Chapter 5 – Approach to Reviewing X-ray Imaging
General Approach to Reviewing x-ray Imaging
Have a strategy, stick to it, and look at the images systematically. Use a method that allows you to assess all of the images provided. You should individualize the image review process in order for you to internalize and standardize your approach.
A useful principle to use when interpreting medical images is that of symmetry i.e. most anatomy in the chest is symmetrical from right to left so you can compare and contrast within the image. This does not hold true for the cardiac silhouette, for example, but is useful for bones and the lungs in general. When possible, assess the image from side-to-side to look for symmetry.
Air rises and this can give you a clue as to the position of the patient when the image was taken, i.e. upright, supine, or decubitus. Pathologic collections of gas/air also rise based upon patient position, e.g. a pneumothorax is best seen in the apex of the hemithorax on an upright chest x-ray.
Images may be modified by the addition of positive contrast (barium, water soluble iodine, etc.) or negative contrast (air, carbon dioxide, etc.) to facilitate the detection of abnormality.
Look for these technical features when reviewing x-rays
1. Name, Age, Gender, Date of image acquisition, and Laterality.
Patient (name/ identification number(s)/ date of birth, gender).
Date and time the image was taken.
Ensure laterality is correct i.e. the Right or Left marker should correspond to proper anatomic orientation.
Determine if previous imaging is available for comparison.
Assessment of these elements is pivotal in matching the image with the particular clinical situation. Reviewing the most recent imaging is paramount. Comparison of the most recent imaging to previous imaging will allow for the detection of changes related to pathology or treatment.
2. Is the image too dark or too light?
If the x-ray is too light (white) this is related to insufficient x-rays reaching the detector. This could be due to the x-ray technologist not programming the x-ray machine to deliver an adequate dose of x-rays or it may be due to a large patient absorbing an excessive amount of the incident x-ray beam. If too much radiation has been administered for the image acquisition, the resulting image will be too dark (black). Both errors diminish the diagnostic utility of the x-ray.
3. Is the x-ray rotated in relation to anatomic position?
Images should be acquired in anatomic position when possible. The process of the standardization of patient positioning for x-rays results in a predictable appearance of the images and will assist the image interpreter in developing an concept of what normal images look like.
This subsequently facilitates the detection of abnormalities in anatomy as the interpreter has a strong foundation in what normal images look like. Non-anatomic positioning can alter the appearance of an x-ray and one must learn the effects of this sub-optimal positioning on the utility of the final image(s) and not be misled into suggesting that the images are abnormal.
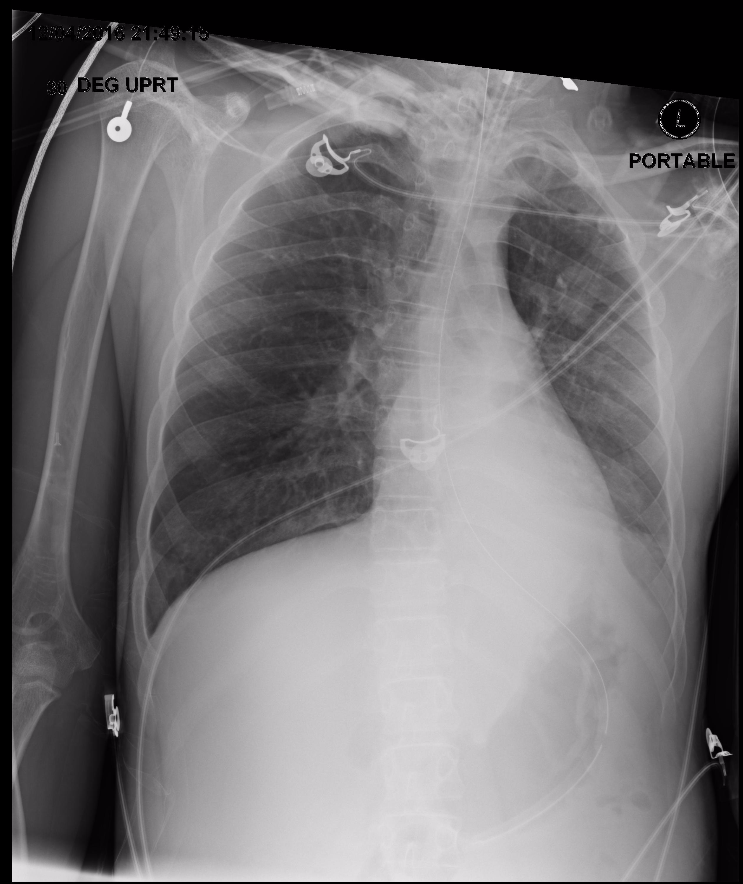
Rotated, Tilted, Poor Inspiration
Better Positioning

4. Has important anatomy been missed on the available image?
Infrequently, the images provided do not include important pertinent anatomy e.g. the chest x-ray image does not include one of the hemidiaphragms or costophrenic angles. This can result in an error. If the excluded anatomy is clinically important, repeat radiographs will be necessary.
Reviewing X-ray Imaging:
- Name, Age, Gender, Date of Image Acquisition
- Is the x-ray too dark or too light?
- Is the x-ray rotated in relation to anatomic position?
- Has important anatomy been missed on the available image?
Attributions
Fig 5.1 A portable upright x-ray where the image is not taken with proper body alignment, the patient is rotated and tilted by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Fig 5.2 A portable upright x-ray taken with patient in proper alignment by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.

