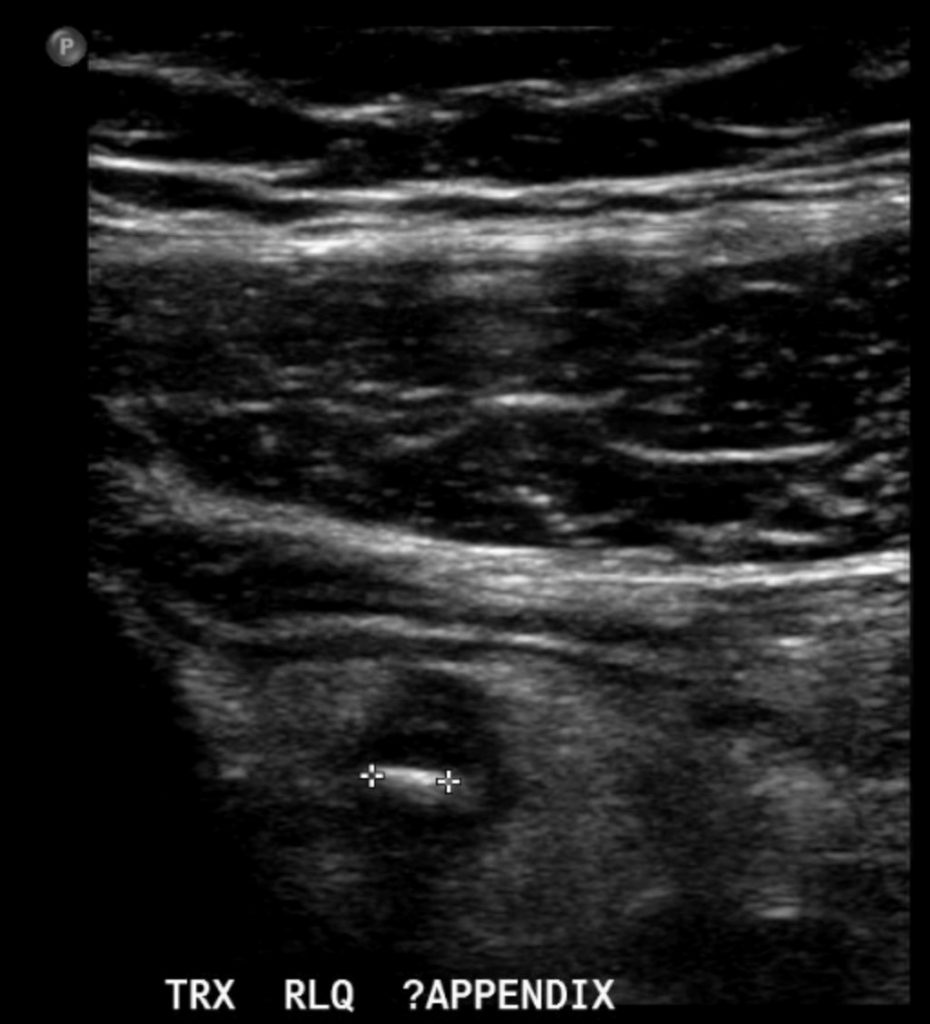
Ultrasound:
Findings:
A thick walled, blind ending tubular structure was seen in the right lower quadrant. A shadowing calculus was seen in this tubular structure. The tubular structure was very painful with graded compression. No fluid in the vicinity. No adenopathy.
Interpretation:
The findings were in keeping with appendicitis.
Diagnosis:
Appendicitis
Discussion:
Appendicitis is an extremely common cause for a surgical abdomen, i.e. fever, pain, tenderness, rebound tenderness, guarding (suggestive of peritonitis).
The most likely cause for appendicitis is blockage of the appendiceal lumen due to a calculus (appendicolith, 15 – 20%) or due to edema in the wall of the neck preventing the lumen from communicating with the cecum. Trapped intestinal contents in the appendix become static and infected leading to appendicitis.
Clinically, appendicitis often starts as obscure, central, abdominal pain that over time migrates to the right lower quadrant. The maximal site of tenderness in the right lower quadrant is often at McBurney’s point (one-third of the distance from the anterior iliac spine to the umbilicus).
The patient may develop guarding and rebound tenderness. If the appendix perforates the patient may develop sepsis related to an abscess or diffuse peritoneal infection.
CT is the imaging modality most useful in adults while US is best for children to avoid radiation exposure in the young.
Imaging findings that suggest appendicitis include:
- Appendicolith
- Blind ending, aperistaltic, tubular structure
- Appendix may be tender with graded compression using the ultrasound probe
- Thick appendix wall, > 6 mm
- Peri-appendiceal increased echogenicity
- Peri-appendiceal fluid
Attributions
Figure 10.8A Axial CT of an Adult Abdomen demonstrating a thick-walled appendix with a calcified appendicolith by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figure 10.8B Coronal CT of an Adult Abdomen, demonstrating a thick-walled appendix with a calcified appendicolith by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figure 10.9A Child ultrasound of appendix, short axis, demonstrating a thick-walled appendix with an appendicolith by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Figure 10.9B Child ultrasound of appendix, long axis, and blind end tubular structure with an appendicolith by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.

