Case Studies
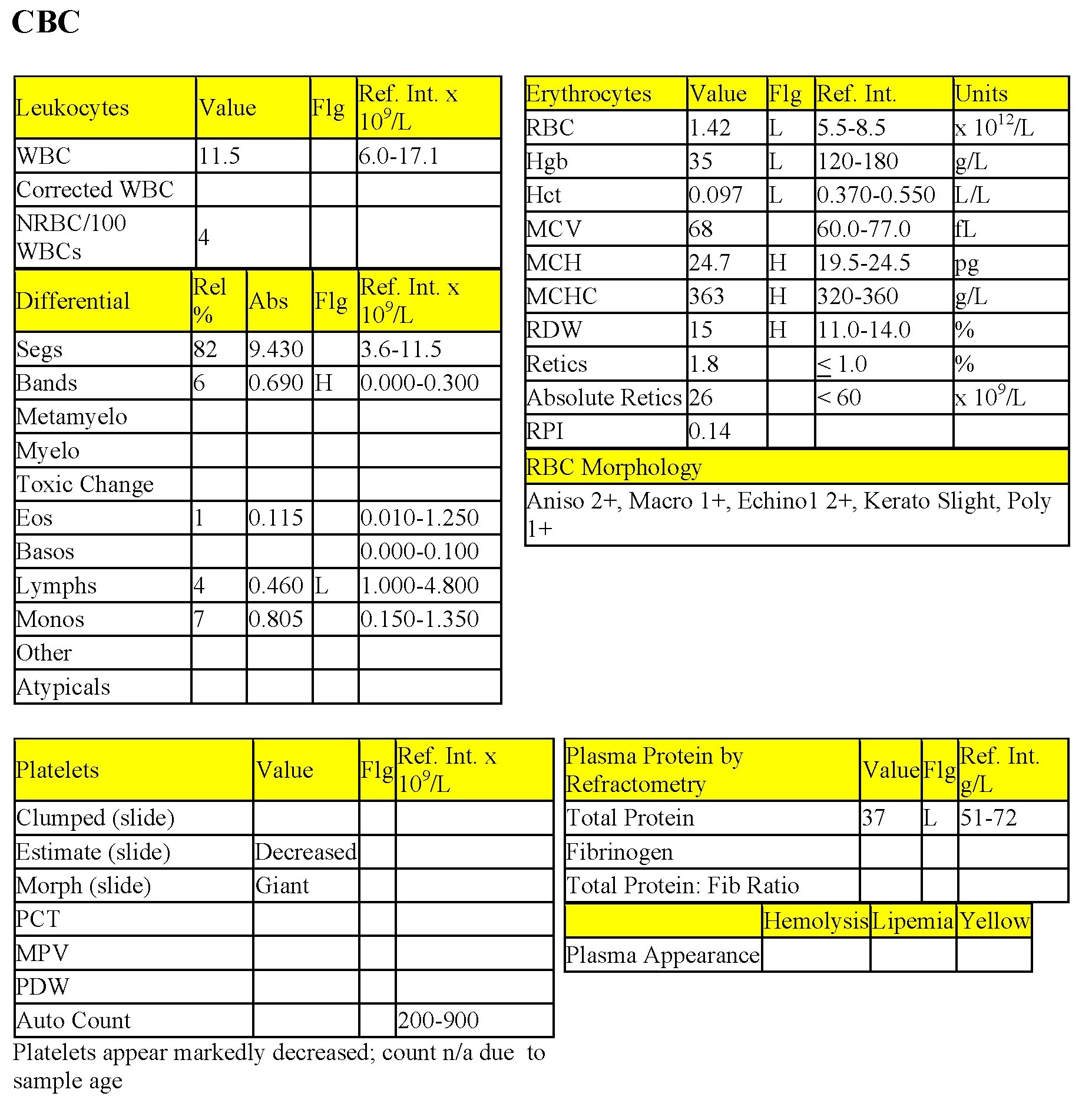
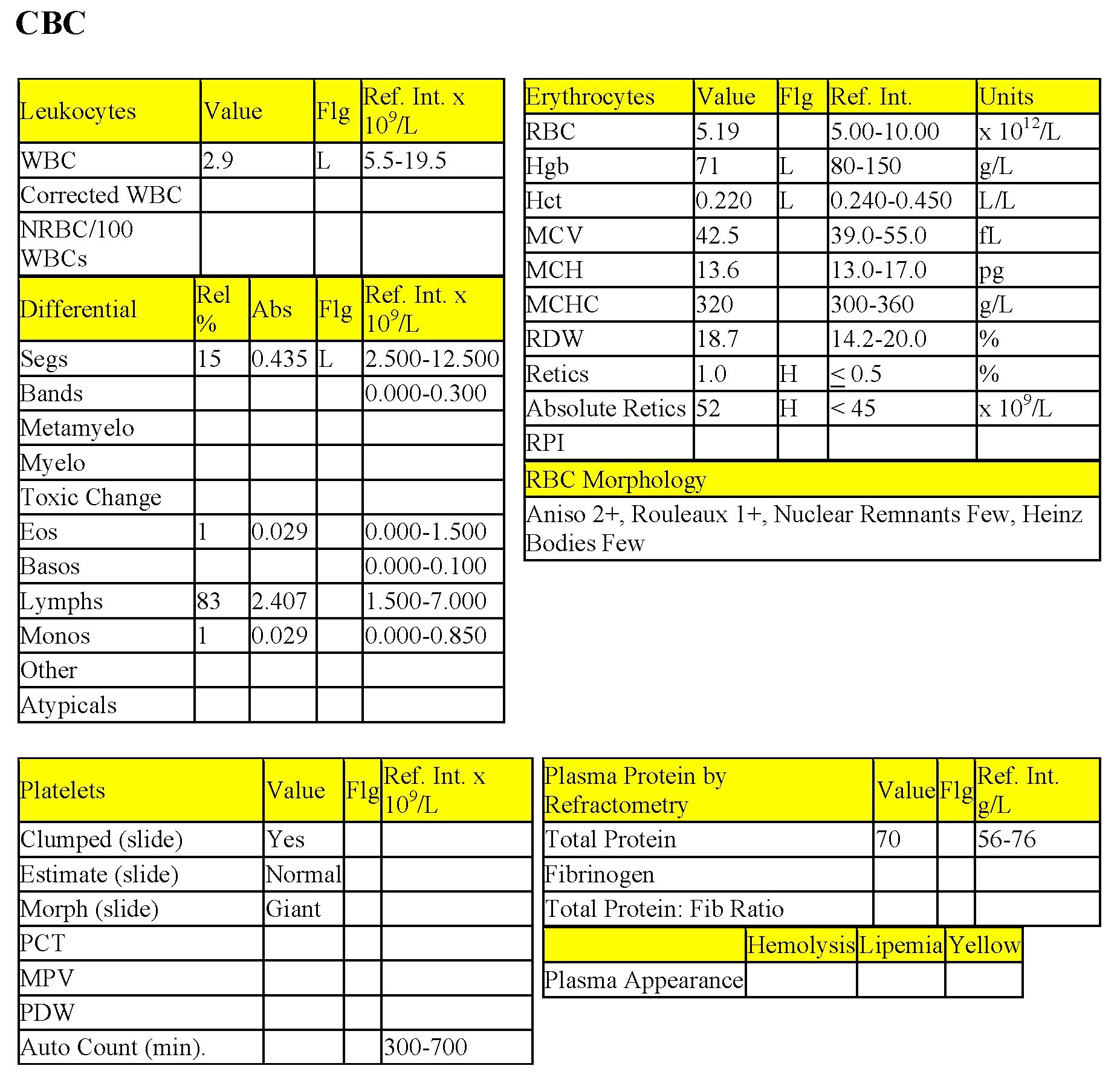
Case 1. Odie
Odie, 9-year-old M(c) Terrier X dog. History of anorexia, lethargy, and vomiting for 2 weeks.
