Case Studies
Case 1: Sonata
Sonata, a 12-year-old F(s) Dachshund dog, had lethargy, anorexia, and vomiting. The main physical finding was cachexia.

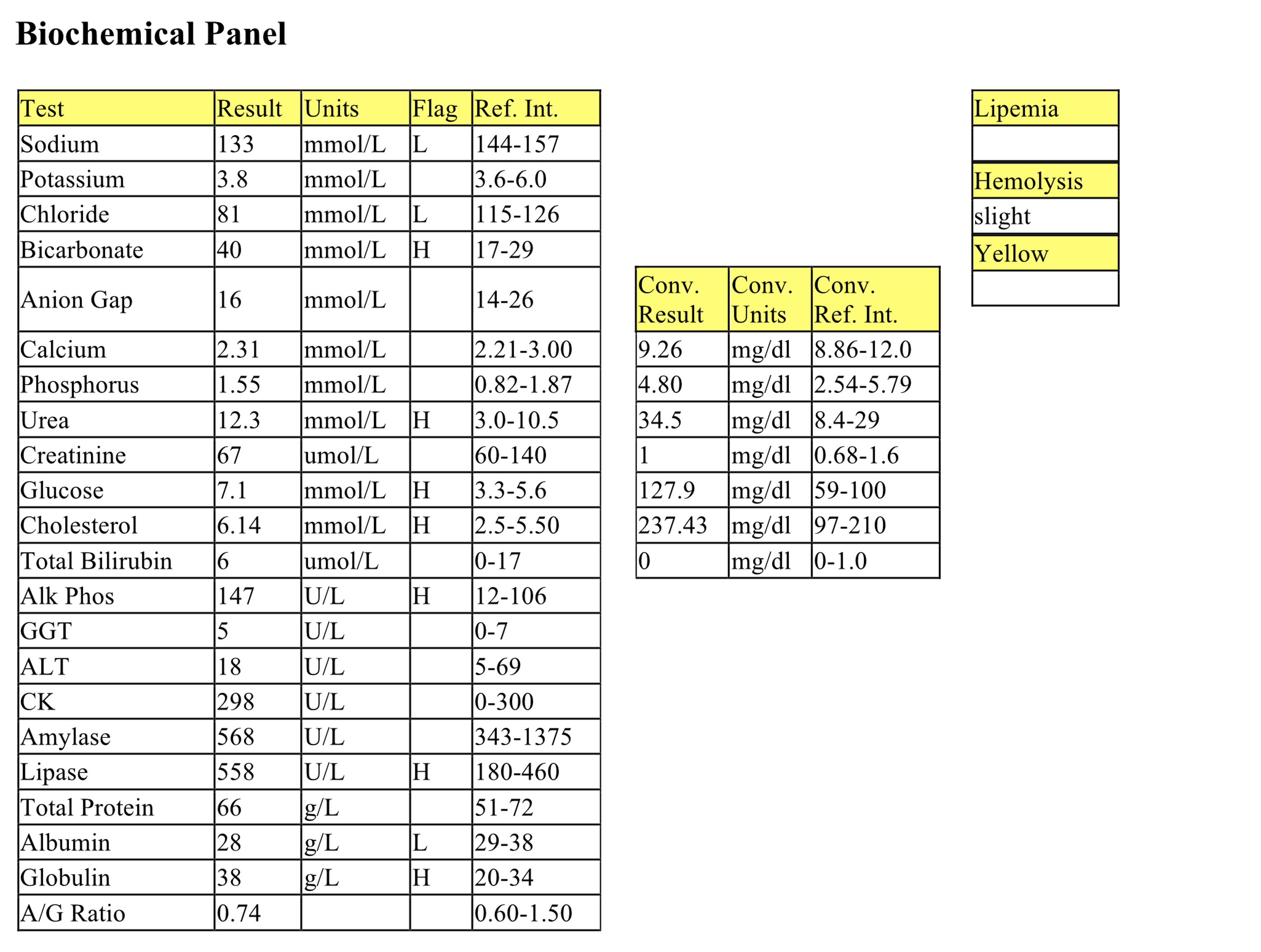
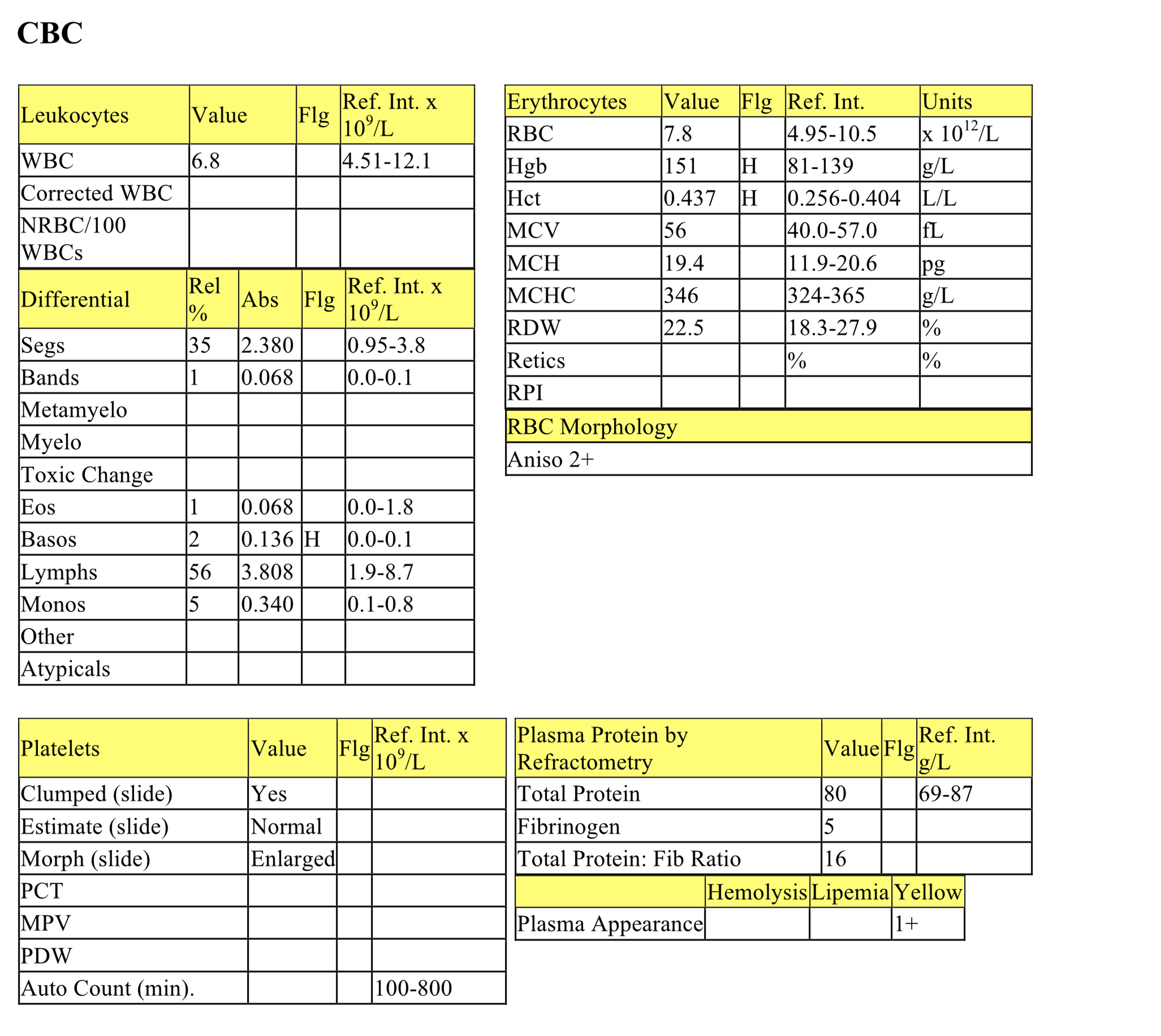
CBC
The erythrogram is unremarkable. The increased RDW does not correspond to increased anisocytosis, so its importance is questionable. Rouleaux of 1+ is unlikely to be significant since up to 1+ can be seen in normal dogs, and there is no evidence of hyperproteinemia. There is a mild leukocytosis characterized by mild neutrophilia with a moderate left shift, mild toxic change, and mild to moderate monocytosis. These findings indicate significant inflammation to which the bone marrow is appropriately responding at this time. They are consistent with established ongoing inflammation, but monitoring for trends is needed to further establish a time frame.
Biochemical Panel
Mild hyponatremia and moderate hypochloremia are probably due to increased losses from vomiting coupled with continued drinking as well as lack of intake. In addition, chloride is disproportionately low relative to sodium, suggesting selective loss. This hypochloremia coupled with metabolic alkalosis (increased bicarbonate) is consistent with loss of HCl from the upper intestinal tract as can be seen with foreign bodies, neoplastic disease, and local inflammatory disease. Mildly increased urea should be interpreted in relation to USG (not available for this case), in order to determine if prerenal or renal azotemia is present. Creatinine may not be also increased because of muscle