11. Circulation
11.1 Introduction
11.1.1 Diffusion and Bulk Flow
11.1.2 What Needs to be Transported
11.1.3 Circulation in Simple Animals
11.1.4 Open Circulatory Systems
11.1.5 Closed Circulatory Systems
11.1.6 Overview of Circulation in Mammals
11.2 Blood and Other Circulatory Fluids
11.2.1 Composition of Blood
11.2.2 Plasma
11.2.3 Red Blood Cells, and Haemoglobin
11.2.4 White Blood Cells
11.2.5 Production of Blood Cells
11.2.6 Platelets and Clotting
11.2.7 Interstitial Fluid
11.2.8 Cerebrospinal Fluid
11.2.9 Lymph
11.3 Blood Vessels
11.3.1 Fluid Dynamics (Haemodynamics)
11.3.2 Arteries
11.3.3 Capillaries
11.3.4 Veins
11.3.5 Angiogenesis
11.4 The Vertebrate Heart
11.4.1 Single and Double Circulation
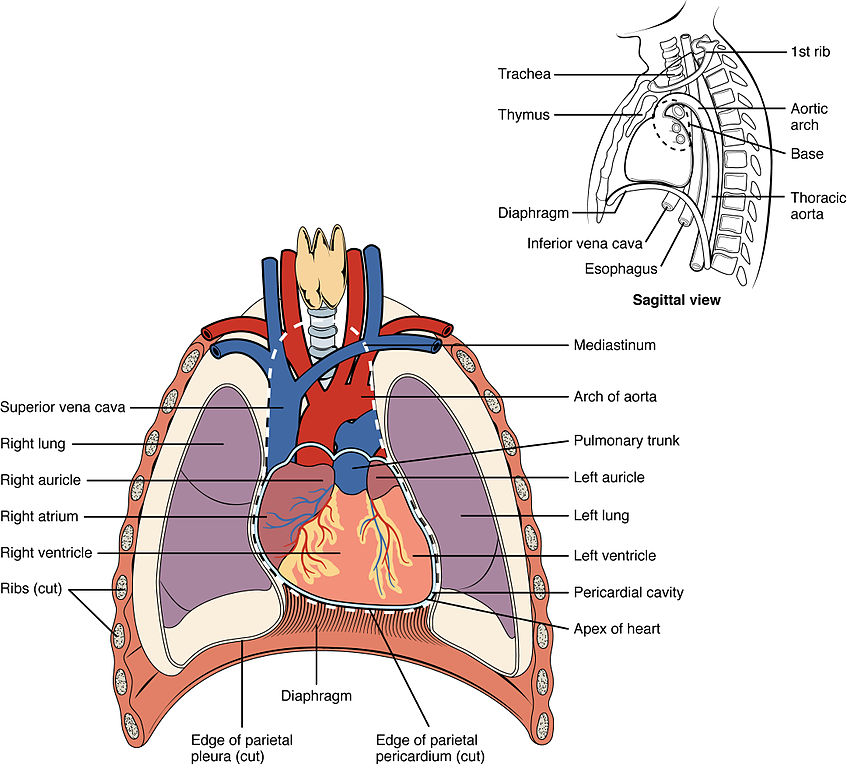
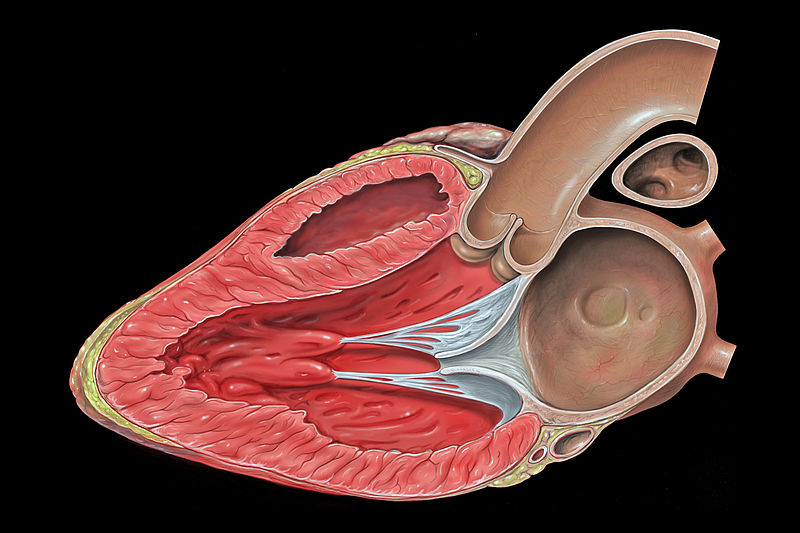
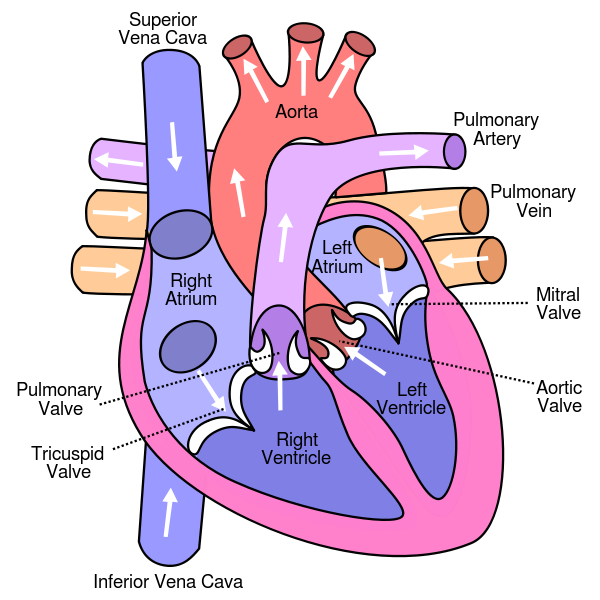
11.4.2 Heart Anatomy
11.4.3 Co-ordination of Heart Contraction
11.4.4 EKG
11.5 Control of Circulation
11.5.1 Ever-Changing Needs for Blood Flow
11.5.2 Vasodilation and Vasoconstriction
11.5.3 Heart Rate and Stroke Volume
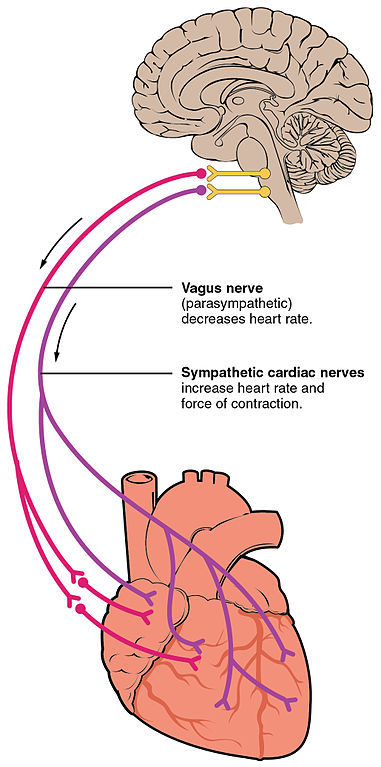
11.5.4 Neural Control of Circulation
11.5.5 Humoral Control of Circulation
11.5.6 Control of Angiogenesis
11.5.7 Control of Haematopoesis
11.5.8 Control of Blood Volume
11.6 The Lymphatic System
11.6.1 Lymph Production
11.6.2 Functions of Lymph
11.6.3 Lymphatic Ducts
11.6.4 Lymph Nodes
11.6.5 Lymphoid Organs
11.7 Summary
11.8 Suggested Readings
11.9 Glossary
– Proverbs 4:23
Spare a moment to thank the hardest-working muscle of your body: your heart.
Day and night, it works tirelessly, beating 80,000 times a day. By the time it stops, it’s likely to have contracted more than three billion times, pumping a volume of blood equal to 200,000 standard, long-course Olympic swimming pools. Be grateful.
11.1 Introduction
11.1.1 Diffusion and Flow
11.1.2 What Needs to be Transported
11.1.3 Circulation in Simple Animals
11.1.4 Open Circulatory Systems
11.1.5 Closed Circulatory Systems
11.1.6 Overview of Circulation in Humans
11.1.1 Diffusion and Flow
To sustain life, molecules need to get from one part of an animal’s body to another. In Chapter 10, Respiration, we reviewed two different ways a molecule can get from one place to another in a fluid.
Do you remember these two mechanisms? If not, re-read Section 10.3 of the Respiration chapter.
To recap, diffusion is the random bouncing around of a molecule relative to its neighbours in a fluid. Diffusion of small molecules is extremely fast over short distances, for instance across part of a cell, but very slow over longer distances. Why is diffusion over longer distances so slow? Because the path that a molecule takes is random, with many changes in direction due to collisions with other molecules. While the motion of individual molecules is random, in a population of molecules there is net diffusion from places of higher concentration to places of lower concentration as the molecules randomly distribute themselves.
Flow is the motion of a molecule with its neighbours. As a result, the path taken is relatively straight. Transport over longer distances is fast compared with diffusion.
As a result, all but the smallest animals need special systems to ensure the flow of extracellular fluid around the internal tissues of the body. This flow is called circulation.
11.1.2 What Needs to be Transported
As we reviewed in the previous section, the communication of substances throughout the body requires the circulation of extracellular fluids. Can you think of which substances need to be transported from cell to cell, tissue to tissue, or organ to organ, in the body?
We can make two lists: substances important for homeostasis[1] and metabolism[2], and substances important for communicating information from one part of the body to another. As you might imagine, these two lists overlap a lot with each other.
Take a moment to think of what needs to be transported, and then compare with the lists below.
Homeostasis and metabolism:
- water
- oxygen
- nutrients, for example:
- glucose
- lipids
- amino acids
- vitamins
waste products, for example:
- carbon dioxide
- lactic acid
- ammonia
salts
blood clotting factors
Information:
- hormones
- antibodes
- cells of the immune system
There’s one more item that needs to be transported, which is not a substance: heat. Control of blood flow to the skin and to the extremities plays an important role in controlling and maintaining body temperature. The control and maintenance of body temperature is called thermoregulation.
11.1.3 Circulation in Simple Animals
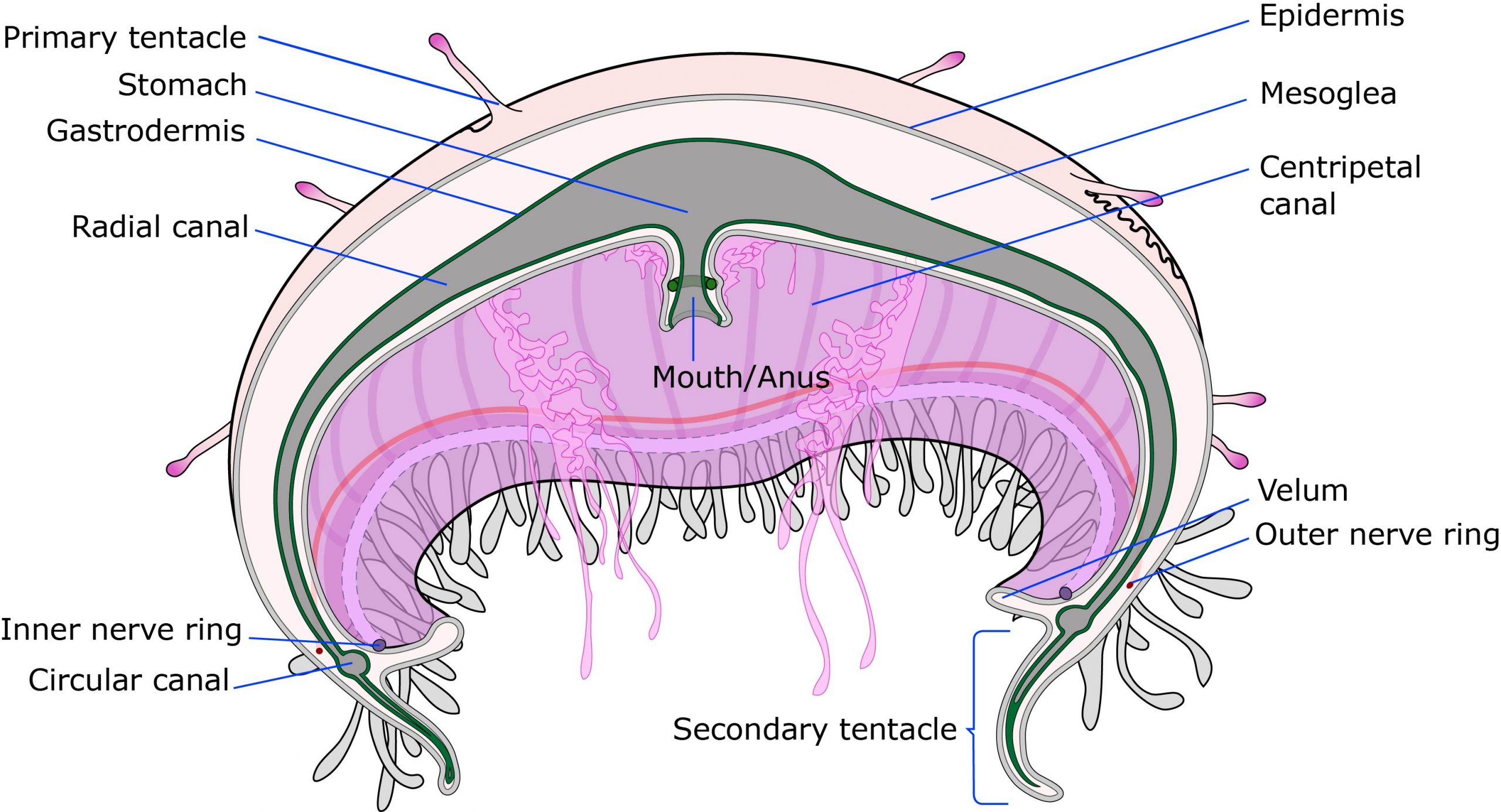
Diffusion can be enough for transport of chemicals in animals that are very small, or very flat, or concentrate their metabolically active tissues near their body’s outer surfaces. For example, the cnidarians – which include jellyfish, anemones, and corals – are diploblasts with only two germ layers: the ectoderm, mostly skin, and the endoderm, mostly gut. Between the two layers, there is a gel-like layer containing relatively few cells. It consists mostly of extracellular matrix of polysaccharides and glycoproteins. In many larger cnidarians, a branched gut that spreads throughout the body speeds up absorption of nutrients, elimination of wastes, and in some cases gas exchange. Such a gut is called a gastrovascular cavity.

