13. Homeostasis
Homeostasis
- 13.1 Introduction
- 13.2 Pathways of Homeostatic Control
- 13.3 Feedback Loops
- 13.4 Body Temperature Regulation
- 13.5 Control of Blood Glucose
- 13.6 The Ovarian Cycle
- 13.7 Homeostasis at the Cellular Level
- 13.8 Summary

13.1 Introduction
Control of the physical and chemical processes that occur at cell and tissue levels is essential to normal functioning of the animal body. These processes are continuously challenged as individuals are normally exposed to factors that affect constancy of the composition of the internal media, which include changes in the diet, level of physical activity, and environmental conditions such as ambient temperature or light exposure and intensity.
Constancy of the internal media is assured by a property of the body termed homeostasis (Greek, hómoios: in like manner; stasis: standing still), which continuously regulates the variables to assure normal functioning of all tissues and organs. Variables under homeostatic control include body temperature, blood pressure, pH of the extracellular fluid, carbon dioxide, oxygen, osmotic pressure, blood sugar level, and concentrations of ions such as sodium, potassium and calcium. These variables are constantly kept within certain pre-set limits called the homeostatic range.
Mechanisms of homeostatic control can be observed at the level of cell, tissue, and organ, as well as in the organism as a whole. Cells and tissues depend on maintaining a relatively narrow level of internal media conditions in order to function normally, whether the processes take place inside the cell or in the interstitial fluid bathing the cells. As such, the body continuously expends energy to tightly regulate the concentrations of metabolites and small molecules at all levels.
Overall, at high energy cost homeostatic mechanism compensates for changes that affect the internal variables, regardless of the internal and external factors that affect stability of the internal media. The patterns of homeostatic control include:
- feedback regulation,
- feed-forward regulation, and
- conditioned stimulus.
13.2 Pathways of Homeostatic Control
The main components of a homeostatic controlled system include, at a bare minimum:
- a stimulus,
- a receptor,
- a centre of control, or integrator, and
- an effector.
The stimulus, receptor, control centre, and effector work together in a feedback loop.
A stimulus is a signal, such as a chemical or physical cue generated inside of the body, or outside of the body like ambient temperature or duration and intensity of light.
A receptor is the sensing component that monitors and responds to internal or external changes. Through the sensory system, the environment influences regulatory organs in the body that exchange signals with target organs that control homeostasis. Receptors include photoreceptors, chemoreceptors, thermoreceptors, and mechanoreceptors. Signals include physical signals like radiation, and chemical signalling molecules like hormones, growth factors and neurotransmitters. Those signals regulate body physical and chemical variables, such as blood pressure, body temperature or concentration of metabolites.
A control centre includes an integrator that compares signals detected by the sensor to the set point for the variable to be regulated. The set point is the normal value for the variable to be regulated. Control centres compensate for the changes in the variable. Homeostatic control centres are located in the hypothalamus as well as in organs in the periphery, such as the renin–angiotensin system in the kidneys that control blood pressure.
An effector is the target acted on to bring about the change back to the normal state of the set point. Effectors include muscle tissue and glands that compensates for deviations between sensed value and the set point value.
At the cellular and molecular level, receptors include nuclear receptors that bring about changes in gene expression through up-regulation or down-regulation, membrane receptors, enzymes and ion channels. These control mechanisms include substrate supply for enzymatic reactions, activation or inhibition of individual enzymes and receptors, synthesis and degradation of enzymes, and molecular cell compartmentalization.
13.3 Feedback Loops
Feedback is the response of a system that influences the activity of a reaction by the end products of that reaction. In other words, feedback is the self-control of a biological reaction mediated by its end product. Two main types feedback loops control homeostasis: positive feedback loops and negative feedback loops:
- In a positive feedback loop, a change in intensity of a stimulus causes further changes on the same stimulus. The variable under control has the ability to amplify itself, thus in a positive feedback loop the stimulatory signal target a tissue and the product of the target tissue leads to an increase in the intensity of the response.
- In a negative feedback loop, a change in intensity of a stimulus causes inhibition of the same stimulus. Negative feedback loop occurs when a stimulatory signal targets a tissue and the product of the target tissue leads to a decrease in the intensity of a response to a stimulatory signal. In this way, a negative feedback loop brings a system closer to stability.
Although some examples of positive examples of positive feedback can be described, negative feedback loops are the most common mechanisms for maintaining a steady stable state of the animal body’s internal media.
Organs that maintain homeostasis
Which organs function to maintain homeostasis of the body as a whole?
The short answer: All of them!
A longer answer: While every organ makes an important contribution to homeostasis of the body, some organs that are specialised for communication with the rest of the body are particularly important for homeostasis:The organs that maintain homeostasis include the nervous system, which working in tandem with the endocrine system form what is called the neuroendocrine system. The nervous system detects external and internal changes that impact the internal media and respond to such events by transmitting signals to and from different parts of its body through the endocrine systems. In addition, signals through the autonomic nervous system which control non-voluntary body functions, such as the liver that regulates metabolism, the pancreas that regulates blood sugar levels, and the kidneys that regulate body fluids composition and blood pressure.