wasting in this patient. Alternatively, intestinal hemorrhage (rich protein source) could explain a selective increase in urea, unrelated to renal function. Mild hyperglycemia is likely due to stress. Mild changes in cholesterol and lipase are not considered significant. Increased ALP activity could be from mild cholestasis or steroid induction. Mild hypoalbuminemia may relate to its role as a negative acute phase protein. Mild increase of globulins may be due to inflammation (positive acute phase proteins) and/or antigenic stimulation.
The inflammatory leukogram, and electrolyte and acid-base abnormalities suggest an upper intestinal tract lesion. Given the age of the dog and reported cachexia, neoplasia was very possible. Inflammation could occur with necrosis of a tumor mass or with devitalization or ulceration of local intestinal tissue. Long-standing foreign body, also leading to a local inflammatory process, was also considered.
- Sonata underwent surgery and a 10 cm section of distal duodenum and proximal jejunum was removed. Plastic, rubber, and other foreign material were contained within this region of bowel. Histologically, there was severe, chronic, pyogranulomatous enteritis. There was a locally extensive area of mucosal necrosis and a mixed inflammatory cell infiltrate extending from the mucosa through to the serosal surface. Sonata recovered uneventfully.
Case 2. Theodore
Theodore, a 12-year-old M(c) Pomeranian X dog, was presented for anorexia, depression, and vomiting for 3 days. The dog was polyuric and polydipsic, and he was dehydrated on physical examination.