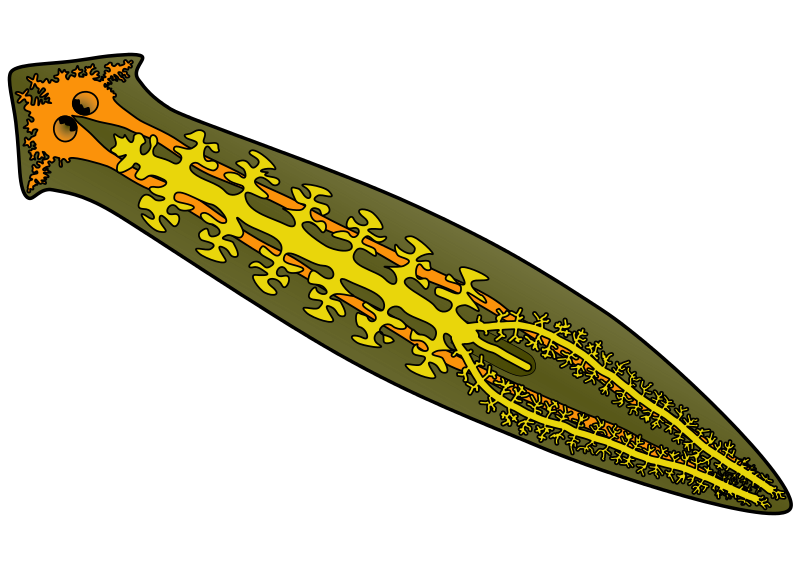
Some triploblastic animals – animals with ectoderm, mesoderm, and endoderm – have a gastrovascular cavity, too. In flatworms, the internal volume of the body is kept to a minimum by a flat overall shape of the body, and there is a little bit of circulation in the interstitial fluid between the cells of the mesoderm. This limited amount of circulation is often supplemented by an elaborately branched gut.
Some animals have very simple circulatory systems. For example, in sponges, water from the environment flows through the entire body. The flagella of the collar cells – choanocytes – drive the flow of external water, so that the water is constantly refreshed. The water brings oxygen, food, and soluble nutrients, and carries away carbon dioxide and other waste products. Diffusion can handle transport over the last couple of micrometres: The choanocytes are directly exposed to the external water, and none of the other cells of the sponge are far from the choanocytes and the external water.
Sponges are unusual among animals in that most cells of the body do feeding and gas exchange directly. Most animals don’t have this luxury. When gas exchange, digestion, waste removal, and other functions are done by separate organs, animals either need to be very small or flat, or they need internal fluids to transport water, gases, nutrients, wastes, and other substances.
Among animals that have simple body plans, some have one or more internal, fluid-filled body cavities that serve to transport material. For example, nematodes – roundworms – have a liquid-filled cavity surrounding their internal organs. As the worm crawls or swims, muscular movement of the whole body mixes the liquid around the body. The fluid-filled body cavity of nematodes is called a pseudocoelom, because the liquid is in direct contact with some of the ectoderm and endoderm cells. A liquid-filled body cavity completely lined with mesoderm cells is defined as a coelom. In some of the simpler coelomate animals, the coelom functions similarly to the pseudocoelom of nematodes, the liquid being mixed by movement of the whole body.
11.1.4 Open Circulatory Systems
In larger animals, simply relying on flow of interstitial fluid doesn’t suffice to exchange fluid fast enough through all of the tissues. To reduce resistance to flow of internal fluids, many animals have fluid-filled channels betwen internal organs. A further refinement is to line these channels with a layer of cells, such that you have a system of pipes leading from one part of the body to another. However, with a pipe isn’t of much help unless there’s a way to pump the liquid through in one direction.

Consider our cousin the sea squirt, for example: Sea squirts are among the closest living relatives of vertebrates. They are our closest invertebrate relative. Sea squirts start their lives swimming around as a tadpole-like stage, but soon they settle down to live a sedentary, sponge-like lifestyle as a filter feeder. They have among the simplest hearts of any animal: the sea squirt heart is a thin tube of muscle cells. Specialised muscle cells at one end act as a pacemaker: the pacemaker cells produce rhythmic action potentials without outside input. That is to say, the action potentials are myogenic. Gap junctions between the cardiomyocytes (heart muscle cells) allow the action potential to spread like a wave from the pacemaker down the tube of heart muscle. As a result, there’s a wave of muscle contraction that pushes the blood through the heart. We’ve seen this pumping mechanism before, in Chapter 8, Digestion. Do you remember what it’s called?[3]
The sea squirt’s heart is enclosed in a liquid-filled sac called the pericardium. The pericardium wall of a sea squirt consists of a tough, non-stretchy connective tissue, and functions to prevent the soft muscle tissue of the heart from blowing out like an overinflated bicycle tire. This allows the sea squirt’s heart to develop a high pressure to push the blood throughout the body. Many other animals have a pericardium too, but the pericardium performs different functions in different animal groups. In mammals, the pericardium serves mostly to lubricate the heart, so that it doesn’t rub against other organs while it beats.
Each end of the sea squirt’s heart connects to a blood vessel that branches into smaller vessels that open directly into the interstitial fluid. Because the blood vessels are open-ended, with the blood mixing directly with the interstitial fluid, the sea squirt is considered to have an open circulatory system. The circulating liquid in animals with an open circulatory system is often referred to as haemolymph.
Sea squirts can do a very unusual party trick: they can reverse the direction of flow through their circulatory system! The sea squirt heart has a second pacemaker, such that the heart has two pacemakers, one at each end. The two pacemakers take turns, such that the heart reverses the direction that it pumps haemolymph every few minutes.
Our own hearts used to be a simple tube of muscle too, when we were embryos. A muscular pipe with a pacemaker at one end works remarkably well as a pump. But this design doesn’t scale well to larger volumes of fluid or higher flow rates. How to modify a tube to make a pump that’s efficient under a wider range of circumstances? One modification is to add one-way valves. One-way valves are a common feature of circulatory systems. One, two, or three flaps of tissue are arranged in such a way that they open if the fluid pressure is higher on the upstream side than on the downstream side, and seal shut if the fluid pressure is higher on the downstream side that on the upstream side.
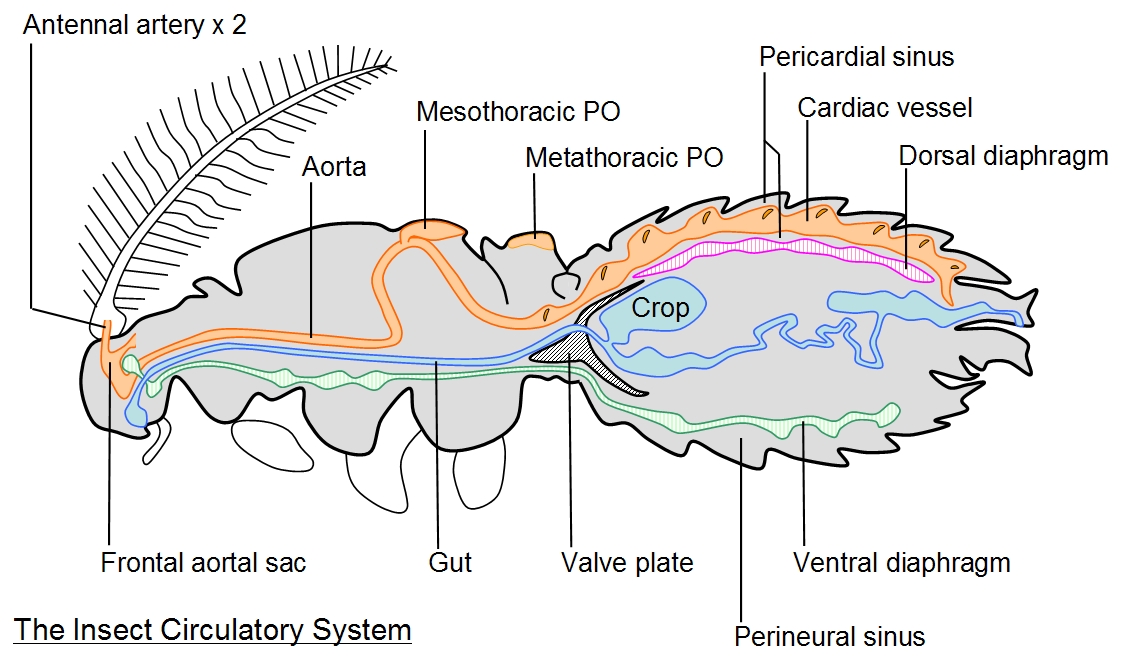
Many insects have a variation of this theme: a heart with intake valves. Insects have a large dorsal (along the back) haemolymph vessel that acts as a series of hearts or heart chambers. Each chamber has a pair of intake valves in its wall, to let haemolymph in from the pericardial space when the chamber expands, and close when the chamber contracts. The chamber contracts by muscular action, and elastic filaments attached to the outside of the chamber expand it when the muscle contracts. The blood vessels empty into spaces between the insect’s organs, thus insects also have an open circulatory system.
11.1.5 Closed Circulatory Systems
In many other animals, the ends of blood vessels join together such that few, if any, of the blood vessels have open ends. Since the blood is contained entirely within blood vessels and the heart, the blood can circuit around the body as a separate compartment from the other extracellular fluids.
The earthworm is an example of an animal with a closed circulatory system. The earthworm heart – of which an individual has several – has a simple design: Imagine a blood vessel with two one-way valves. The two valves define a chamber. The chamber can fill through the inlet valve. When the chamber contracts, the inlet valve seals shut, preventing blood from flowing back, and blood is forced out of the outlet valve. When the chamber relaxes, the outlet valve closes due to back pressure from the rest of the circulatory system and body, and the inlet valve opens. This is the basic design of hearts of many different animals.
Like open circulatory systems, closed circulatory systems seem to have evolved several times. Closed circulatory systems occur in many annelids (such as the earthworm), cephalopod molluscs (squid, octopus, cuttlefish, and nautilus), and all vertebrates.
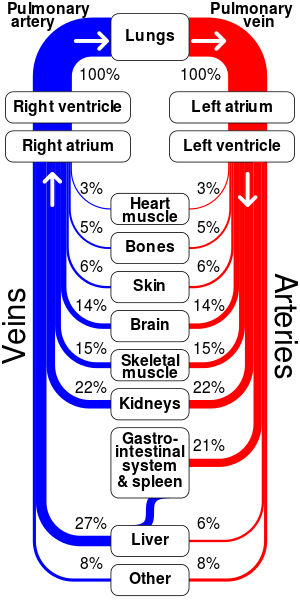
11.1.6 Overview of Circulation in Humans
For most of this chapter, we’ll use the human body as a typical example of a closed circulatory system. The blood, which is the main circulatory fluid, is in a separate compartment from the other extracellular fluids of the body. A special oxygen-binding protein called haemoglobin, packaged in red blood cells, allows the blood to carry many times more oxygen than it could otherwise. The blood flows in a closed loop of blood vessels, pushed by a muscular pump called the heart. The heart actually pumps the blood twice per circuit around the body, through two loops: one, through the lungs, and two, through the rest of the body. Exchange of materials with the body’s tissues happens in the smallest blood vessels, the capillaries. Because the blood has to be under pressure to flow through the vessels, pressure forces some of the fluid in blood through the capillary walls to join the tissue fluid, also called the interstitial fluid. The lymphatic system collects excess interstitial fluid and returns it to the blood.