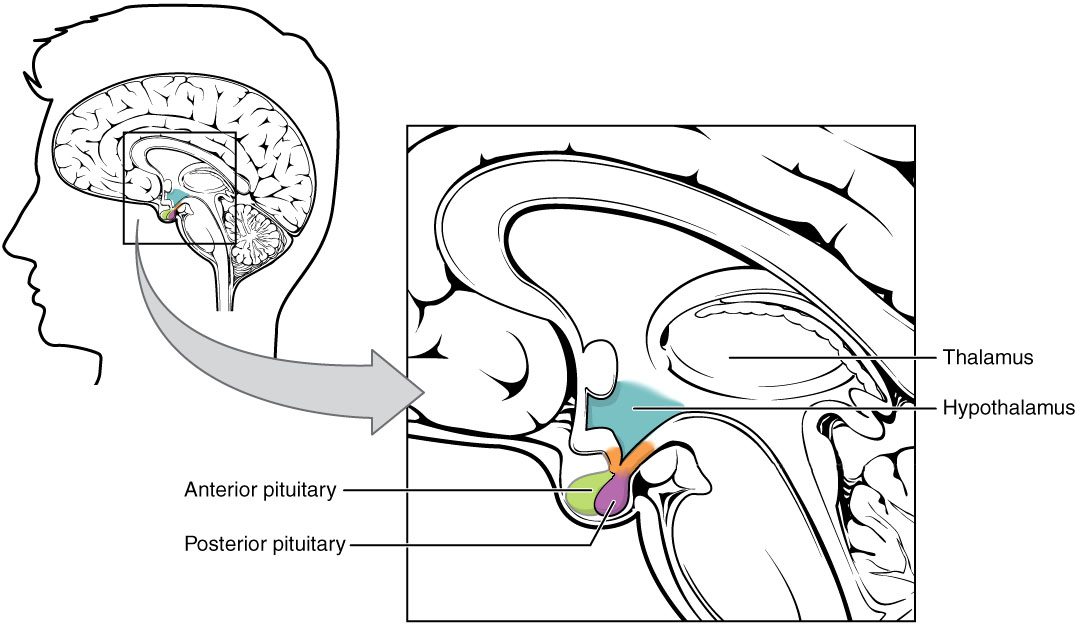
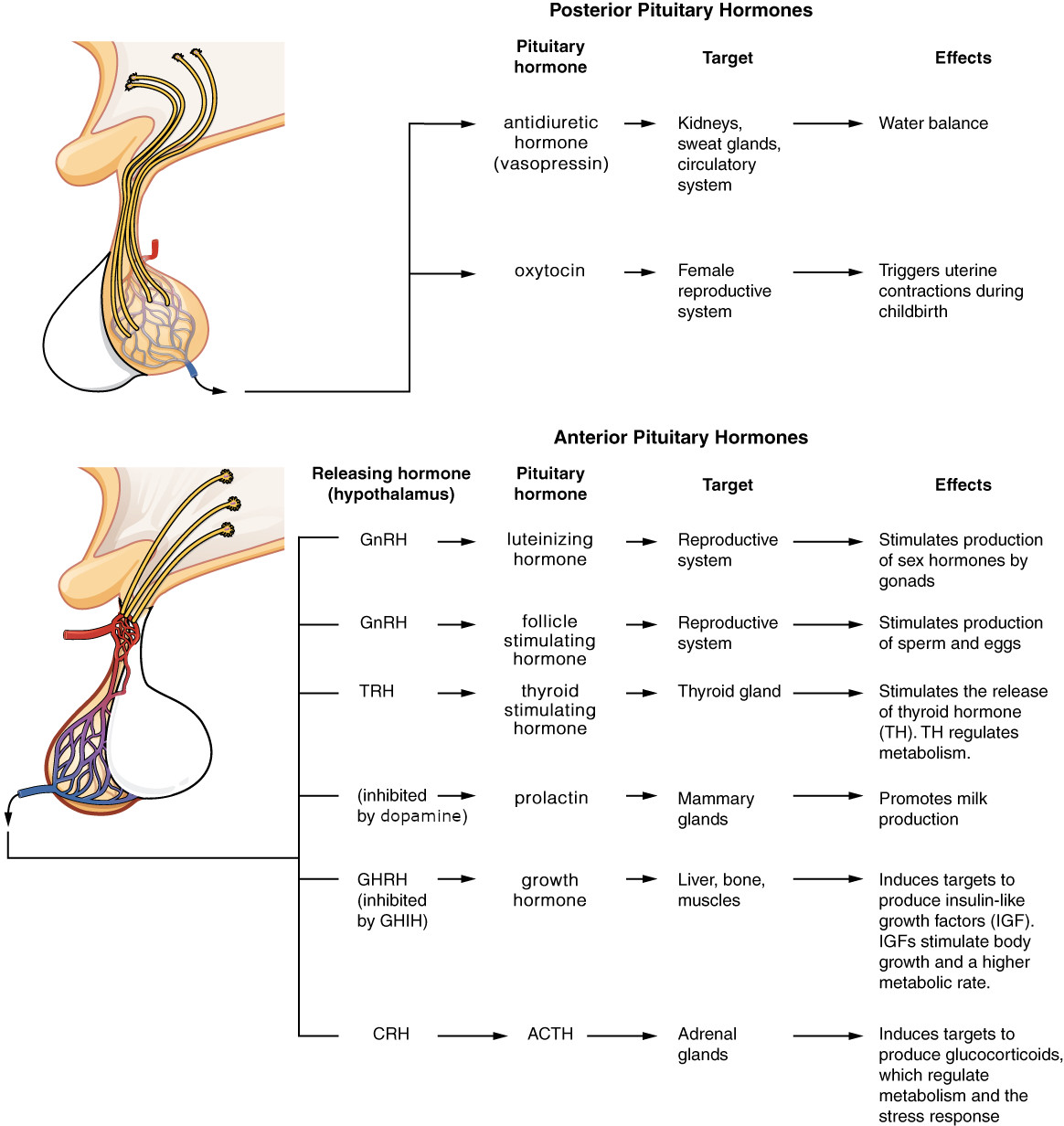
The endocrine-regulated variables are controlled by the hypothalamus through the pituitary gland as both organs are anatomically and functionally in direct association. The pituitary gland is a small gland located at the base of the brain composed of two lobes: anterior and posterior, with the intermediate lobe that joins the two regions.