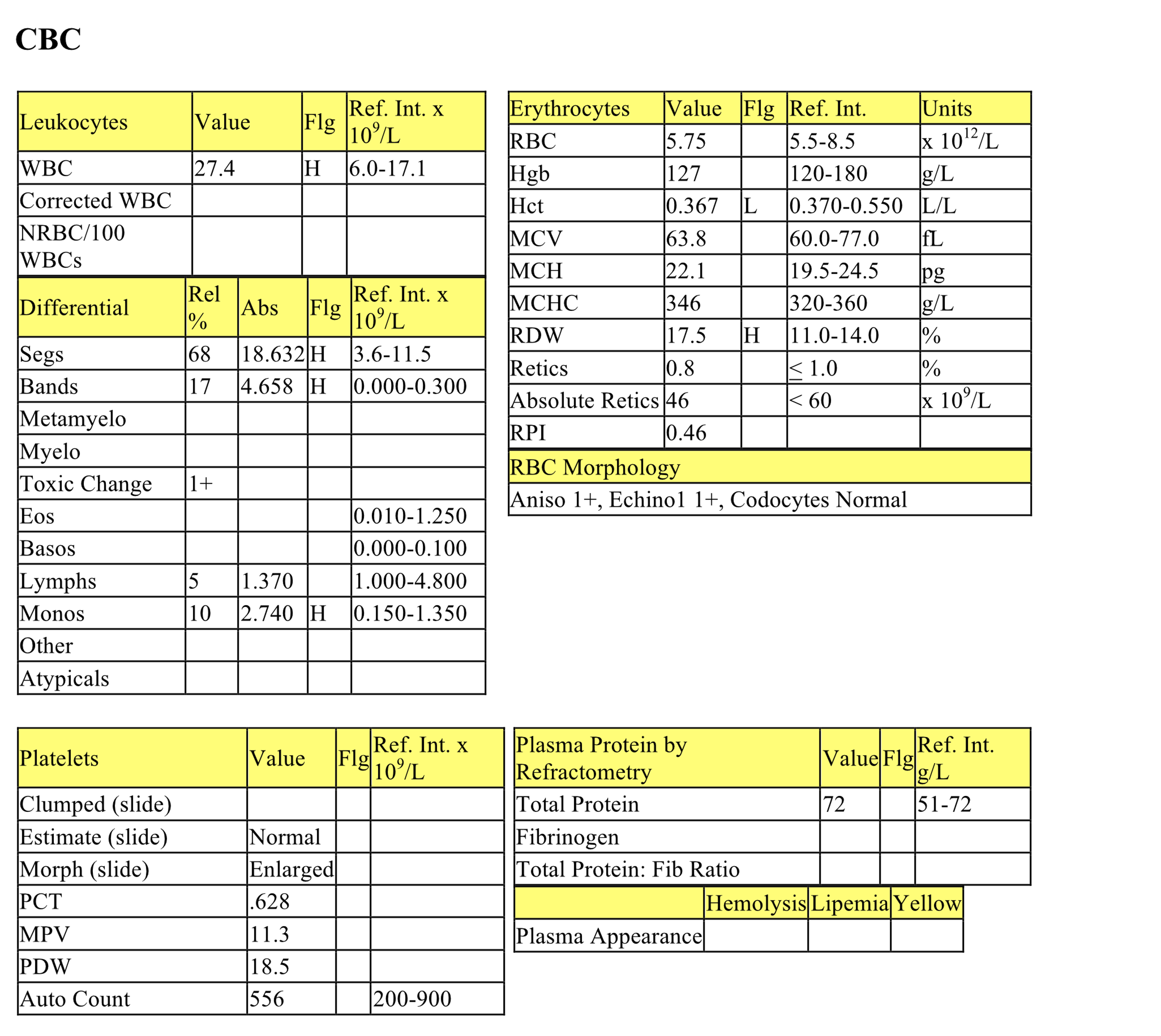
CBC
The mild nonregenerative anemia may be underestimated if Theodore is dehydrated (as stated in history). The leukocytosis is characterized by a mild to moderate neutrophilia with a moderate left shift, mild toxic change, and mild-moderate monocytosis. These findings indicate significant inflammation to which the bone marrow is appropriately responding at this time.
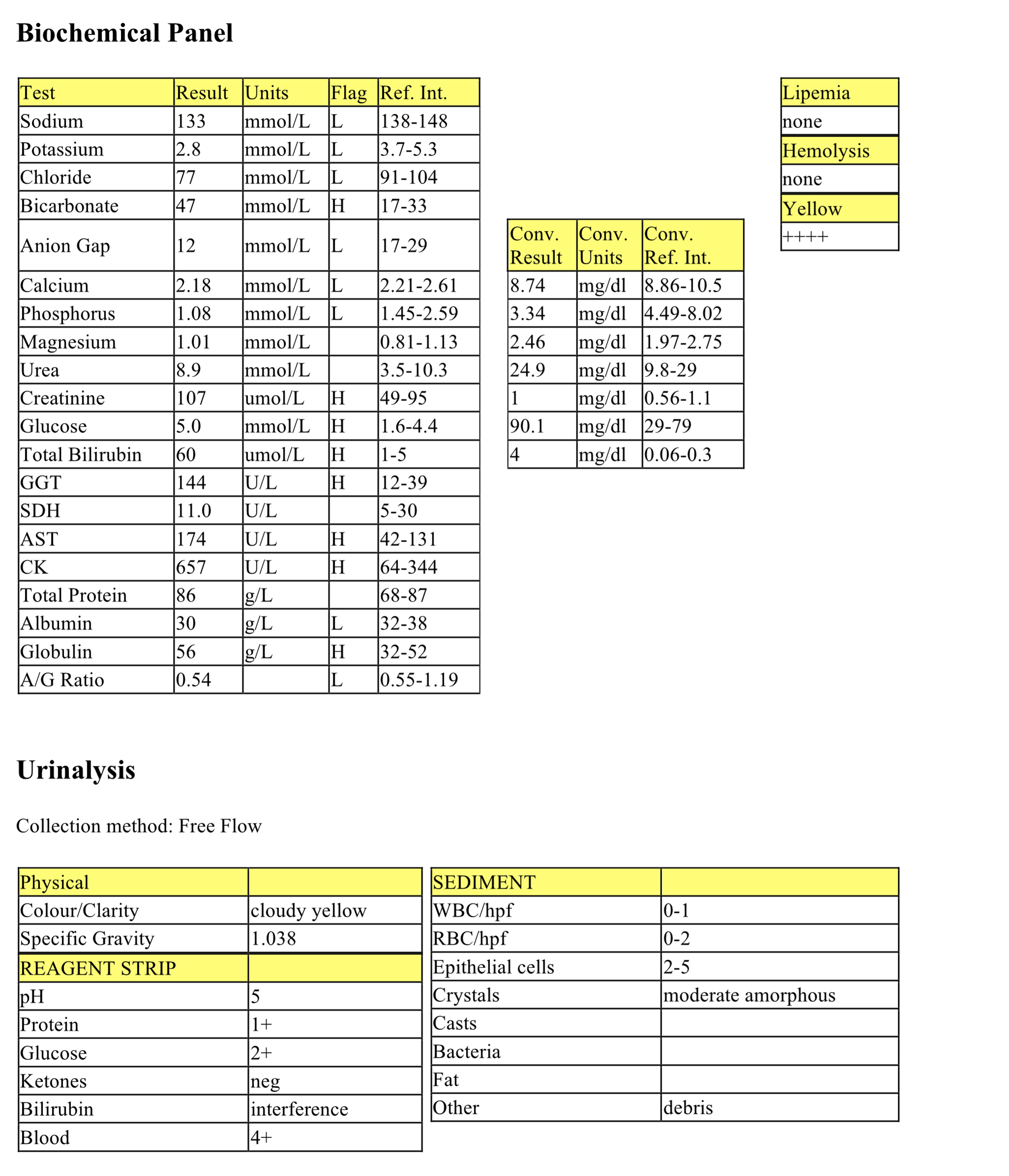
Biochemical Panel
Marked hyponatremia and hypochloremia are due to several reasons: increased losses from vomiting and osmotic diuresis (glucosuria associated with diabetes mellitus leads to renal sodium and chloride loss), hyperglycemia draws water out of cells leading to a relative decrease in sodium and chloride in the peripheral blood, and lack of intake. Chloride is low relative to sodium, probably from vomiting and HCl loss. The high anion gap metabolic acidosis relates to retention of renal acids as well as probable ketoacidosis. Lactic acidosis may also be present if there is poor perfusion due to dehydration. Mild hypocalcemia can be seen with acute pancreatitis. The mechanism is not confirmed but may relate to binding of calcium to free fatty acids which are liberated from fat necrosis within the peritoneal cavity. The urine is not sufficiently concentrated given the presence of azotemia (urea and creatinine elevations), indicating renal azotemia. Marked hyperglycemia is consistent with diabetes mellitus which can be transient when acute pancreatitis occurs, or can be pre-existing. Recurrent