11.2 Blood and Lymph
11.2.1 Composition of Blood
11.2.2 Plasma
11.2.3 Red Blood Cells, and Haemoglobin
11.2.4 White Blood Cells
11.2.5 Production of Blood Cells
11.2.6 Platelets and Clotting
11.2.7 Interstitial Fluid
11.2.8 Cerebrospinal Fluid
11.2.9 Lymph
11.2.1 Composition of Blood
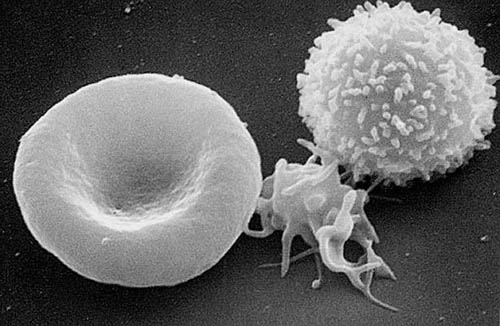
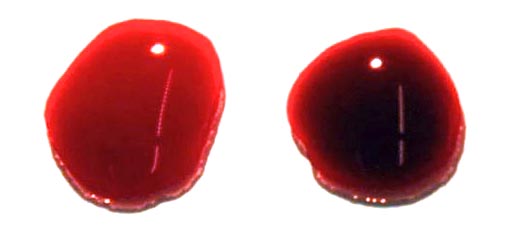
In vertebrate animals, blood is a mix of cells and liquid. Cells and cell fragments make up a large proportion of the volume of blood, typically almost half. The liquid portion is called plasma. The plasma carries all of the nutrients that tissues use and nearly all of the waste products that tissues produce, as well as hormones, antibodies, and soluble clotting factors. Most of the cells are red blood cells, also called erythrocytes (Greek, eruthrós: red; kútos: jar). Red blood cells are essentially bags of haemoglobin, the red-coloured protein that carries almost all of the oxygen and about a quarter of the carbon dioxide in blood. Blood cells that do not contain haemoglobin are called white blood cells, or leucocytes (Greek, leukós: white). There are several different kinds of white blood cell, each with a different function in the immune system. In mammals, blood also contains cell fragments called platelets, which are important for blood clotting. In other animals, a special kind of white blood cell performs the same function as platelets.
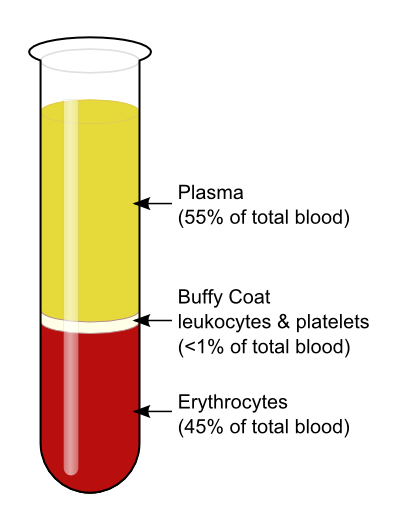
The packed cell volume (haematocrit) can be measured by centrifugation. In healthy humans the haematocrit can range from around 30% to around 60%, but in most women the haematocrit is around 42%, and in men sightly higher, around 45%. The constant flow of blood in a healthy individual normally keeps the cells suspended, preventing the blood cells from settling out.
11.2.2 Plasma
Plasma is the liquid in which the all other components of blood are either dissolved or suspended. Plasma has many constituents:
- Water. Plasma is over 90% water by mass, and over 99% water by number of molecules, so plasma is basically water containing solutes and colloids, listed below. Water in plasma is in equilibrium with water in most tissues of the body; for more on this topic, see Chapter 9 on osmoregulation.
- Salts and other electrolytes. The concentrations of salts and other electrolytes in plasma are very similar to their concentrations in the other extracellular fluids of the body.
- Proteins. Plasma is around 8% protein by mass.
11.2.3 Haemoglobin, and Red Blood Cells
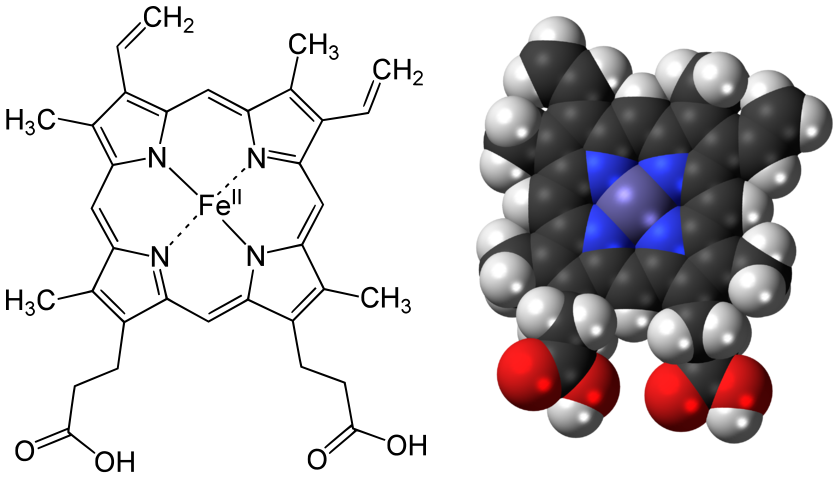
Why blood is red Blood plasma is mostly water, and water isn’t good at dissolving gases. Oxygen (O2) is no exception: For example, air contains about 40 times as much oxygen as the same volume of water saturated with oxygen at atmospheric pressure. And yet, in a large, active animal, blood has to deliver the entire oxygen supply to nearly all the tissues. How to solve this engineering challenge? Various groups of animals have evolved oxygen-carrying proteins called respiratory pigments. They’re called ‘pigments’ because they usually have a strong colour due to a transition metal atom. Oxygen molecules are hard to grab on to, even for a protein, so respiratory pigments contain a little helper: a metal atom that can form a temporary bond with oxygen, due to oxygen’s greediness for electrons. In vertebrate animals, the respiratory pigment is haemoglobin, containing iron. Various invertebrates have other respiratory pigments, including haemocyanin (blue when oxygenated; contains copper), erythrocruorin (red; contains iron), haemerythrin (pink when oxygenated; contains iron), and chlorocruorin (green when deoxygenated, red when oxygenated; contains iron).
As you learned in Chapter 10 (Respiration), haemoglobin increases the amount of oxygen that blood can carry 70-fold compared with water or plasma. For the blood in a human body, this means being able to carry a few minutes supply instead of only being able to carry a few seconds supply of oxygen. Given that it takes about a minute for blood to complete a circuit around the human body, it’s easy to see why haemoglobin is important.
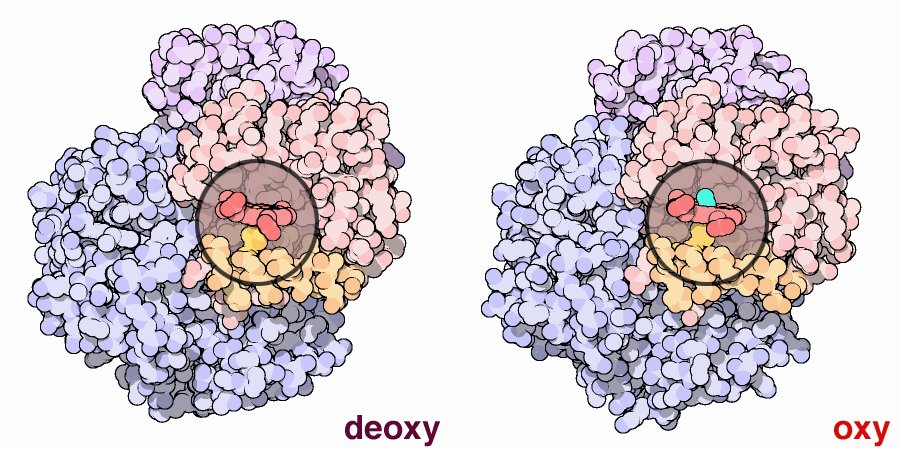
Let’s take a look at the structure of haemoglobin. Haemoglobin is a tetramer[4] of four globin protein chains. In human adults, most haemoglobin molecules contain two α-globin polypeptide chains and two β-globin polypeptide chains.
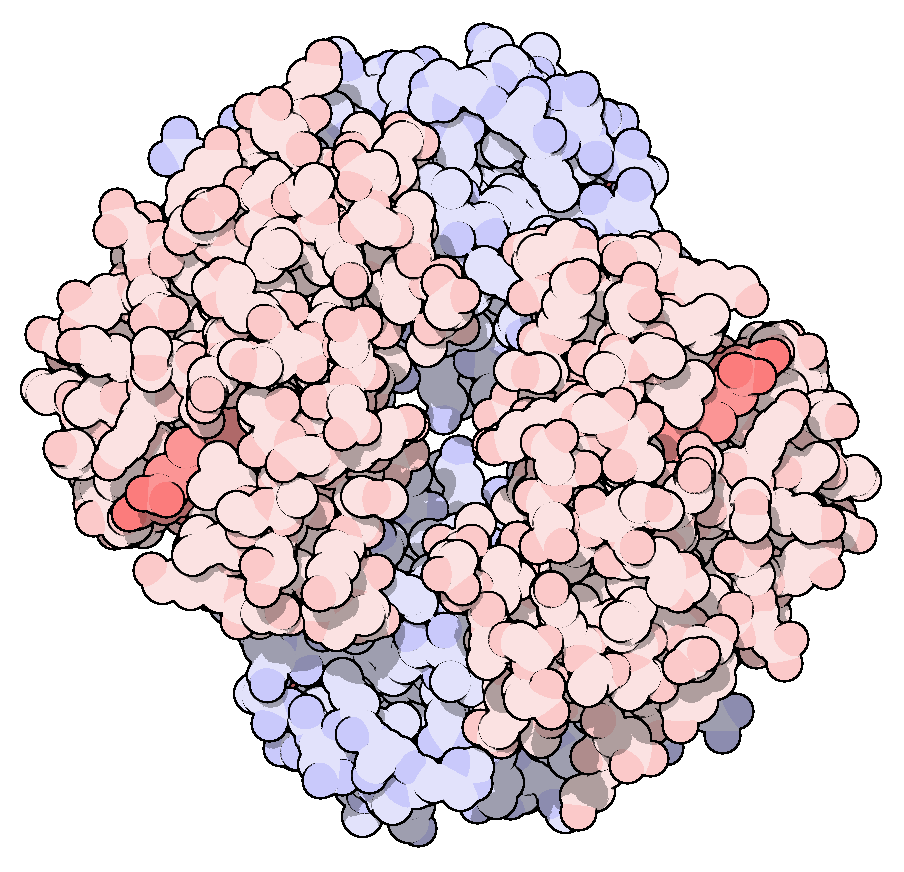
Each globin subunit holds a chemical cofactor called haem. Haem is a flat ring co-ordinating a ferrous (Fe2+) iron atom capable of reversibly binding an O2 molecule. Thus, each haemoglobin molecule can carry up to four oxygen molecules.
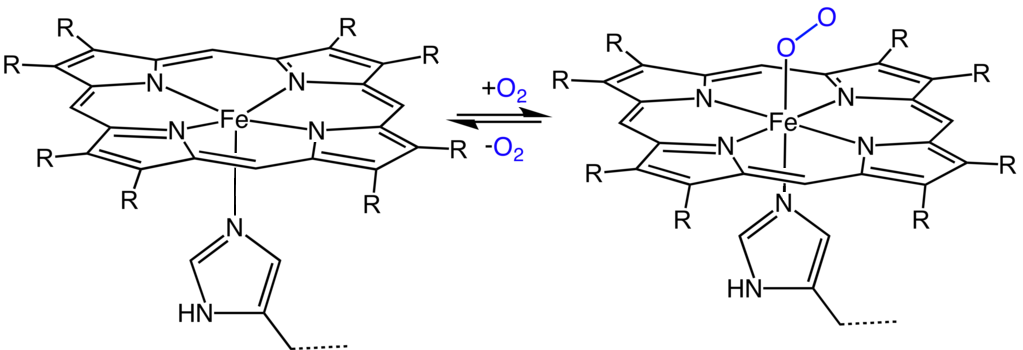
Consider the following problem: If an oxygen-carrying molecule binds oxygen tightly enough to pick up the maximum amount of oxygen in the lungs, how would it be able to let go of that oxygen in the tissues that need it? And if the oxygen-carrying molecule binds oxygen loosely enough to release it in the body’s tissues, how would the oxygen-carrying molecule be able to fully load itself with oxygen in the lungs?