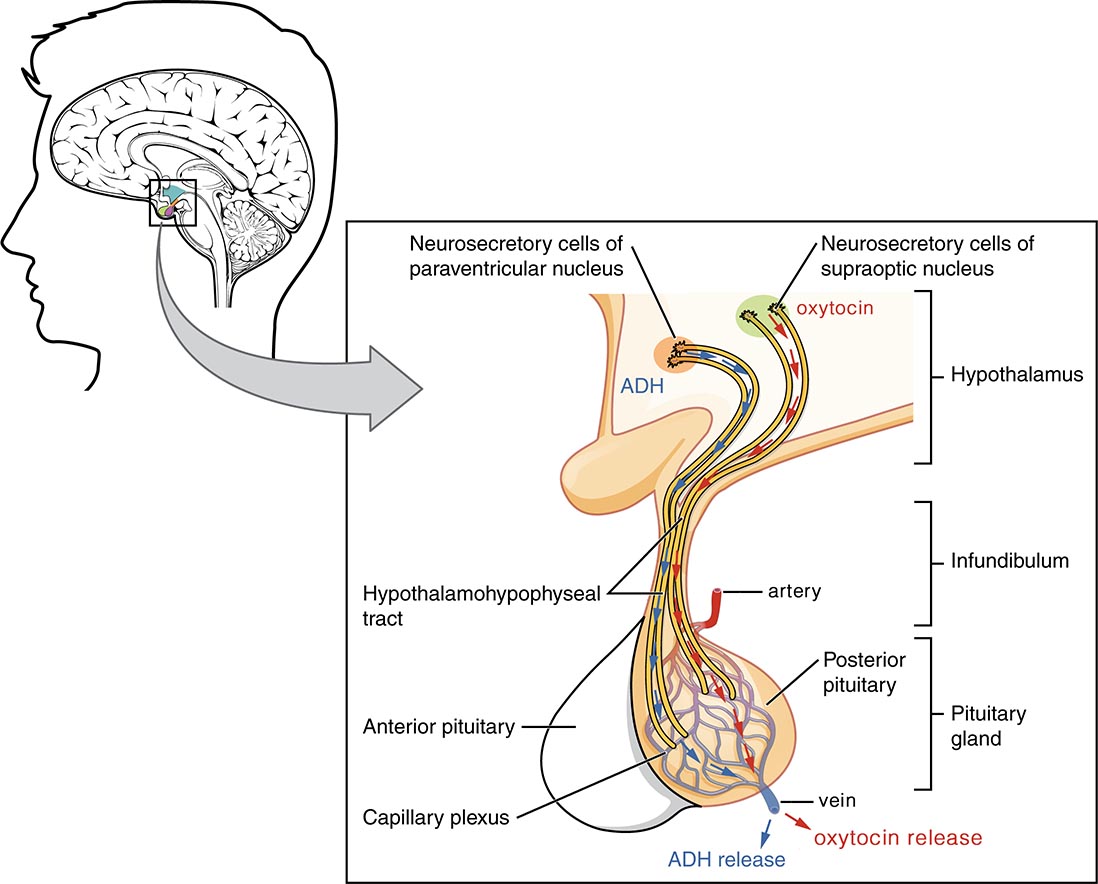
The posterior pituitary gland that derives from neural ectoderm is an extension of the hypothalamus into what is anatomically known as the posterior lobe, or neurohypophysis, which form the hypothalamic-neuro-hypophyseal system that secretes oxytocin and vasopressin directly into the blood stream. Oxytocin controls mammary gland functions and contraction of the uterus during birth, while vasopressin (also termed antidiuretic hormone or ADH) is involved in controlling blood pressure and water retention by the kidneys.