pancreatitis may also cause diabetes mellitus by repeated destruction of endocrine along with exocrine pancreatic tissue. Given the likelihood of ketoacidosis, pre-existing diabetes mellitus is probable. The moderately increased ALP activity suggests cholestasis, related to pancreatitis or hepatic lipidosis (from diabetes mellitus), enzyme induction from increased levels of endogenous/exogenous steroids, or both. Amylase and lipase activities are mildly elevated which could be due to early pancreatitis, or secondary to decreased renal excretion or inactivation of these enzymes, or both. The history of vomiting, together with an inflammatory leukogram and increased activities of pancreatic enzymes, support the diagnosis of pancreatitis. Although we might expect hypoalbuminemia in this case since it is a negative acute phase protein, the albumin concentration is only low normal and hypoalbuminemia may be masked by the presence of dehydration (indicated in the history).
Urinalysis
The urine is not concentrated in the presence of azotemia, indicating renal disease. Glucosuria is consistent with diabetes mellitus. Ketonuria indicates that Theodore is in negative energy balance, utilizing fat stores rather than carbohydrates. Also, given the high anion gap metabolic acidosis, ketoacidosis is likely. Granular casts are seen with renal tubular injury.
- Theodore has multiple problems. He has mild anemia possibly from anemia of inflammatory disease or renal disease; inflammation which could be pancreatic in origin; diabetic ketoacidosis, and renal insufficiency. Theodore was started on fluids, antibiotics, and insulin; his response to treatment is not known.