The evolution of haemoglobin in vertebrates has provided clever solutions to this problem. The key to understanding most of these clever tricks: knowing that haemoglobin can change the shape and arrangement of its subunits. The haemoglobin tetramer rapidly switches back and forth between two forms, one that binds tightly to oxygen, and one that binds loosely to oxygen, thousands of times a second. Normally, the two forms are in equilibrium with each other in blood, and this equilibrium can shift either towards the high oxygen affinity (tightly binding) form, or towards the low oxygen affinity (loosely binding) form, depending on various factors described below.
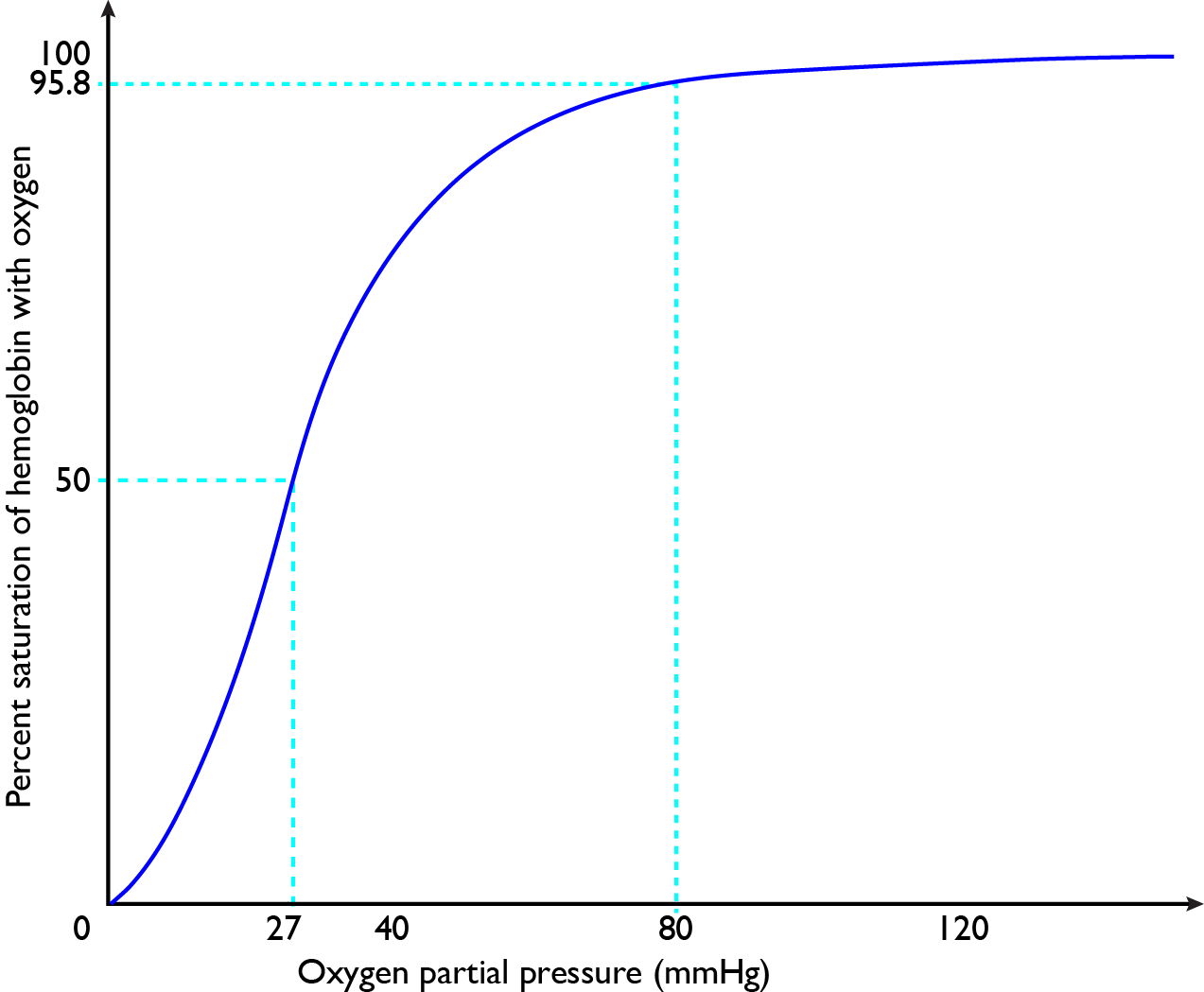
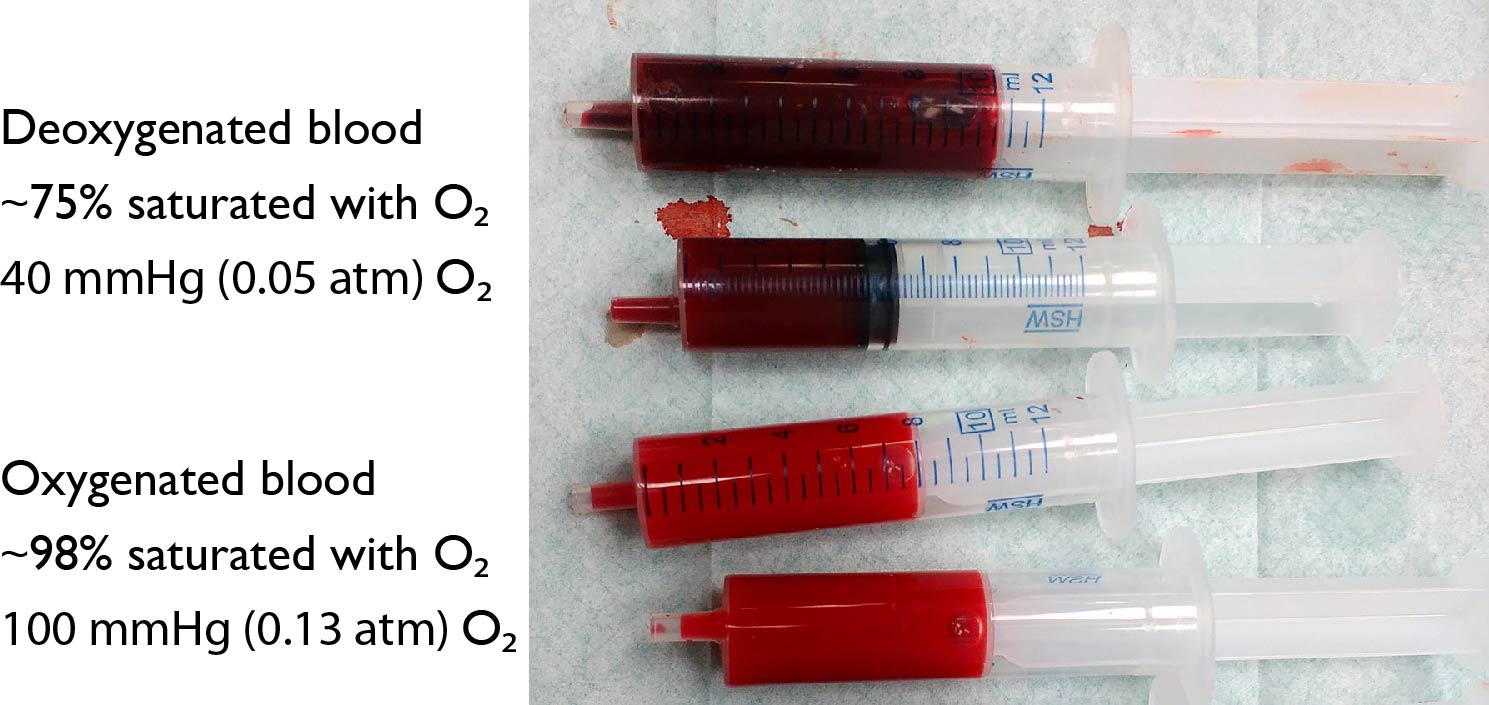
Co-operative binding of O2 to haemoglobin One such factor is oxygen itself. In the absence of oxygen, haemoglobin is mostly in the low oxygen affinity form. When one of the globin subunits acquires an oxygen molecule, the high affinity form becomes more favoured. Thus, binding of an oxygen molecule to each globin subunit makes it easier for the remaining subunits to pick up oxygen. This allows haemoglobin to become fully saturated with oxygen in the lungs, without the need for oxygen binding that’s so tight that it becomes irreversible. Oxygenated blood leaving the lungs in a healthy human at sea level is around 95-99% saturated with oxygen.
The reverse happens, as well: Removing each O2 molecule makes it easier for haemoglobin to let go of the remaining O2 molecules. This allows haemoglobin to release most of its oxygen in tissues without allowing the partial pressure of oxygen in those tissues to drop too low. In a human body at rest, deoxygenated blood returning to the lungs is around 75% saturated with oxygen, but this can drop down to 20% saturation during strenuous exercise. Have close look at Figure 11.13, a graph plotting the amount of oxygen bound by haemoglobin against partial pressure of oxgen in blood: You can see that the curve is S-shaped, such that the steepest part of the curve begins well above zero oxygen. This steep part of the curve overlaps a lot with the 20-75% oxygen saturation range seen in partially deoxygenated blood in humans. As result, a relatively small drop in the partial pressure of oxygen results in the release of a relatively large amount of oxygen from haemoglobin. This helps protect tissues from hypoxia (oxygen starvation; Greek, hupo: under), which causes tissue damage.
11.3 Blood Vessels
11.3.1 Fluid Dynamics (Haemodynamics)
11.3.2 Arteries
11.3.3 Capillaries
11.3.4 Veins
11.3.5 Angiogenesis
11.3.1 Fluid Dynamics (Haemodynamics)
In order to understand circulatory systems, we need to take a look at the factors affecting how and where fluids flow.