The anterior pituitary gland is composed of cells of epithelial origin derived from the oral ectoderm. They form the anterior pituitary lobe or adenohypophysis that secretes glycoproteins and proteins hormones that directly or indirectly control stress, metabolism and growth, reproduction, and lactation. The hypothalamus controls the anterior pituitary gland through axon terminals of hypothalamic neurons that secrete neurohormones into the vasculature of the median eminence located at the base of the brain and irrigate the anterior pituitary gland via the hypothalamus-hypophyseal portal vessel system. Hypothalamic neurons produce both stimulatory and inhibitory effects on the pituitary gland. Hypothalamic peptides with stimulatory effects are called releasing hormones, while peptides with inhibitory effects are called inhibitory hormones.
Under control of the hypothalamic neurohormones, the anterior pituitary gland produces six hormones:
- Glycoproteins:
- Follicle stimulating hormone (FSH),
- Luteinizing hormone (LH), and
- Thyroid stimulating hormone (TSH),
- Polypeptides:
- Adrenocorticotropic hormone (ACTH),
- Prolactin (PRL), and
- Growth hormone (GH).
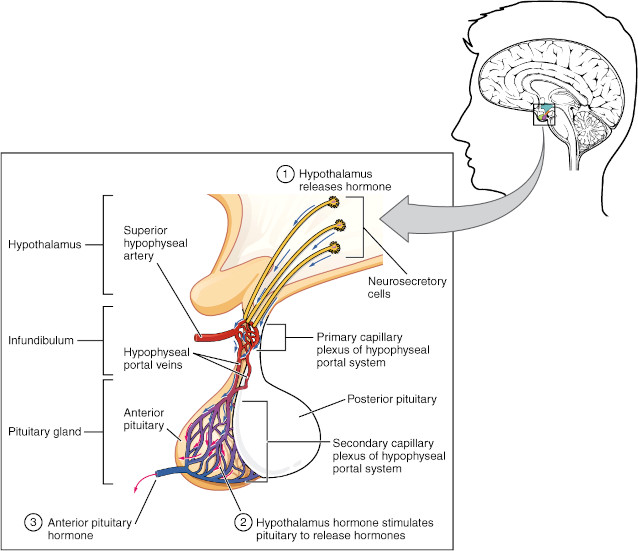
Secretions of the anterior pituitary gland are regulated by two homeostatic feedback loops. The first loop, termed the short loop, is between the hypothalamus and the anterior pituitary gland. The second loop, termed the long loop, is between the anterior pituitary gland and the target glands or tissues. According to the gland or tissue affected, they are grouped into regulatory axes between the hypothalamus, the anterior pituitary gland, and the glands and tissues being regulated:
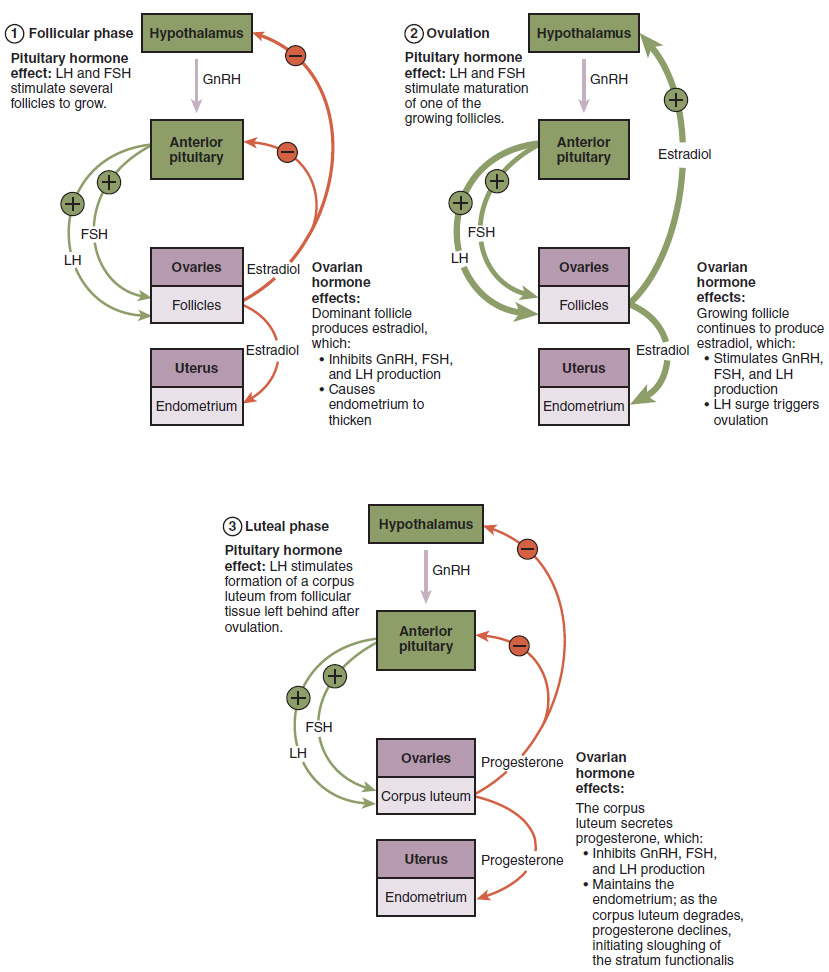
- The hypothalamic–pituitary–gonad axis is a direct control between the hypothalamus, the anterior pituitary gland and the ovaries or testis. The hypothalamus secretes gonadotropin-releasing hormone (GnRH) and the anterior pituitary gland respond with a secretion of the gonadotropic hormones, follicle-stimulating hormone (FSH) and luteinising hormone (LH), which control the gonads. The gonads respond with the secretion of steroid hormones; The ovaries respond with secretion of estradiol and progesterone, and the testes respond with secretion of testosterone. Both groups of steroids exert feedback control on the axis.