Case 3. Brie
Brie, an 8-year-old F German Shepherd dog, had a history of increased water consumption and weight loss since whelping 8 months previously, and vomiting and anorexia over the day prior to presentation. The dog was emaciated and moderately dehydrated.
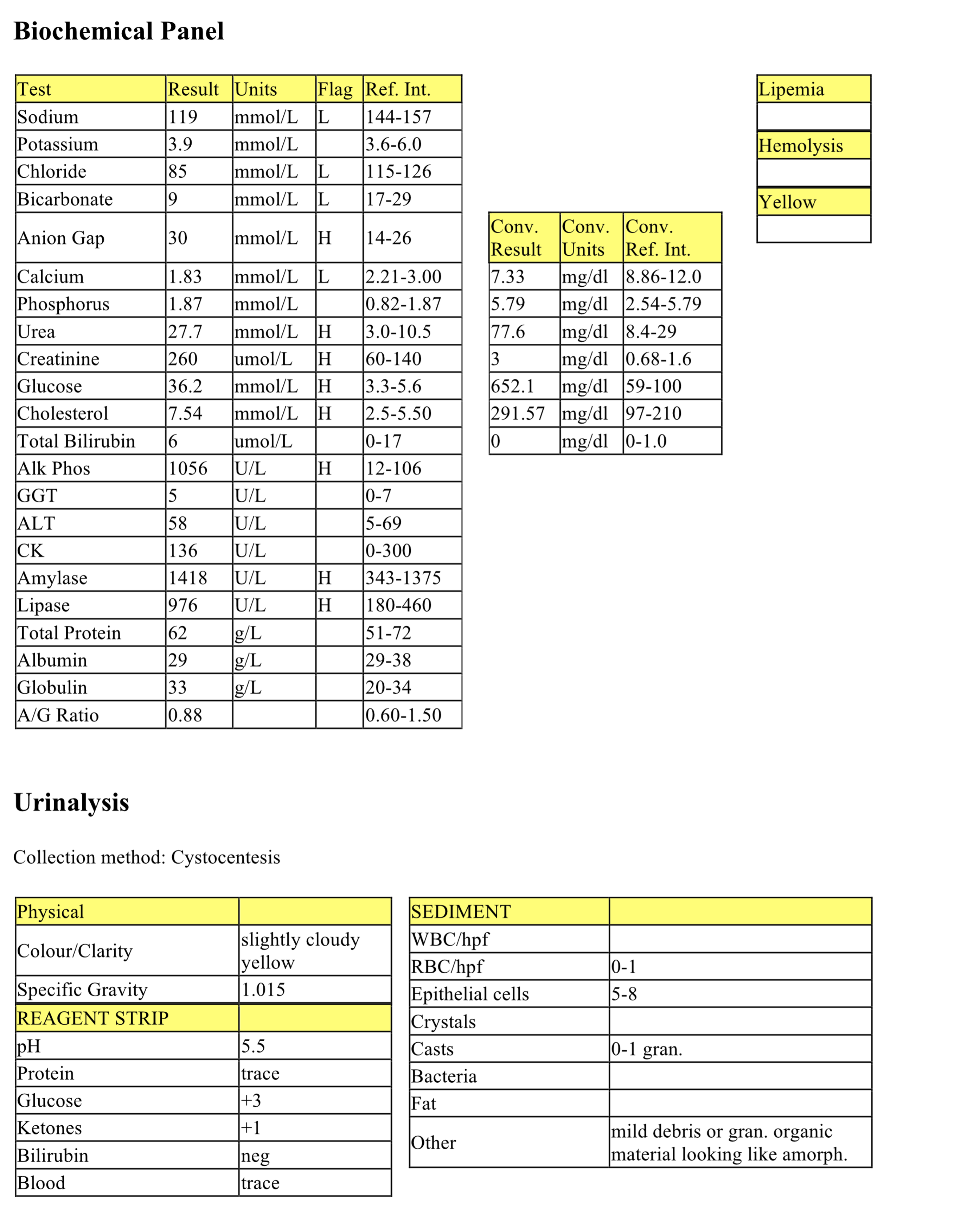
Biochemical Panel
There are abnormalities on the biochemical panel which are incompatible with life. The most notable of these are severe hyperkalemia and severe hypocalcemia. The clinic was contacted to discuss the results and it was determined that the sample had been collected into a purple topped tube containing dipotassium EDTA. The sample was then centrifuged and the plasma was withdrawn and placed in a red topped serum tube. Potassium in the anticoagulant resulted in the very high potassium measurement, and calcium was chelated by the EDTA resulting in the very low calcium measurement. The slightly low glucose was likely due to in vitro glycolysis of the sample prior to separation of cells from the plasma. The clinic was asked to resubmit an appropriate sample in order to obtain meaningful results.
Case 4. Nina
Nina, a 9-year-old Holstein-Friesian cow, had surgery for a displaced abomasum 2 days previously. She then became anorexic and depressed, but afebrile.
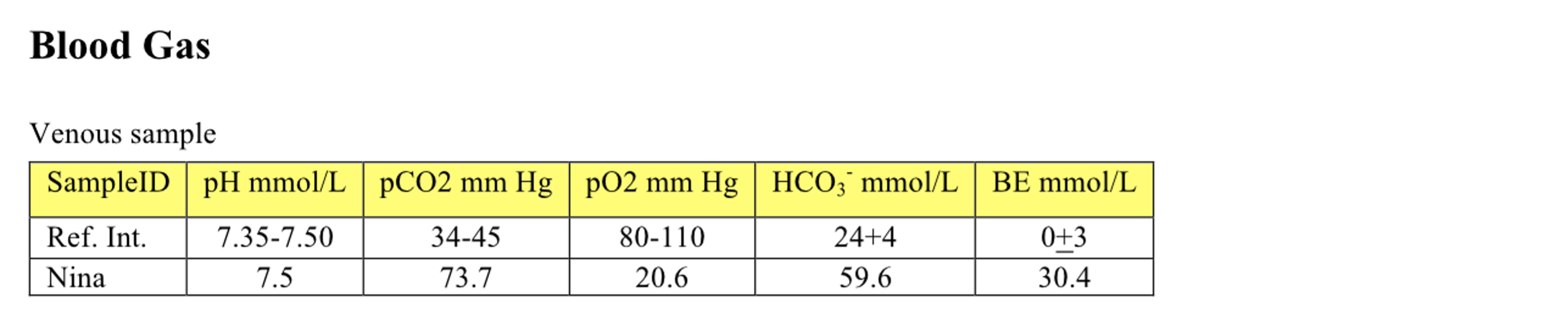
CBC
The mildly increased hematocrit and hemoglobin may be due to dehydration (relative erythrocytosis). The remainder of the CBC is unremarkable.