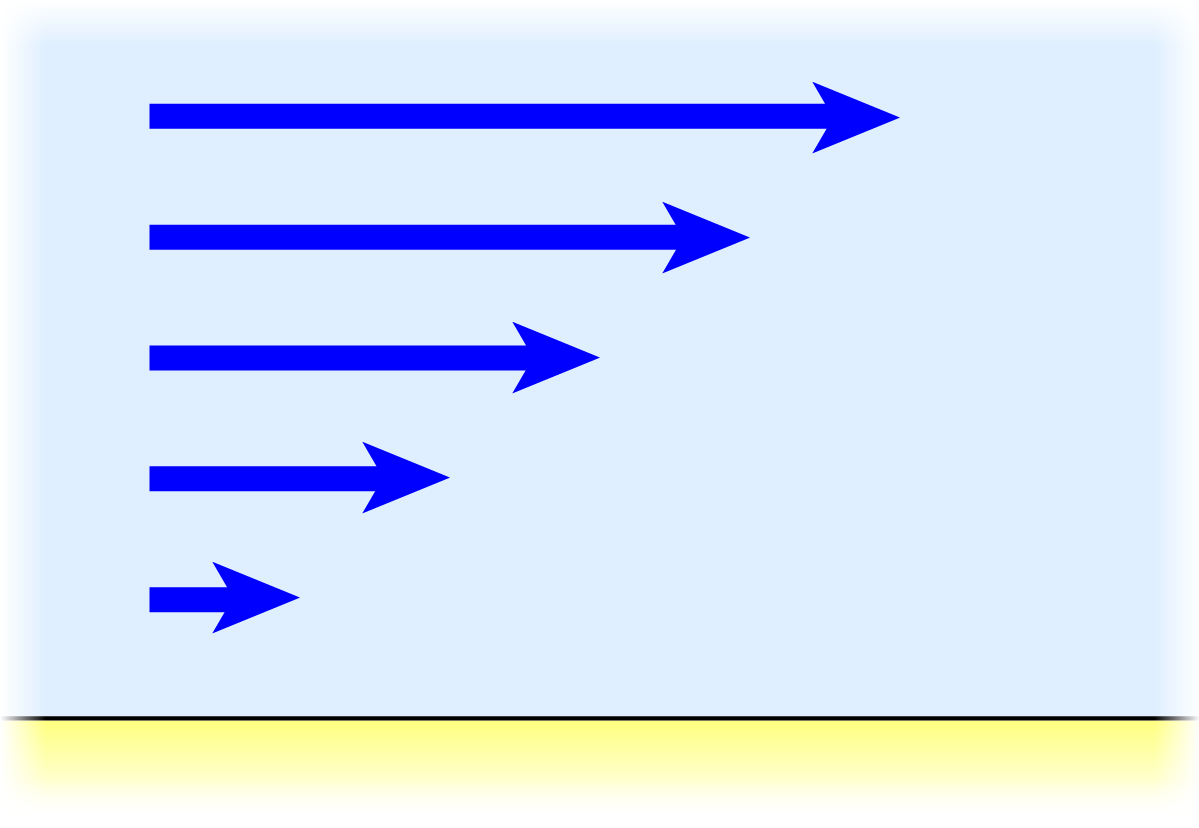
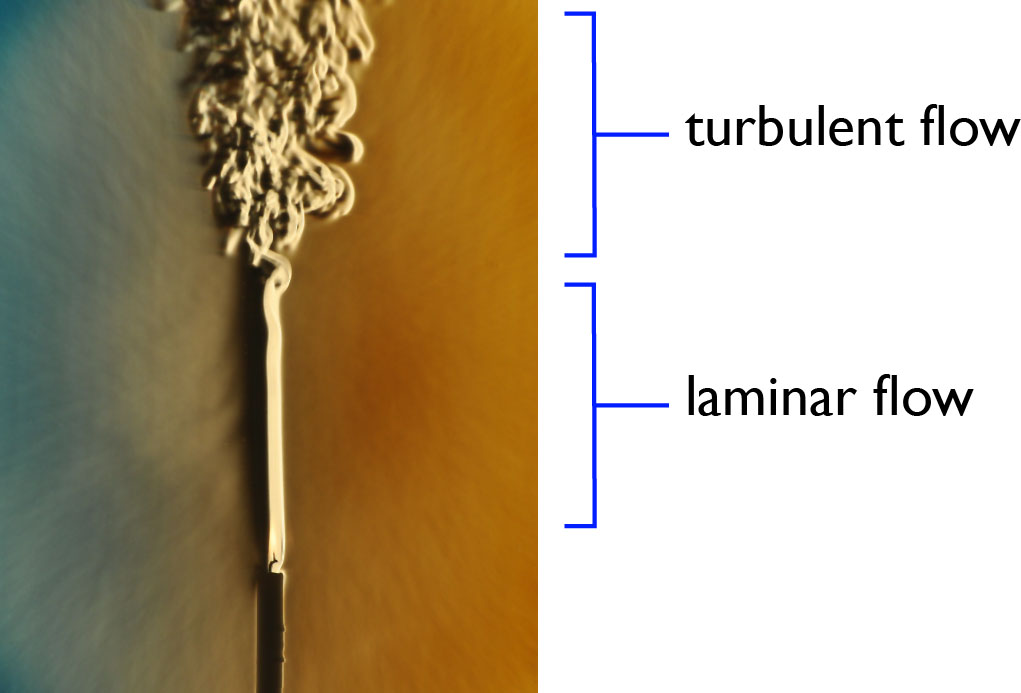
Fluid directly next to a solid surface doesn’t flow, because many of the molecules of the fluid interact with molecules of the surface that are anchored in place. The next layer of molecules out from the surface can slide past, by breaking and re-forming bonds with their neighbours trillions of times per second. Likewise for the next layer of fluid after that. And the next layer. Thus, all other factors being equal, the speed at which a fluid can flow depends on:
- distance from a solid surface, and
- resistance of the fluid to shear
This resistance to shear forces is called viscosity. Viscosity is a measure of the energy needed to move molecules of a fluid past each other. Water has a viscosity of about 0.7 g/(m·s) at human body temperature, blood has a viscosity of 3-4 g/(m·s), and honey has a viscosity around 5000 g/(m·s). Thus, blood is “thicker” than water. The viscosity of blood plasma is only 1.4 g/(m·s), roughly twice the viscosity of water. But the presence of a large volume of suspended objects, namely the red blood cells, means that the shear forces in whole blood are concentrated in barely over half the total volume. As a result of the presence of red blood cells, the viscosity of normal blood is two to three times that of plasma. This limits the amount the amount of red blood cells blood can carry without becoming too viscous.
As already mentioned in the first section of this chapter, circulatory systems in most animals involve flow through a system of tubes or pipes. How is the flow rate affected by the diameter (width) of a tube? Knowing that the resistance to flow is due to viscosity, and that fluid next to a solid surface does not flow, you can calculate how the diameter of a cylindrical pipe affects resistance to flow. If you’re learning introductory calculus, now is a perfect time to get out a pencil and a piece of paper to derive the formula!
Next, we look at the various kinds of tubes or pipes that carry blood in the circulatory system.
11.3.2 Arteries
Arteries are defined as blood vessels that carry blood away from the heart. Arteries leading from the heart branch into smaller and smaller arteries, the smallest ones being called arterioles.
A typical artery has a thin inner lining of endothelial cells, surrounded by connective tissue with a lot of smooth muscle and plenty of elastin fibres, all inside a tough but elastic sheath of connective tissue. The smooth muscle cells are elongated around the circumference of the artery, and spiral around the smaller arteries. When they contract, they shrink the diameter of the artery but don’t change the artery’s length. The smooth muscle cells are connected with each other by gap junctions, allowing them to co-ordinate their contraction. Axons from the autonomic nervous system innervate the artery’s smooth muscle. This is important for controlling blood flow, as discussed later in this chapter.
Arterioles branch into a large number of microscopic vessels called capillaries, where the real business of perfusion of tissues takes place.
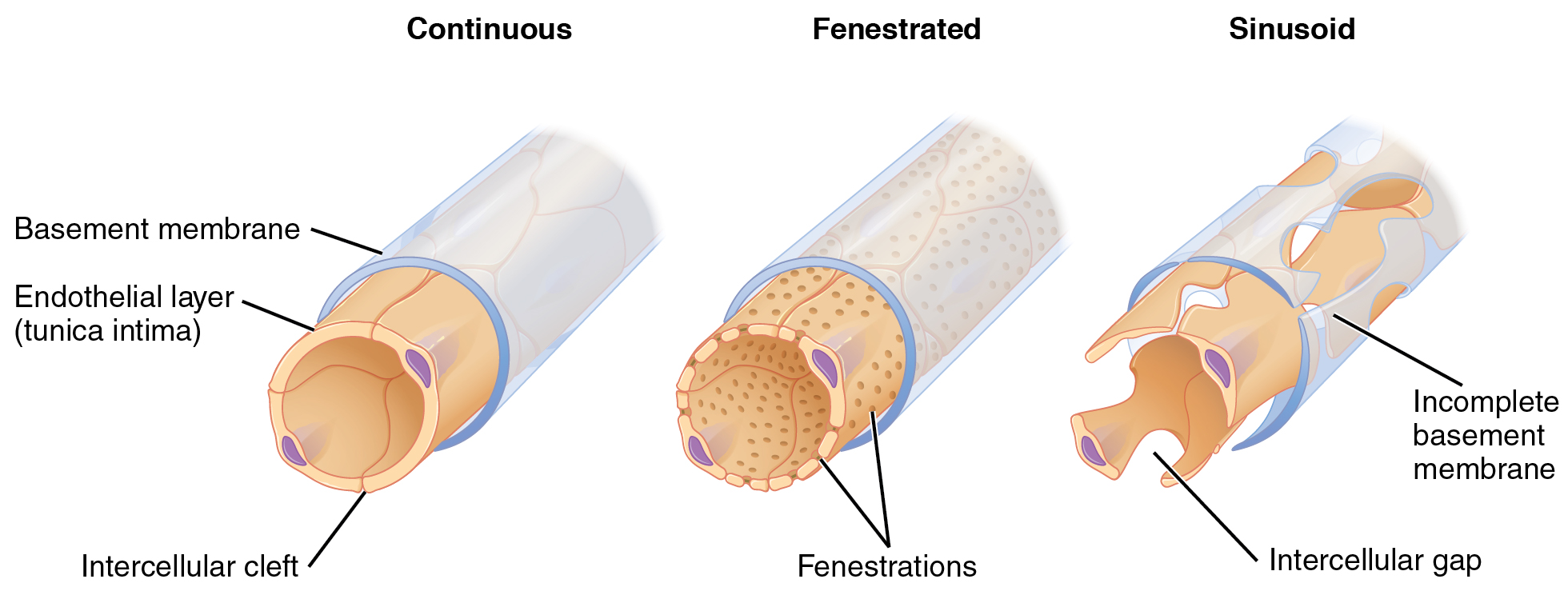
11.3.3 Capillaries
Capillaries are the very smallest and most abundant blood vessels. They are where the blood exchanges materials with the surrounding tissues, so they need to have thin walls to facilitate diffusion, and a high surface area relative to their volume. As a result, they are very narrow, only 5-10 µm across, and have walls only a fraction of a µm thick. Capillaries are just wide enough to allow red blood cells to squeeze through, and even then, the red blood cells have to flex and fold to fit through. Lined end-to-end, the capillaries in an adult human body would stretch one circuit around the Earth’s equator. The surface area of those capillaries add up to a NHL hockey rink, more or less.

Knowing that capillaries are so narrow, you might think that capillaries are the main source of peripheral resistance to blood flow. It would be a good guess, but it would be wrong. The reason is that there are so many capillaries in parallel that the total cross-sectional area is far greater than any other kind of blood vessel. The biggest source of peripheral resistance is the arterioles, accounting for about 2/3 of resistance.
Because the total cross-sectional area of the capillaries is so big, the speed of blood flow through capillaries is much slower than in other blood vessels, ranging from 0.5 millimetre per second to 3 mm/s, with around 1 mm/s being typical. Contrast this speed with the aorta, where blood flows at an average speed of 400 mm/s; the same volume of blood is forced through a hundreds of times smaller cross-sectional area.
The permeability of capillaries varies a lot between tissues. At one extreme are the capillaries of the brain, where tight junctions seal the adjoining edges of the endothelial cells. This results in a blood-brain barrier, where water-soluble molecules and high molecular weight molecules have to be actively transported by the capillary endothelial cells. At the opposite extreme are the capillaries of the liver, spleen, and bone marrow, which have large gaps that can even let cells pass through.
11.3.4 Veins
Veins are defined as blood vessels that carry blood towards the heart. Capillaries join together and feed into the smallest veins, called venules. Venules then join together into larger veins, which in turn join together into the largest veins, which empty into the first chambers of the heart, the atria.
Because the blood has already been through the aterioles and capillaries, blood pressure will have dropped to a low level by the time the blood enters venules. Therefore, veins need an additional way to propel blood towards the heart: Most veins contain one-way valves which consist of a pair of flaps that prevent backflow. Motion of the body alternately squeezes and opens the veins, pumping the blood along with the one-way valves ensuring the blood flows in the correct direction.

A typical vein has a thin inner lining of endothelial cells, surrounded by connective tissue with some smooth muscle and plenty of elastin fibres, all inside a tough but highly elastic sheath of connective tissue. The smooth muscle cells are important for controlling the diameter of the vein. This is much like the structure of arteries, but the wall of a vein is usually much thinner, with less smooth muscle and connective tissue, than the wall of an artery of the same size.
In addition to returning blood towards the heart, veins function as a reservoir of blood. Veins stretch more in response to mild internal pressure than arteries do. The technical term for this stretchiness is compliance. As we’ll see later in this chapter, storage of blood in the veins plays an important role in controlling blood pressure and heart output.
There is one more type of blood vessel: Some blood vessels carry blood from one capillary bed to another without the blood passing through the heart first. These are called portal vessels.
In the chapter on digestion (Chapter 8), we heard about the hepatic portal vein, which carries water-soluble nutrients from the small intestine to the liver. The hepatic portal vein also brings blood from the stomach, gallbladder, large intestine, and spleen to the liver. About three quarters of the blood supply to the liver comes from the hepatic portal vein, the remainder coming from the hepatic artery. Because most substances absorbed by the digestive tract (other than lipids) go directly to the liver, the hepatic portal system results in what is known as first pass metabolism or the first pass effect. This is important for two major functions of the liver:
- processing of nutrients absorbed by the gut, and
- detoxification of harmful substances absorbed by the gut
Because of these functions of the liver, the liver is one of the only places in the body where blood comes into direct contact with tissues other than blood vessel endothelium. Hepatocytes (liver cells) are bathed in blood along extremely permeable blood vessels in the liver called sinusoids. Hepatocytes make up the majority of cells in the liver.
Another important portal system in vertebrate animals is the hypophyseal portal system, which carries neurohormones released by neurons of the hypothalamus at the base of the brain, to the nearby anterior pituitary gland. Many of the hormones produced by the hypothalamus are releasing factors for hormones of the anterior pituitary gland.
11.3.5 Angiogenesis
Angiogenesis is the growth of new blood vessels from existing ones. Endothelial cells can migrate and divide to generate sprouts off of existing vessels, or sometimes the endothelial cells in a vessel can reorganise themselves to split the vessel into two vessels. Blood vessels can also grow in diameter.