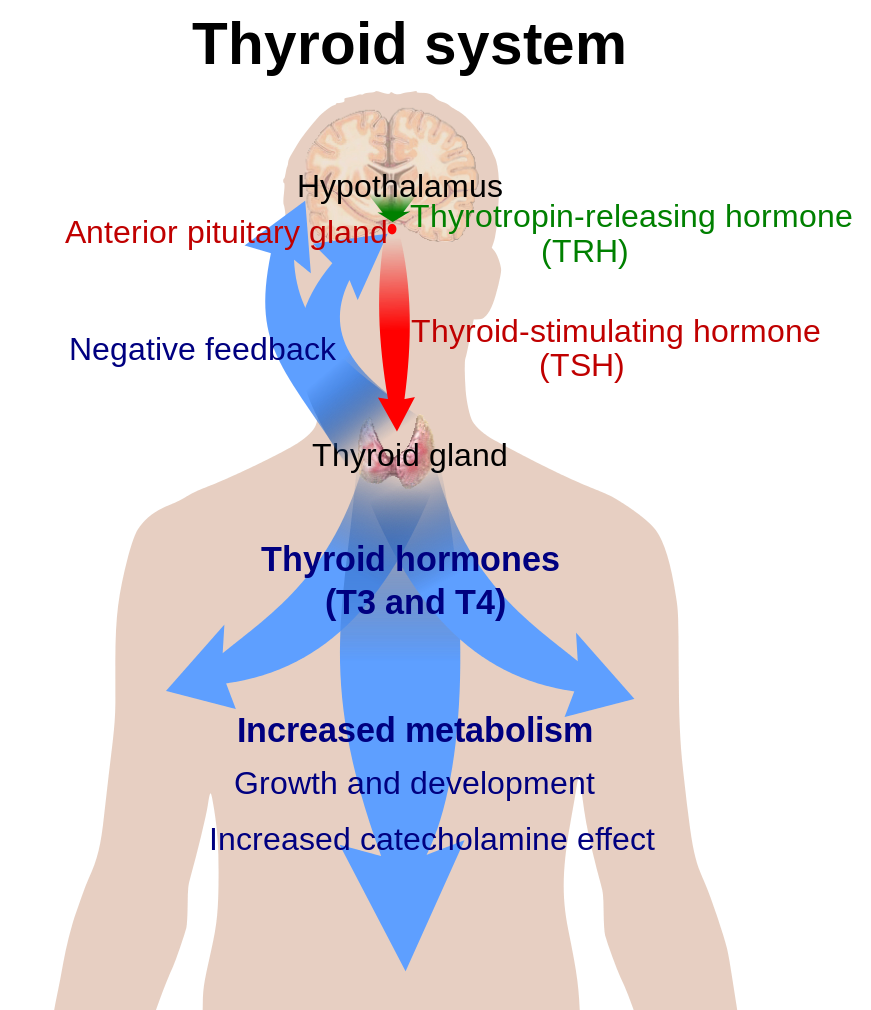
- The hypothalamic–pituitary–thyroid axis is a direct control between the hypothalamus, the pituitary gland and the thyroid gland that secretes triiodothyronine (T3) and thyroxine (T4). The hypothalamus senses low circulating levels of T3 and T4 and responds by releasing thyrotropin-releasing hormone (TRH) from the anterior pituitary gland, which in turn stimulates the thyroid to produce T3 and T4 until levels in the blood return to normal. The thyroid hormones exert negative feedback control over the hypothalamus as well as anterior pituitary gland, thus controlling the release of both TRH from hypothalamus and TSH from anterior pituitary gland.
- The hypothalamic–pituitary–adrenal axis is a direct control between the hypothalamus, the pituitary gland and the cortex of the adrenal glands. The hypothalamus secretes corticotropin-releasing hormone (CRH) into the short loops, the anterior pituitary gland secretes adrenocorticotrophic hormone (ACTH) and the adrenal glands cortex respond with secretion of glucocorticoids that negatively feedback the axis.
- The hypothalamic–pituitary–mammary gland axis is a direct control between the hypothalamus, the pituitary gland that secretes the hormone prolactin (PRL) that stimulates milk production by the mammary gland. The hypothalamus controls this axis by secretion of dopamine, a neurotransmitter that inhibits PRL secretion by the pituitary gland.