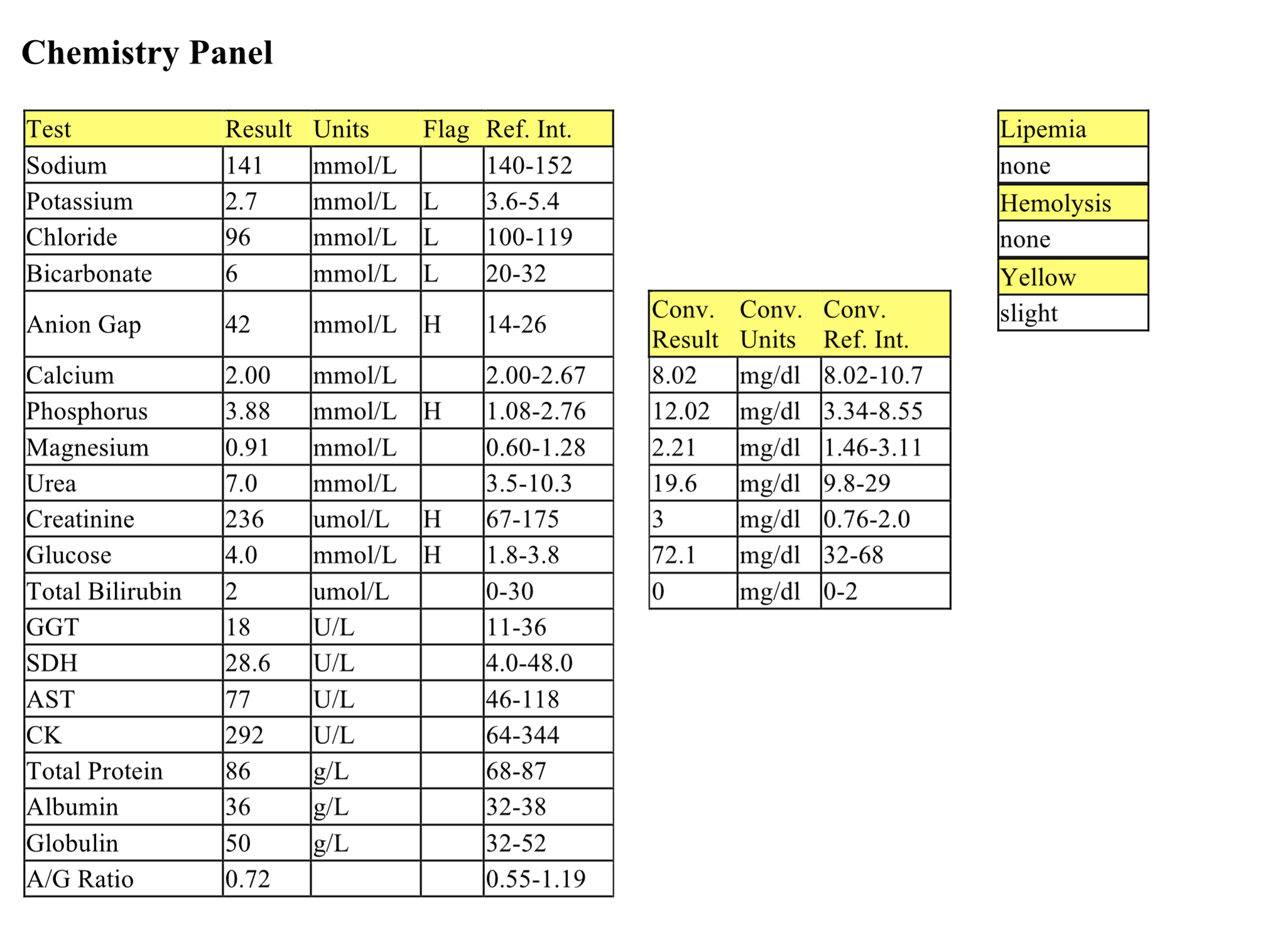
Biochemical Panel
Mild hyponatremia and hypokalemia may be due to decreased intake. Marked hypochloremia is disproportionate to the magnitude of hyponatremia suggesting HCl pooling in the abomasum. The severe metabolic alkalosis (increased bicarbonate) is also consistent with an abomasal disorder. Mildly decreased anion gap relates to the mild hypoalbuminemia. Very mild hypocalcemia and hypophosphatemia probably also relate to decreased feed intake, although there may be a contribution to the hypocalcemia from hypoalbuminemia (decreased protein binding to calcium). Creatinine is slightly increased which could be due to prerenal azotemia from dehydration. Hyperglycemia is related to stress and is mild. Moderate hyperbilirubinemia may be due to any combination of the following: cholestasis, lack of uptake of bilirubin by hepatocytes, decreased conjugation of bilirubin, decreased excretion of conjugated bilirubin, and anorexia. Moderately increased activity of GGT supports cholestasis as a cause of the hyperbilirubinemia. CK and AST activities are mildly increased suggesting muscle injury perhaps from increased recumbency. Hepatocellular injury is less likely to be a cause of increased AST activity given the normal SDH activity. Mild hypoalbuminemia may be due to decreased hepatic synthesis, renal loss, or decreased protein intake. Mild hyperglobulinemia is likely due to chronic antigenic stimulation, although dehydration may be a contributing factor.
Urinalysis
The urine is concentrated, supporting the evidence of prerenal azotemia. Aciduria is paradoxical given the metabolic alkalosis. Glucosuria is likely secondary to stress and mild hyperglycemia. 4+ blood on the reagent strip may be due to mild hematuria (only 0-2 intact erythrocytes/hpf though), lysed erythrocytes within the urine in vitro (hemoglobin) or myoglobin. 1+ protein may be due to contamination from the urogenital tract since this is a free flow sample, however hemoglobin or myoglobin may also contribute. The cause of interference with the bilirubin result is unknown in this case, but possibly because the result could not be verified with an additional test (ictotest).
Blood Gases
The pH >7.0 indicates alkalemia. The pCO2 is high because Nina is hypoventilating to try to compensate for the metabolic alkalosis by retaining acid. The very high bicarbonate and base excess also indicate that metabolic alkalosis is present. Low pO2, relative to that of arterial blood, is usually present in a venous sample, however this value is even lower than expected; collection of an arterial blood sample would be required to accurately evaluate oxygenation status in this cow.
- Although abomasal stasis is often secondary to anorexia for other reasons in cattle, there was historical and clinical evidence to suggest that Nina had a primary abomasal disorder. She was diagnosed with a mass at the level of the pylorus that was preventing outflow from the abomasum. Paradoxic aciduria occurs with long-standing alkalosis in the presence of dehydration, hyponatremia, hypokalemia, and hypochloremia (see text).
Case 5: Ramona
Ramona, an adult Texas Longhorn cow, had acute recumbency 2-3 days after grain ration was increased. The cow was very depressed and had a full, static rumen.