Blood vessel growth is important in the growth and maintenance of tissues, in wound healing, and in increasing perfusion of muscle in response to physical exercise. Angiogenesis also contributes to certain diseases: For example, the high metabolic rate and growth rate of tumours means that cancer can only progress to the final stages if there is extremely rapid angiogenesis in tumours. In older people, various diseases can result in loss of vision due to excessive angiogenesis in the retina.
11.4 The Vertebrate Heart
11.4.1 Single and Double Circulation
11.4.2 Heart Anatomy
11.4.3 Co-ordination of Heart Contraction
11.4.4 EKG
11.4.1 Single and Double Circulation
In many animals that have closed circulatory systems, blood is pumped only once each time it circulates around the body. This is called single circulation or single cycle circulation. If the animal has a specialised organ for gas exchange, it’s usually beneficial to have the blood do gas exchange in the respiratory organ before circulating through the rest of the animal’s body. This is the situation in most fish. The disadvantage is that the heart has to produce enough blood pressure to push the blood through at least two beds of small blood vessels: the gills, and the rest of the body.
The alternative is to pump the blood twice per circuit around the body.
11.5 Control of Circulation
11.5.1 Ever-Changing Needs for Blood Flow
11.5.2 Vasodilation and Vasoconstriction
11.5.3 Heart Rate and Stroke Volume
11.5.4 Neural Control of Circulation
11.5.5 Hormonal Control of Circulation
11.5.6 Control of Angiogenesis
11.5.7 Control of Haematopoesis
Suppose a tissue isn’t getting enough blood flow. What factor would be the first to cause problems for that tissue?
If you guessed “oxygen”, you’d most likely be right. The tissues of the body cannot store much oxygen relative to their needs, so they need to be constantly supplied with oxygen.
As we learned in the chapter on respiration (Chapter 10), the energy needs of the whole body varies manyfold from minute to minute. Consequently, the the oxygen needs of the whole body varies ten or even twenty fold from minute to minute. The changes in oxygen demand in individual tissues are even greater.
Therefore, body needs quick ways to change the rate of blood flow.
11.6 The Lymphatic System
11.6.1 Lymph Production
11.6.2 Functions of Lymph
11.6.3 Lymphatic Vessels
11.6.4 Lymph Nodes
11.6.5 Lymphoid Organs
11.6.1 Lymph Production
By definition, in a closed circulatory system, there’s no direct contact between the blood and most of the body’s cells. The interstitial fluid between cells is a separate compartment from the blood in nearly all tissues. In order for the blood to deliver supplies and remove wastes, the walls of the capillaries need to be permeable: Water and most solutes can diffuse through. But cells, platelets, and larger proteins cannot passively cross, not easily, because the pores are too small in the glycocalyx surrounding the endothelial cells and in the diaphragms of the fenestrae (‘windows’) through the endthelial cells. Thus, cells, platelets, and most plasma proteins are kept inside the capillary, while smaller molecules are exchanged with the interstitial fluid surrounding the capillary.
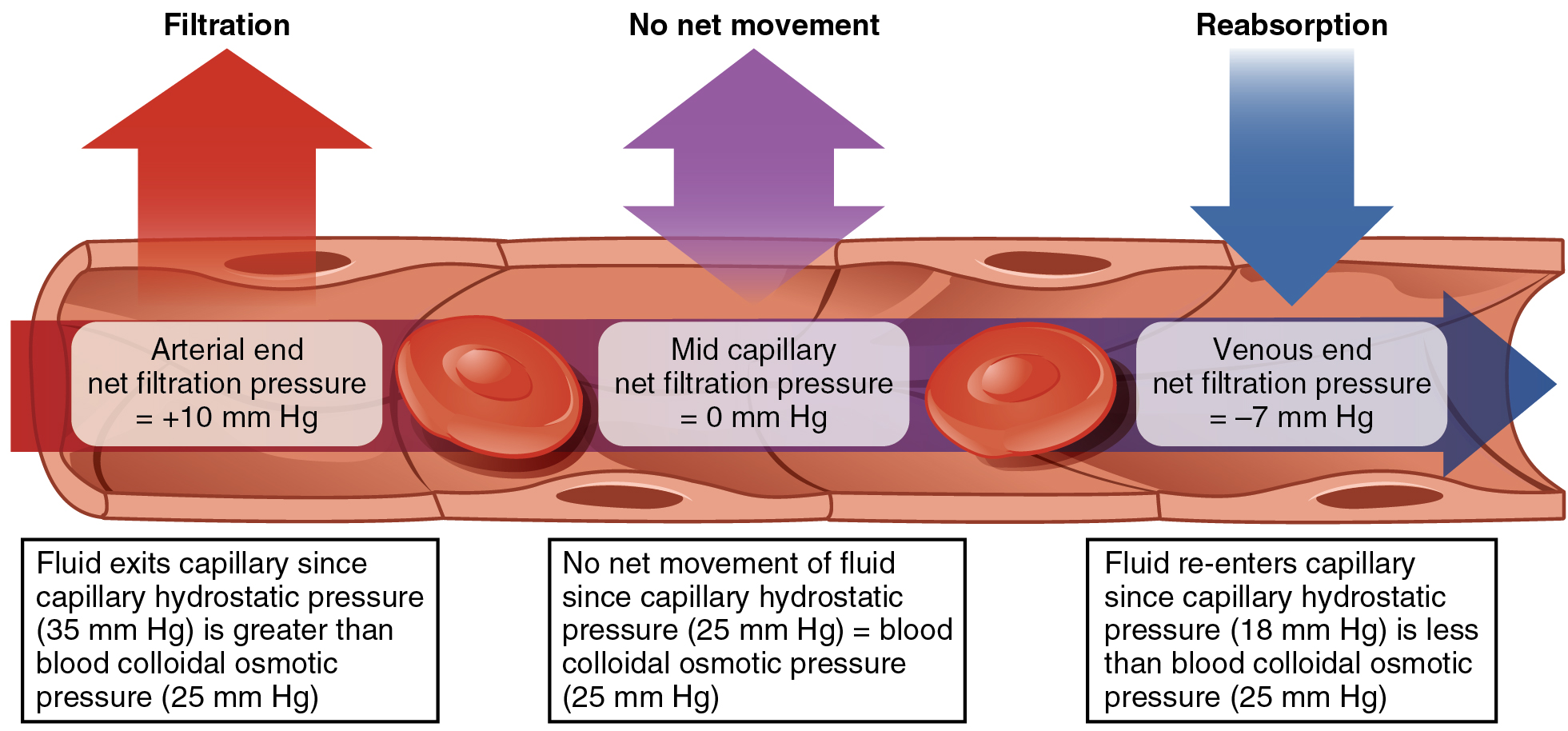
Because of the permeability of the capillary walls for water and small solutes, blood pressure forces fluid through the capillary wall. Remember, blood pressure is the hydrostatic pressure generated by the pumping of the heart. Blood pressure forces most components of plasma to seep through, with the exception of plasma proteins, which are too large to easily get through the capillary walls.
Retention of plasma proteins inside capillaries means that the concentration of dissolved protein – mostly albumin – is much much higher in blood plasma than in the interstitial fluid. Dissolved plasma protein left behind inside the capillary results in a deficit of water in the plasma relative to the interstitial fluid. In other words, plasma proteins have an osmotic effect. Osmotic pressure due to dissolved protein is sometimes called oncotic pressure. The greater oncotic pressure in plasma compared with the interstitial fluid surrounding the capillary is an opposing force against blood pressure, drawing water back into the capillary. Small solutes are indirectly drawn back into the capillary along with the water.
These two opposing forces, the hydrostatic pressure and the osmotic pressure, almost counterbalance each other, but not quite. In the sections of capillary closest to the arterial supply of blood, blood pressure is slightly greater than the oncotic pressure, and fluid leaks out. In the sections of capillary closest to where the blood is drained by venules, oncotic pressure is slightly greater than blood pressure, and fluid is drawn back into the capillary. Overall, loss of fluid from the capillaries into the interstitial fluid is slightly greater than reabsorption. Over the enormous surface area of capillaries in an adult human body, the amount of fluid released by ultrafiltration adds up: roughly 8 litres per day. If you consider that the total volume of plasma is only about 3 litres, this would mean that plasma is filtered through capillary walls at least once every 9 hours, on average.
If this fluid were to accumulate in a tissue, that tissue would swell. Tissue swelling due to accumulation of interstitial fluid is called oedema. To prevent oedema, the body has to drain this excess interstitial fluid. Bony fish, reptiles, amphibians, mammals, and birds have a special set of plumbing: A network of vessels called the lymphatic system drains excess interstitial fluid back into circulating blood.
The smallest vessels of the lymphatic system are called lymph capillaries, but the name is a little bit misleading: At around 50 µm wide, lymph capillaries tend to be much wider than blood capillaries, which are 5-10 µm across in mammals. Another difference is that lymph capillaries are dead-ended, while blood capillaries are connected on both ends with other vessels to form a closed loop. A third difference is that the edges of the lymphatic capillary endothelial cells are loose flaps that act as tiny one-way valves. Endothelial cells of a lymph capillary are shaped like oak leaves, in that each cell has several lobes. These lobes are attatched at the sides to the other endothelial cells through button-like adhaerens junctions, but are free at the tips. When the hydrostatic pressure is higher inside the lymph capillary than outside, the edges seal shut, and when the hydrostatic pressure is lower inside the lymph capillary than outside, protein fibres anchored in the surrounding tissue pull open a gap between the endothelial cells, letting fluid in. In this way, any movement of the surrounding tissues pumps any excess interstitial fluid into the lymph capillaries.
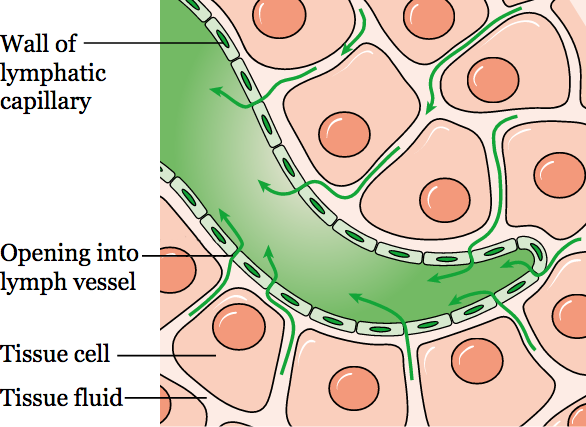
After fluid enters the lymph capillaries from the interstitial fluid, the fluid is called lymph (Latin, lympha: clear water).
11.6.2 Functions of Lymph
The main functions of lymph are:
- returning excess liquid to the circulating blood;
- clearing extracellular particles such as bacteria from tissues;
- helping the body defend itself from invading microbes; and
- transporting digested lipids from the small intestine to the circulating blood.
Each of these functions are worth exploring in more detail.
As mentioned above, the main function of the lymphatic system is to drain excess interstitial fluid into the bloodstream. If the lymphatic system fails or is blocked, massive swelling (oedema) of tissues can result.
Another important function of the lymphatic system is to clear the interstitial fluid of particles that are too large to be taken up by blood capillaries. These include debris from dead cells; foreign matter; damaged, aggregated proteins; cell fragments released by living cells of some tissues; and remnants of HDL, a lipoprotein that carries cholesterol from peripheral tissues to the liver. Most importantly, infectious organisms that appear the interstitial fluid – especially bacteria – are flushed into the lymph. As a result, the lymphatic system has a central role in the immune system. Indeed, many of the cells of the vertebrate immune system are called lymphocytes because they inhabit the lymphatic system.
In Chapter 8, on digestion, you’ll already have encountered a fourth function of the lymphatic system: transport of digested fat. It’s a special case of the lymph’s function in clearing and transporting extracellular particles from the interstitial fluid. The most abundant fats and oils in the diet are triglycerides. In the lumen of the intestine, the enzyme lipase digests triglycerides into fatty acids and monoglycerides. The enterocytes of the intestine absorb the digested lipids and reassemble them into lipoproteins called chylomicrons, containing mostly reconstituted triglycerides. Running down the centre of each villus of the small intestine is one lymph capillary called a lacteal (Latin, lacteus: milky, from lac: milk) which takes up chylomicrons, which are too large (up to one micron[10] in diameter) to fit through the fenestrae of blood capillaries, but can easily enter large pores near the ends of lacteals. In addition to the passive flow of interstitial fluid contaning chylomicrons, lacteals also actively take up chylomicrons by transcytosis through the lacteal endothelial cells.