- The hypothalamic–pituitary–somatotropic axis controls growth hormone (GH) secretion from the pituitary gland. GH stimulates insulin-like growth factor 1 (IGF-1, also termed somatomedin-1) production in the liver. The hypothalamus controls secretion of GH through a dual mechanism that involves two peptides with opposite effects on the pituitary gland: the GH-releasing hormone (GHRH; also termed somatocrinin), and the GH-inhibiting hormone (GHIH, also termed somatostatin). Thus, GHRH and GHIH exert inhibitory and stimulatory short loops of feedback control over GH secretion by the pituitary gland. In addition, the peptide ghrelin termed the “hunger hormone” produced by the by cells of the gastrointestinal tract mainly the stomach, stimulates GH secretion by the anterior pituitary gland.
| Anterior Pituitary Hormone | Hypothalamic Hormone | Major Functions of Anterior Pituitary Hormone |
|---|---|---|
| Adrenocorticotropic hormone (ACTH) | Stimulatory: Corticotropin-releasing hormone (CRH) |
Stimulates glucocorticoids synthesis and release by the adrenal glands |
| Follicle-stimulating hormone (FSH) | Stimulatory: Gonadotropin-releasing hormone (GnRH) |
Stimulates germ cells development and sex steroid production by the gonads |
| Luteinizing hormone (LH) | Stimulatory: GnRH |
Stimulates sex steroid production by the gonads and induces ovarian ovulation |
| Growth hormone (GH) | Stimulatory: GH-releasing hormone (GHRH) |
Promotes linear growth; regulates glucose and fatty acid balance in the blood and protein metabolism |
| Inhibitory: GH inhibitory hormone (GHIH or somatostatin) |
||
| Prolactin (PRL) | Inhibitory: Dopamine |
Stimulates milk production in the mammary glands |
| Thyroid-stimulating hormone (TSH) | Stimulatory: Thyrotropin-releasing hormone (TRH) |
Stimulates the thyroid gland to produce thyroid hormones |
There are many examples of positive feedback loops in animal physiology. Two particularly famous examples are the blood clotting cascade, and the rising phase of an action potential. You’ll learn about these later in this book. For the moment, let’s look at two examples of positive feedback loops in mammalian reproduction:
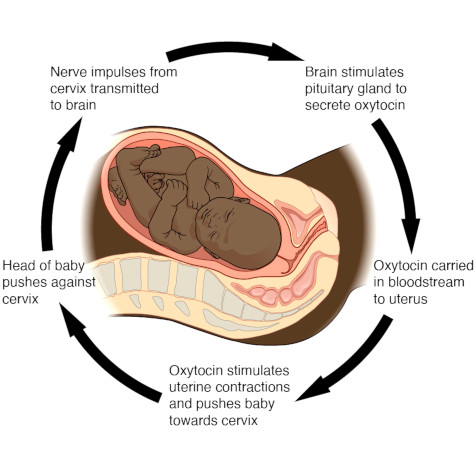
Childbirth and breastfeeding are classical examples of positive feedback loops. At the time of parturition pushing of the baby towards the cervix of the uterus stretch sensor that signal the hypothalamus to produce the neurohormone oxytocin, secreted by the posterior pituitary gland. Oxytocin targets the smooth muscular cells of the uterus and intensifies contractions of the organ that take place during childbirth. This is a positive feedback as the more the child pushes the more oxytocin is released and more intense are the contractions of the uterus. Thus, by positive feedback oxytocin accelerates the output created by the child stimulus on the cervix.
When are positive feedback loops useful? Three kinds of situations come to mind:
- amplifying a small signal into a much bigger signal,
- committing to one or the other choice out of two possible conditions, and
- memory (where the choice is between two stable states, for example a typical light switch).
You can see that the first two of these apply to the positve feedback loop in childbirth.
In lactating mothers, oxytocin acts on the mammary glands, causing milk to be ‘let down’ into lactiferous ducts, from where it can be secreted via the nipple. Suckling by the infant at the nipple causes more oxytocin to be released, which in turn causes more milk letting down into the lactiferous duct. In addition, breastfeeding exerts a positive feedback loop on secretion of the hormone prolactin, which is the hormone of the anterior pituitary gland that stimulates production of milk. As the baby suckles, the mother’s pituitary gland secretes more prolactin, which causes more milk to be produced.