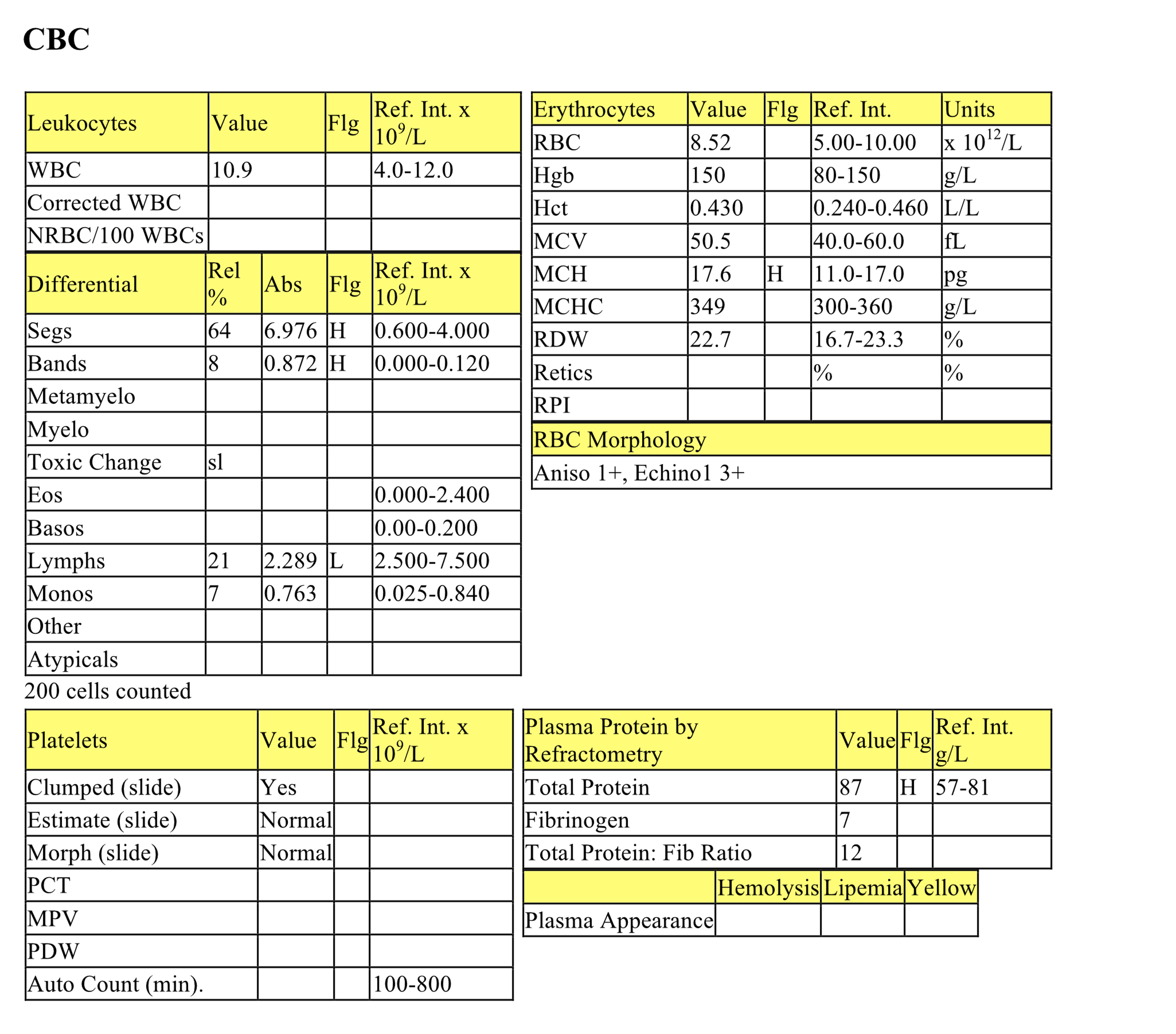
CBC
The hematocrit is high normal which could be normal for this cow or due to dehydration, as the serum protein is also high normal. The mild increase of MCH is not clinically significant. There is a mild neutrophilia with a mild left shift, slight toxic change, and mild lymphopenia. These changes indicate inflammation and stress. The fibrinogen concentration is high normal. The total protein to fibrinogen ratio is in the “grey” zone that could indicate dehydration, absolute hyperfibrinogenemia, or both.