11.6.3 Lymphatic Vessels
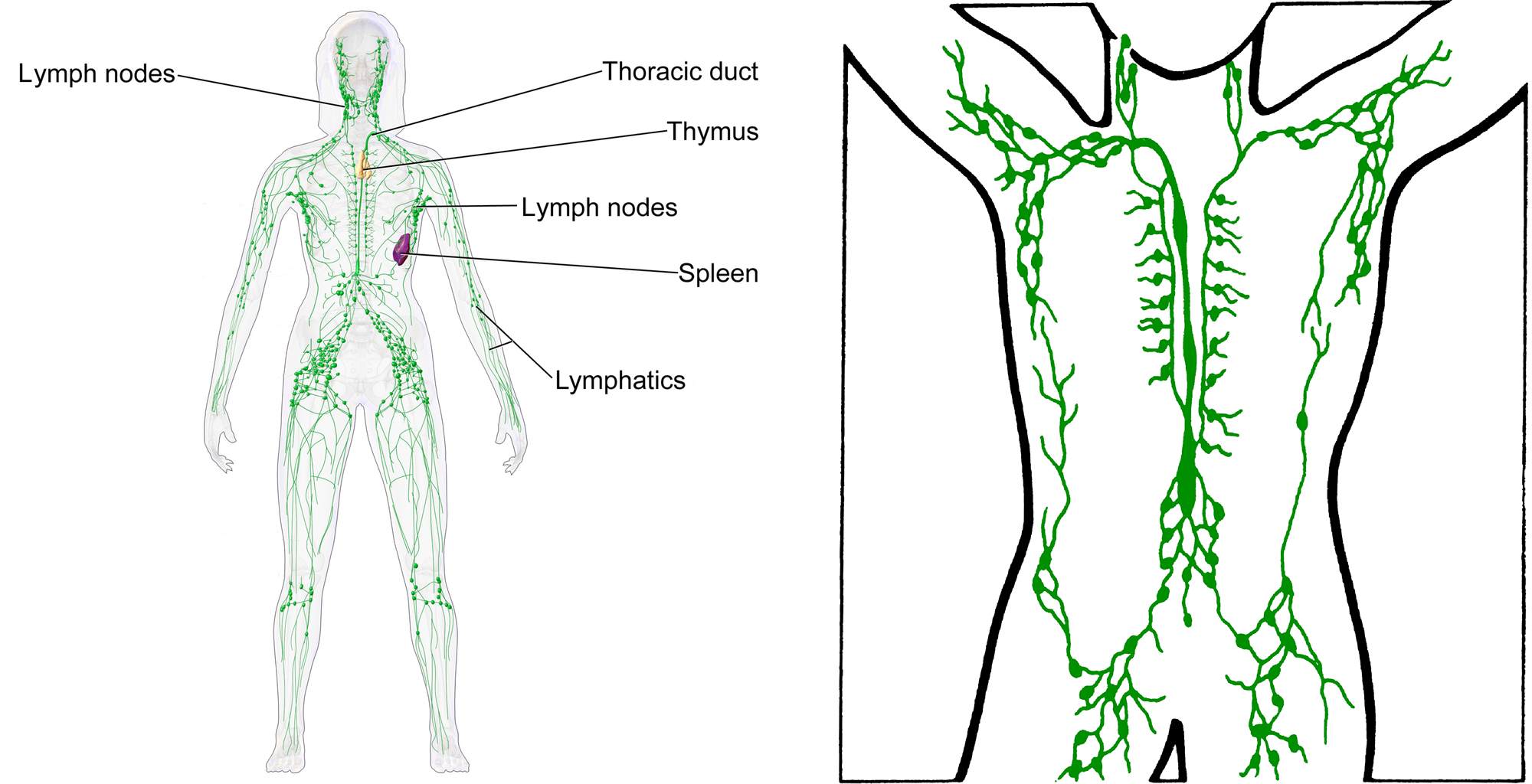
Lymphatic capillaries join together and drain into larger lymphatic vessels, which eventally lead to lymphatic ducts that empty into major veins. In humans, there are two main lymphatic ducts that empty into large veins at the base of the neck. The larger of the two lymphatic ducts is called the thoracic duct.
Lymphatic vessels contain internal one-way valves, much like veins do. The one-way valves help the flow of lymph. As movement of the body compresses and expands the vessels, the chambers defined by the valves act as a series of pumps. In some vertebrate animals, a few of lymphatic vessels form a sheath around large arteries, taking advantage of the pulsing motion of the arteries to move the lymph along. Many vertebrates have ‘lymph hearts’, where thick striated muscle in a single chamber’s wall helps the pumping action. However, mammals lack these, and instead have a thin layer of smooth muscle along the length of many larger lymph vessels to assist pumping of lymph.

Taken literally, the word “elephantiasis” would mean “infection by elephants”. The disease has been known for thousands of years, and still afflicts more than one hundred million people in tropical Africa and Asia today. Tens of millions of people are disfigured. It isn’t elephants that are blocking the lymphatics; The culprits are nematode worms. The larvae are spread by mosquito bites, and grow into adults in the lymphatic system of their victims. The disease gets its name from the swelling of the legs and thickening of the skin, such that the legs look vaguely like those of an elephant.
11.6.4 Lymph Nodes
In mammals and some birds, the lymphatic vessels are interrupted by small capsules of connective tissue housing large numbers of immune system cells. These capsules or nodules of lymphoid tissue are called lymph nodes. In humans, lymph nodes are usually range from 5 mm to 20 mm in length.
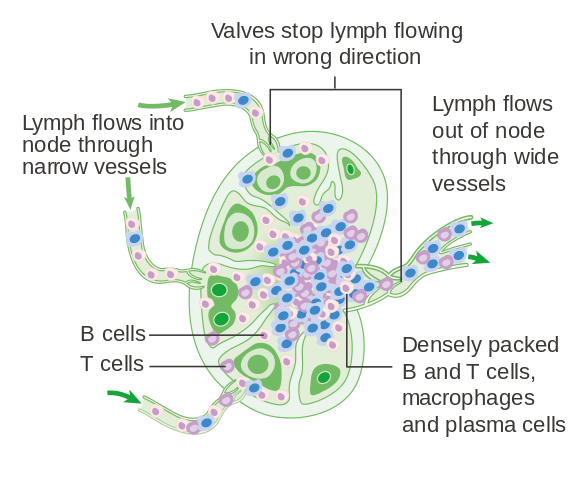
During an infection, the lymph nodes can swell dramatically due to proliferation of immune system cells. Most people will have had temporarily swollen lymph nodes due to the common cold at some point in their lives.
11.7 Summary
- In all but the smallest animals, diffusion is too slow for communication and transport throughout the animal body.
- Instead, bulk flow of liquids is important in the vast majority of animals.
- Examples of items that need to be transported around the body are oxygen, nutrients, water, carbon dioxide, waste products, hormones, cells of the immune system, and components needed for clottng.
- In larger, more complex animals, a system of pipes or tubes (vessels) makes bulk flow easier.
- A muscular pump, called the heart, pumps this circulatory fluid.
- In animals with a closed circulatory system, vessels entirely enclose the main circulatory fluid, called the blood, which does not come in direct contact with most of the tissues of the body.
- Almost half of the volume of blood consists of smooth, flexible, tough cells packed with the oxygen-carrying protein haemoglobin. These are the erythrocytes (red blood cells).
- …
11.8 Suggested Readings
Fluids and Transport, in Anatomy & Physiology, OpenStax CNX.
http://cnx.org/contents/FPtK1zmh@8.86:XC_BBOMZ@5/Introduction
from Anatomy & Physiology, OpenStax CNX. June 14, 2017 http://cnx.org/contents/14fb4ad7-39a1-4eee-ab6e-3ef2482e3e22@8.86
11.9 Glossary
Acidosis – The blood is more acidic than normal, meaning the concentration of hydrogen ions is high, or equivalently, the pH is low. Blood pH below about 7.35 is typically considered to be acidosis. Often due to excess carbon dioxide in the blood.
Alkalosis – The blood is more alkaline than normal, meaning the concentration of hydrogen ions is low, or equivalently, the pH is high. Blood pH over 7.45 is typically considered to be alkalosis.
Anastomosis – A cross-connection of vessels. Can range from a simple shunt between two vessels, to a net-like pattern of vessels.
Angiogenesis – Growth of new blood vessels from existing blood vessels.
Aorta – The largest artery of the body, leading from the left ventricle to the systemic circulation.
Aortic arch – The part of the aorta that curves, leading from the ascending aorta to the descending aorta in bipedal animals such as humans.
Arteriole – A tiny artery. Arterioles are the smallest arteries, connecting larger arteries to capillaries.
Artery – Blood vessel that carries blood away from the heart, towards capillaries.
Atrioventricular node – A group of cells in the heart’s electrical conduction system, the AV node creates a delay before sending the signal to contract to the ventricles. The AV node is located in the interatrial septum at the base of the right atrium, near the septum between the two ventricles.
Atrioventricular valve – One-way valve between an atrium and a ventricle in the heart, preventing blood from flowing back into the atrium when the ventricle contracts. See mitral valve and tricuspid valve.
Atrium – Chamber of heart that receives blood from the veins and delivers it to a ventricle.
AV node – Atrioventricular node.
AV valve – Atrioventricular valve.
B cell – B cells are white blood cells that produce and secrete antibodies. B cells also present antigens, and produce cytokines. They are a type of lymphocyte.
Bicuspid valve – Valve consisting of two flaps. The mitral valve is usually the only bicuspid valve in the human heart.
Blood – The main circulating liquid in animals that have a closed circulatory system.
Blood-brain barrier – A set of selective barriers separating the capillary blood supply from the central nervous system. Considered to be distinct from the blood-cerebrospinal fluid barrier and the blood-retina barrier.
Blood island – Blood islands are the points of origin of blood vessels and red blood cells for the early stages of the embryo, and are located mostly in tissues surrounding the embryo.
Blood pressure – Fluid pressure of blood. The most common blood pressure measurement is pressure against the walls of larger arteries, expressed as millimetres of mercury (mmHg) relative to atmospheric pressure, the maximum during systole and minimum during diastole, for example 115/75.
Bradycardia – Slower than average heart rate.
Bundle of His – Part of the heart’s electrical signal conduction system that carries impluses from the atrioventricular node towards the ventricles.
Bursa of Fabricius – An organ in young birds that is the main site of B cell maturation.
Capillary – The narrowest blood vessels, only 5 to 10 microns across. Their walls are extremely thin, allowing exchange of many substances between the blood and the surrounding tissues.
Capillary filtration – Filtering of materials through the capillary walls; The capillary endothelium poses a barrier to cells and to macromolecules such as proteins larger than 10 nm, while low molecular mass solutes and water can pass through relatively unimpeded.
Carbon dioxide – CO2.
Carbonic anhydrase – Enzyme that greatly speeds up the interconversion of carbon dioxide with bicarbonate in water:
CO2 + H2O ↔ HCO3– + H+.
Cardiac – Of the heart.
Cardiac shunt – Diversion of blood from pulmonary circulation to systemic circulation during diving and breath-holding in those reptiles that have a three-chambered heart.
Carotid artery – Artery that supplies blood to the head.
Cerebrospinal fluid – The clear liquid bathing the central nervous system.
Chorda tendina – Tendon or “heart string” holding a flap of a heart valve in place against backwards flow of blood.
Chyle – The fat-containing liquid that the small intestine produces and sends through lacteals into the lymphatic system. Chyle has a milky appearance because it is a colloid of the fat-carryig chylomicrons.
Chylothorax – Leakage of chyle-containing lymph into the pleural cavity (the body cavity containing a lung).
Circle of Willis – A circle of arteries cross-connecting the arteries supplying blood to the brain. This anastomosis creates a redundancy of blood supply to the brain so that ischemia is less likely if one vessel is blocked.
Clot – A gel or solid that forms from blood in response to injury. Blood clots function to stop bleeding and seal a wound.
Coelom – Liquid-filled body cavity surrounding the gut and several other internal organs and lined with a sheet of mesodermal cells.
Complement – The complement system is a set of dozens of proteins, most of them in the blood plasma, that function together in the immune system to mark and eliminate pathogens and foreign objects.
Coronary artery – Artery that supplies the myocardium with oxygen and nutrients.
Countercurrent – Neighbouring currents flow in opposite directions. Countercurrent flow results in highly efficient transfer of materials between two fluids by diffusion, and also results in highly efficient transfer of heat.
CSF – See cerebrospinal fluid.
Cyanosis – A slightly blue colour of mucous membranes and skin due to high deoxyhaemoglobin levels. Cyanosis becomes noticeable when blood oxygen is less than roughly 70-80% of saturation.
Cytoglobin – A globin found in many cells of the body.
Dendritic cell – A type of antigen-presenting cell in the immune system of mammals, birds, and reptiles.
Deoxyhaemoglobin – Haemoglobin without O2. See cyanosis and oxyhaemoglobin.