13.4 Body Temperature Regulation
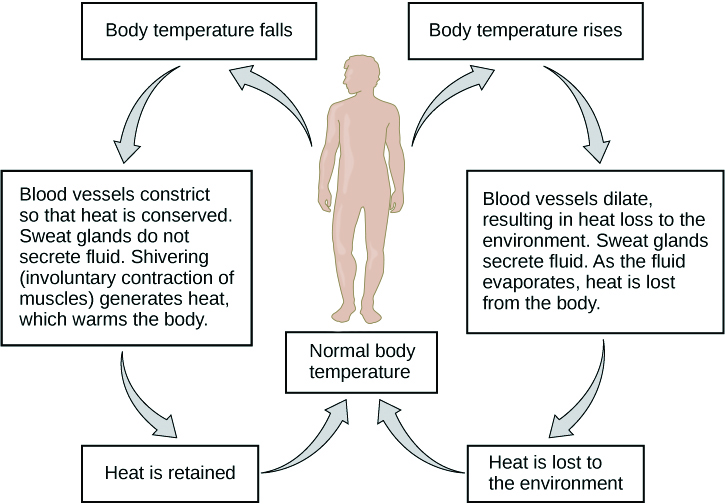
Control of body temperature is a classical example of negative feedback loop. The centre controlling body temperature is located in the hypothalamus, which monitors the temperature and sends signals to the effectors to compensate for deviations between detected value and the temperature set point. The components of the mechanisms of temperature regulation in the body can be compared with the components of the temperature regulatory system in a house, in which there are at least four interdependent components for a regulated variable:
- The set point is the normal value for controlled variable. For example, the human core body temperature is normally close to 37°C.
- The receptor is the sensing component that monitors and responds to changes in the environment, either external or internal. In the case of body temperature, thermoreceptors are the sensing component.
- The integrator processes information from the sensing component to generate an appropriate response. In the control of body temperature in humans, the hypothalamus compares signals detected by the thermoreceptors to the set point and compensates for any changes.
- An effector is the target acted on to bring about a change back towards the set point. It compensates for deviations between sensed value and the set point value. Effectors for body temperature include muscle, endocrine and exocrine glands, and other regulated structures that can generate, conserve or dissipate heat.
When body temperature falls, muscles are one of the effectors among many that can elevate body temperature. Shivering of the skeletal muscle elevates body temperature, which sends a negative feedback signal to the hypothalamus that relieves shivering. Vasoconstriction and formation of goosebumps are also part of the body rapid response to low temperature. In humans, peripheral blood vessels tighten the surrounding skin reducing the surface area from which to lose heat. Vasoconstriction ensures that only a small surface area of the veins is exposed to the cooler outside temperature, retaining heat. In other mammals, goosebumps raise the hair or fur allowing more heat to be retained.
When body temperature rises above normal the body begins to sweat, and vasodilation occurs to allow more of the blood surface area to be exposed to the cooler external environment. As the sweat cools, it causes evaporative cooling, while the blood vessels cause convective cooling.

13.5 Control of Blood Glucose
The concept of homeostasis was originally defined by the French scientist Claude Bernard as a milieu intérieur (French: internal environment) in 1865. “Milieu intérieur” refers to the composition of the extracellular fluid environment and its physiological capacity to ensure protective stability for the tissues and organs. This concept was later reviewed and expanded by Walter Cannon in 1926, who studied regulation of blood glucose content. Glucose supply is required for most tissues in the body, but is particularly essential to the brain, testes, erythrocytes, and kidney medulla as it is the only source of energy that they can use. Therefore, a tight regulation of glucose metabolism is critical and certain level of glucose in the blood must be maintained in order to assure sufficient energy for the normal functioning of those critical tissues. The graph (Figure 9) is a representation of the results of one of the experiments conducted by Walter Cannon to study regulation of glucose in blood, as an example of homeostatic control.

After a meal, the small intestine absorbs glucose from digested food, therefore blood glucose levels rise very rapidly as can be appreciated in the graph, but one hour after glucose start to decrease in response to a compensatory mechanism that reduces its concentration to normal levels. We now know that the endocrine compensatory chemical signal responsible for the reduction in blood glucose after a meal is the hormone insulin, which is a peptide secreted by the beta cells of the pancreatic islets that sense glucose.
Glycogenesis is the process by which the soluble glucose monomers are added to the insoluble polymer glycogen for cell storage of energy.
Glycogenolysis is the breakdown of the polymer glycogen into the soluble monomer glucose.
Glycogenolysis takes place mainly in muscle and liver cells when more energy is needed.
Gluconeogenesis is the metabolic process by which non-carbohydrate precursors are converted into sugars, mainly glucose.
High glucose levels signal the beta cells to secrete insulin, which stimulates transport of glucose into cells for their own use, and therefore reduces its blood levels. A decrease in glucose is the negative feedback signal to stop insulin secretion. If glucose is not immediately used, it is converted into glycogen by glycogenesis for energy storage, mainly in the liver and muscle tissue as a reserve of energy.
The second salient point that we can observe in this graph is that after 24 h fasting, during which circulating glucose was consumed, its blood levels are slightly reduced; meaning that glucose levels are restored regardless of the dietary supply. In this case, low glucose signals the hormone glucagon, which also secreted by the pancreas, but by the alpha cells of the islet, to stimulate glycogenolysis from liver reserves of glycogen, to liberates glucose into the blood stream. Thus, both hormones exert negative feedback control: Insulin prevents hyperglycemia, while glucagon prevents hypoglycemia.