See also Chapter 1: Erythrocytes, Case 1
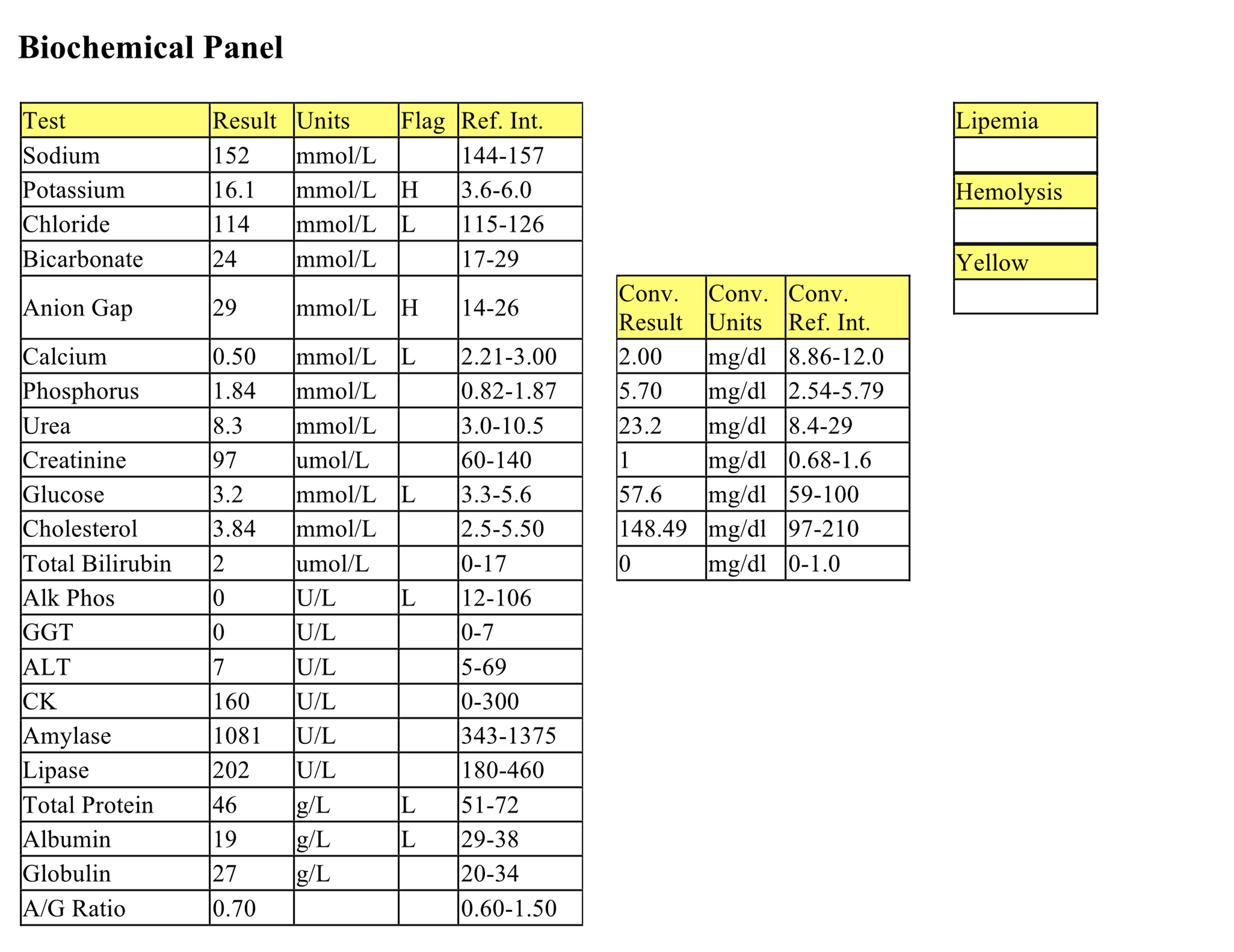
Biochemical Panel
Moderate hypokalemia may be due to decreased intake, loss/pooling within the digestive tract, and loss through the saliva. Mild hypochloremia may be due to pooling of HCl in the abomasum. The severe high gap metabolic acidosis is likely due to lactic acid accumulation from carbohydrate fermentation within the rumen, with possible contributions from renal acids. Low normal calcium relates to decreased intake. Mild to moderate hyperphosphatemia could be due to both decreased renal excretion and increased intake from excessive grain ingestion (a rich source of phosphorus). Creatinine elevation suggests prerenal azotemia given the additional evidence of dehydration; however, urinalysis is required to assess urine concentrating ability. Mild hyperglycemia is likely due to stress.
Ramona was suffering from grain overload (ruminal acidosis). Chemical rumenitis frequently becomes septic from infection of the damaged mucosa with bacteria, fungi, or both. Ramona was extremely ill and began passing watery feces with frank blood and sheets of mucosa. The rumen contents had a pH of 5, where ruminal pH is normally between 5.7 and 7.3. The prognosis is very poor in such situations. No further follow up is available.
State of extreme wasting, secondary to severe chronic illness.
All tests on the complete blood count (CBC) that evaluate erythrocytes, including morphologic examination on the peripheral blood smear.
Variation in cell size.
“Stack” of red blood cells resembling a roll of coins; prominent in equine and often feline blood. Formation increases as negative charges between RBCs decrease (e.g. with increased plasma proteins).
Increase in the number of neutrophils in peripheral blood.
Release of less mature neutrophil stages (bands, metamyelocytes, myelocytes) from the marrow into the peripheral blood in response to inflammation.
Cytoplasmic abnormalities seen in neutrophils that have not matured normally in the bone marrow. Abnormalities include retention of primary granules, vacuolation, darker staining due to retention of ribosomes, and deposits of rough endoplasmic reticulum (Döhle bodies).
Increase in the number of monocytes in peripheral blood.
Azotemia due to renal disease.
Lipid used to form cell membranes, steroid hormones, bile acids, and vitamin D.
Impaired bile flow.
All tests on the CBC that evaluate leukocytes. Also, that part of the leukon which is evaluated by examination of a peripheral blood sample (typically does not include leukocyte precursors).
Abnormal uncontrolled growth of cells that are unresponsive to normal physiologic growth controls; may be benign or malignant.
Decrease in hematocrit (PCV) recognized on the complete blood count (CBC); usually hemoglobin concentration and RBC numbers are also decreased.
Organ responsible for production of hemopoietic cells; found in the medullary cavity, especially the ends of long bones (e.g. femur) and flat bones (e.g. the pelvis, sternum.)
Volume of erythrocytes per liter of whole blood. Reported as L/L (calculated: MCV x RBC count). Equivalent to PCV (%) determined by centrifugation of blood in a microhematocrit tube
Increase in hematocrit (PCV) in peripheral blood; usually accompanied by increases in hemoglobin and RBC numbers.
Azotemia due to extracellular fluid volume depletion (dehydration).
Break-down product of hemoglobin.
Nonspecific term for sublethal or lethal injury to hepatocytes due to various causes, e.g. hypoxia, toxins, infection.
Heme protein responsible for oxygen transport in muscle.
Increase in blood pH above normal.
Amount of acid or base that needs to be added to bring the pH of blood back to normal.
Average amount of hemoglobin per erythrocyte (calculated: hemoglobin÷RBC count).