Depulsation – Smoothing out of the difference between peak systole blood pressure and diastole blood pressure, by elastic arteries.
Diastole – The part of the hearbeat cycle when the ventricles relax and the heart re-fills with blood.
Diastolic pressure – The lowest blood pressure in arteries between two heart contractions.
Dilation – Increase in inner diameter, for example when air passages or blood vessels expand to get wider. Dilation of a tube lowers resistance to flow.
Double circulation – Blood circulation where the oxygenated blood is pumped through systemic circulation, and the deoxygenated blood pumped a second time through the respiratory circulation. Common in air-breathing vertebrates. Contrasts with single circulation.
DPG – 2,3-diphosphoglycerate. An allosteric regulator of haemoglobin in red blood cells.
Ductus arteriosus – A blood vessel connecting the pulmonary artery with the aorta in the fetus of mammals, shunting blood wawy from the nonfunctional lungs. Health problems can result if the ductus arteriosus fails to close shortly after birth.
Dural sinus – Dural sinuses are chambers in the dura mater (part of the meninges) covering the brain which collect venous blood from the brain.
ECG – Electrocardiogram.
Edema – Accumulation of fluid in a tissue.
EKG – Electrocardiogram. Alternate spelling of ECG.
Elastic – Able to store mechanical energy when stretched, such that the material passively returns to its original shape when the stretching force is no longer present.
Elastic recoil – Return to original shape after external force is removed. See elastic.
Electrocardiogram – Recording of voltages across the torso of the body to diagnose heart function.
Embolism – A piece of solid or gel that has become lodged in a blood vessel, blocking blood flow.
Embolus – A piece of solid or gel in the blood, large enough to block blood flow if it gets lodged in a vessel.
Endocardium – The inner lining of the heart.
Epithelium – A sheet of cells lining the inner or outer surface of various organs, glands, and vessels. One of the basic tissue types of the animal body.
Erythrocyte – Red blood cell, full of haemoglobin, and functions to carry oxygen.
Fibrinogen – A blood plasma protein that clotting converts into fibres of a blood clot.
Foramen ovale – An opening through the atrial septum, which is present in the fetus of mammals.
Frank-Starling effect – Increasing the volume of blood refilling the ventricle by the end of diastole increases the force of heart contraction during the following systole. Individual heart muscle cells respond to stretch by increasing their force of contraction.
Gastrovascular cavity – A gut that extends throughout the body, allowing it to fulfill some of the functions of a circulatory system. Often highly branched. Seen in some invertebrate animals.
Globin – Protein of a diverse family of O2-binding proteins that contain haem and iron.
Glycocalyx – A layer of long-chain, branched polysaccharides covalently attached to the outside surface of cells, forming a dense gel that filters and protects.
Heart – A pump that pumps blood. Consists of a special kind of muscle called cardiac muscle.
Heart rate – The frequency of heart beats (contractions).
Haem – The oxygen-binding cofactor in globins such as haemoglobin. Contains an atom of iron. Also spelled heme.
Haemoaemocyanin – A blue protein that carries O2 in the haemolymph of molluscs, crustaceans, and some spiders, scorpions, and centipedes. Haemocyanins are unrelated to globins, and contain copper, not haem and iron.
Haemoglobin – Abundant globin of red blood cells, the main carrier of O2 in many animals.
Haemolymph – The main circulating liquid in animals that have an open circulatory system.
Haematocrit – The proportion of blood volume taken up by red blood cells. Usually expressed as a percentage.
Haematopoiesis – Formation of blood cells.
Hepatic portal vein – Blood vessel acting as a portal “vein” from capillary beds in the intestine to capillary beds in the liver.
Hypercapnea – An abnormally high concentration of carbon dioxide in the blood.
Hypoxia – A lower than normal oxygen level in the body.
Interstitial fluid – The extracellular liquid bathing the cells of internal solid tissues of the body. Also known as tissue fluid.
Ischemia – Loss of blood flow to a tissue.
Jugular vein – Large vein in the neck.
Lacteal – Chyle-collecting lymphatic vessels in the lining of the small intestine.
Leucocyte – White blood cell.
Lymph – The liquid that carries material from the interstitial fluid to the bloodstream in animals that have a closed circulatory system.
Lymph heart – A muscular pump that pumps lymph, found in many vertebrate animals, but not mammals.
Lymph node – Small organ of the immune system connnected to lymphatic vessels, home to many lymphocytes.
Lymphatic capillary – Lymph capillaries are the smallest lymphatic vessels, and are the site where the lymphatic system collects interstitial fluid and plasma ultrafiltrate.
Lymph duct – A duct that drains lymph into a major vein. Humans have two lymph ducts: the thoracic duct, and the right lymphatic duct.
Lymphocyte – Lymphocytes are a category of white blood cells that are also abundant in the lymph. Lymphocytes include B cells, T cells, and NK cells.
Macrophage – An amoeba-like type of white blood cell that engulfs (phagocytoses) pathogens, other foreign objects, and other materials the body needs to recycle or remove.
Marrow – A soft tissue inside larger bones, some of which is haematopoietic.
Medulla oblongata – Portion of the brainstem that controls several vital functions of the autonomic nervous system, including control of breathing, control of heart rate, control of blood pressure, and several reflexes of the respiratory system and upper gastrointestinal tract.
Meninges – A set of tissue membranes enclosing the central nervous system.
Methaemoglobin – Haemoglobin where the iron is oxidised to the ferric (Fe3+) ion from the ferrous (Fe3+) ion. In healthy individuals, methaemoglobin is normally only a small fraction of total haemoglobin.
Microcirculation – Blood circulation through the smallest vessels: arterioles, capillaries, and venules.
Mitral valve – The bicuspid valve that prevents blood flow back from the left ventricle to the left atrium.
Myocardium – Muscle tissue of the heart.
Nitric oxide – NO.
Oncotic pressure – Pressure due to the difference in concentration of water between blood plasma and plasma ultrafiltrate. Most of the oncotic pressure is due to dissolved protein that is retained in the blood plasma inside capillaries. See capillary filtration.
Oxygen – O2.
Oxyhaemoglobin – Haemoglobin loaded with O2.
Pacemaker – Any structure that generates a rythmic, regularly repeating electrical impulses. Natural pacemakers consist of cells whose plasma membrane voltage cycles without any external input. See Chapter 1.
Partial pressure – The pressure exerted by one gas in a gas mixture. See Dalton’s law. Also a measure of the concentration of a gas dissolved in a liquid. See Henry’s law.
Perfusion – The passage of circulatory fluid through an organ or tissue.
Peripheral resistance – Resistance to blood flow through peripheral tissues. Also called systemic vascular resistance.
Pericardium – A bag-like membranous tissue that enclose the heart, consisting of a fibrous pericardium on the outer surface of the heart, pericardial fluid outside the fibrous pericardium, and a serous pericardium enclosing the pericardial fluid.
Peyer’s patch – Peyer’s patches are lumps of lymphoid tissue on the intestine.
Placenta – An organ that exchanges dissolved materials between mother and embryo or fetus. The placenta is also an important source of hormones during pregnancy.
Plasma – The extracellular liquid of blood.
Platelet – Platelets are cell fragments in blood important for blood clotting in mammals. Platelets are also sometimes called thrombocytes.
Pons – The part of the brainstem between the medulla and the midbrain.
Portal vein – Blood vessel, not a true vein, that connects capillary beds between two different organs.
Postcava – Equivalent to the inferior vena cava.
Precava – Equivalent to the superior vena cava.
Pulmonary artery – Artery that carries blood to the lungs. Unlike other arteries, the pulmonary arteries carry deoxygenated blood.
Pulmonary trunk – The short and wide pulmonary artery directly connected to the heart. It splits into the right pulmonary artery and left pulmonary artery.
Pulmonary valve – A tricuspid valve that prevents blood from flowing back from the pulmonary artery to the right ventricle.
Purkinje fibre – Elongated cell specialised for rapid conduction of electrical impulses in the ventricle walls.
Red blood cell – See erythrocyte.
Rete mirabile – A densely-packed complex of arteries and veins close to each other, allowing countercurrent exchange of heat or water or solutes.
SA node – Sinoatrial node.
Semilunar valve – Valves of the heart that prevent backflow of blood from the arteries back into the ventricles. See aortic valve and pulmonary valve.
Septum – A wall separating two chambers of the heart.
Serum – The clear liquid that separates out when blood clots, serum contains all the compenents of blood other than the cells and most of the clotting factors.
Serum albumin – The most abundant protein in blood plasma of vertebrate animals, serum albumin carries fatty acids and the more hydrophobic hormones.
Single circulation – Blood circulation where blood is not re-pumped between the respiratory capillary beds and the systemic capillary beds. Common in bony fish. Contrasts with double circulation.
Sinoatrial node – A group of cells in the heart’s electrical conduction system, the SA node includes the main pacemaker of the heart. The SA node is located in the wall of the right atrium, next to the superior vena cava.
Shunt – Any structure or mechanism that allows blood to bypass its expected path of circulation.
Spiral valve – Structures on the inner surface of a ventricle that keep oxygenated blood and deoxygenated blood flows separate. Seen in some animals whose heart has only one ventricle.
Spleen – An organ that filters blood and stores red blood cells, the spleen is also important for the immune system as a site of lymphoid tissue.
Stroke – Brain damage due to interrupted blood flow, either due to ischemia or due to internal bleeding.
Stroke volume – The volume of blood pumped by each contraction of the left ventricle.
Systole – The part of the heartbeat cycle when the ventricles contract, ejecting blood into the arteries.
T cell – T cells are a type of white blood cells that perfrom various functions in the immune system. They are a category of lymphocyte.
Tachycardia – Faster than average heart rate.
Thoracic duct – The larger of the two lymph ducts, draining chyle and lymph into the brachiocephalic vein.
Thrombocyte – Blood cells important for blood clotting in vertebrate animals other than mammals, where platelets perform the same functions.
Thrombosis – Embolism due to a blood clot.
Thrombus – See clot.
Thymus – A major lymphoid organ in the neck that is the main site of T cell maturation.
Tonsil – A patch of lymphoid tissue at the back of the throat (the tonsil most familiar to most people), or the back of the nasal cavity (where it is also known as the adenoid).
Trabecula – Projection of heart tissue into chamber of ventricle, improving oxygenation of heart muscle.
Tricuspid valve – A valve consisting of three flaps.
Tricuspid valve – The tricuspid valve (see definition above) that prevents blood flow back from the right ventricle to the right atrium.
Tunica adventitia – The tough, elastic outer layer of arteries and veins, containing a layer of the fibrous protein collagen. Also known as the tunica externa.
Tunica intima – The thin innermost layer of arteries and veins, consisting of a layer of endothelial cells one cell thick and their basal lamina.
Tunica media – The middle layer of arteries and veins, containing elastic fibres, and in most arteries and some veins, smooth muscle.
Ultrafiltration – Filtration through a semipermeable membrane, such that microscopic colloidal particles and molecules of a certain size or larger are concentrated on one side and excluded on the other side of the membrane.
Umbilical cord – Cord connecting a fetus to the placenta, containing one or more veins bringing oxygen and nutrients to the fetus, and one or more arteries bringing wastes to the placenta.
Vagus nerve – The tenth cranial nerve and one of the most important nerves of the autonomic nervous system.
Vascular resistance – Resistance to blood flow through a set of tissues.
Vasoconstriction – Constriction (narrowing) of blood vessels by smooth muscle contraction. Vasoconstriction increases resistance to flow.
Vasodilation – Dilation (widening) of blood vessels by smooth muscle relaxation. Vasodilation reduces resistance to flow.
Vein – Blood vessel that carries blood towards the heart, away from capillaries.
Vena cava – A large vein returning deoxygenated blood to the heart. Mammals, birds, and some reptiles have two venae cavae.
Ventricle – Chamber of heart that provides the main pumping force.
Venule – A tiny vein. Venules are the smallest veins, connecting capillaries to larger veins.
- A quick reminder: The term homeostasis refers to keeping a constant internal environment. ↵
- A quick reminder: The term metabolism refers to the main chemical reactions that maintain life. ↵
- peristalsis ↵
- ‘tetramer’ (Greek, téttares: four; méros: part) is the term for a structure with four subunits ↵
- Haemoglobin would make the blood much too viscous ↵
- The pulmonary artery and umbilical cord arteries. ↵
- Capillaries have to be wide enough for blood cells to squeeze through. Erythrocytes in mammals lack nuclei, so they can be smaller than erythrocytes in most amphibians, fish, reptiles, and birds. ↵
- Arteries are exposed to much higher blood pressures than veins. ↵
- The pulmonary artery and umbilical cord arteries. ↵
- 1 micron is 1/1000 of a millimetre, or 1000 nanometres ↵