The graph also illustrates how blood glucose rises in the absence of the compensatory effect of insulin. This condition is observed in diabetes, a disease of the endocrine system in which insulin is deficient or cells become resistant to it. Insulin is essential for normal functioning of the body as glucose is a nutrient of high biological value that the body retain by reabsorbing it in the kidneys. If excess of blood glucose in the blood stream overcomes the kidneys capacity to reabsorb it, glucose is lost in the urine causing dehydration as it behaves as an osmolyte that continuously attracts water that is lost in the urine.

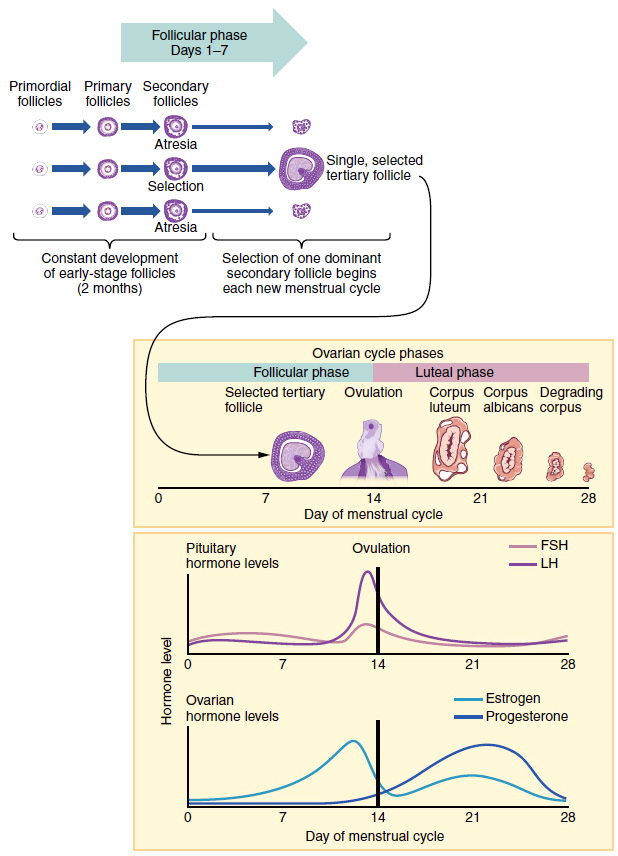
13.6 The Ovarian Cycle
Homeostasis during the ovarian cycle is an example of positive and negative feedback loops on the same regulated variable. Ovarian function is regulated by the hormones FSH and LH produced by the anterior pituitary gland under control of the hypothalamus. During the first half of the ovarian cycle, gonadotropins stimulate production of the steroid hormone estradiol that promotes follicular growth. During this part of the ovarian cycle, estradiol exerts negative feedback control on the hypothalamus to prevent secretion of excessive amounts of gonadotropins until the follicle matures and becomes ready to ovulate. But when the ovarian follicles mature and are ready to ovulate, estradiol reverses its effect from negative feedback to positive feedback, demanding more gonadotropins to be liberated to trigger ovulation. The positive feedback effect of estradiol on the hypothalamus increases secretion of GnRH causing a sudden surge of the hormone LH by the anterior pituitary gland that stimulates the release of the oocyte through the rupture of the follicle.
13.7 Homeostasis at the Cellular Level
As mentioned before, homeostasis happens at the level of the whole body, at the level of individual organs, at the level of tissues, and at the level of individual cells. At the level of an individual cell, there is a huge number of variables that need to be kept relatively stable if the cell is to function at full efficiency. Most of those variables are beyond the scope of this course – a good, thorough biochemistry course would cover those – but we will discuss homeostasis of signalling molecules because they are particularly relevant to animal physiology.
For example, quite often, excitable cells such as neurons don’t respond in proportion to the absolute strength of a stimulus, but instead respond more to a change in the strength of the stimulus. How do they accomplish this? In many synapses, there is negative feedback control of the amount of neurotransmitter released from the pre-synaptic cell, and also negative feedback control of the number of neurotransmitter receptors at the surface of the post-synaptic cell.
13.8 Summary
- Homeostasis is property of the body that assures constancy of the internal media variables required for normal functioning of all tissues and organs.
- Variables under homeostatic control include body temperature, pH of the extracellular fluid, carbon dioxide and oxygen, osmotic pressure and concentrations of ions such as sodium, potassium and calcium, blood pressure and blood sugar level, among others, which are constantly kept within certain pre-set limits termed homeostatic range.
- The primary components of a homeostatic controlled system include a stimulus, a receptor, a center of control, an effector, and feedback mechanisms.
- Two main types feedback loops control homeostasis: positive feedback loops and negative feedback loops.
- In the positive feedback loops, a change in intensity of a stimulus causes further changes on the same stimulus.
- In the negative feedback loops, a change in intensity of a stimulus causes inhibition of the same stimulus.
- The organs that maintain homeostasis include the nervous system, which working in tandem with the endocrine system form what is called the neuroendocrine system that includes the posterior and anterior pituitary glands.
- Childbirth and breastfeeding are the classical examples of positive feedback loop.
- Control of body temperature and control of blood glucose levels are examples of negative feedback loop.
- Homeostasis during the ovarian cycle is an example of positive and negative feedback loops on the same regulated variable.