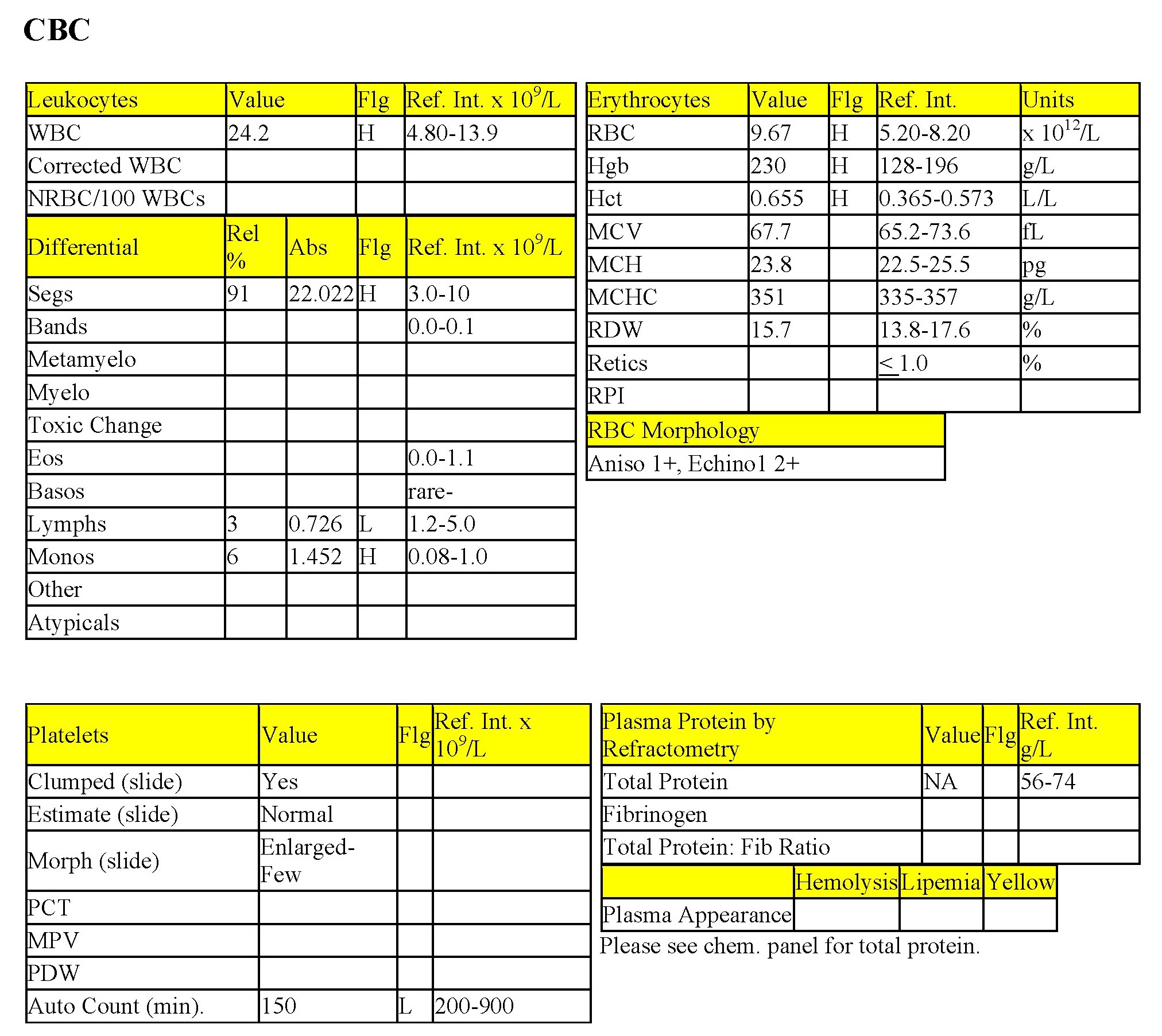
CBC
The Hct, Hgb, and RBC are all mildly to moderately elevated, indicating erythrocytosis. RBC morphology findings are not considered to be clinically significant. There is a mild to moderate leukocytosis characterized by mild to moderate neutrophilia, moderate lymphopenia, and mild monocytosis. These findings could be entirely due to stress (sustained, high levels of endogenous cortisol, in this case), however, concurrent established inflammation is also possible. Platelets are clumped but estimated to be within RI on smear evaluation. Note that the auto count, read from the automated instrument, is low due to platelet clumping, and represents a minimum value only.
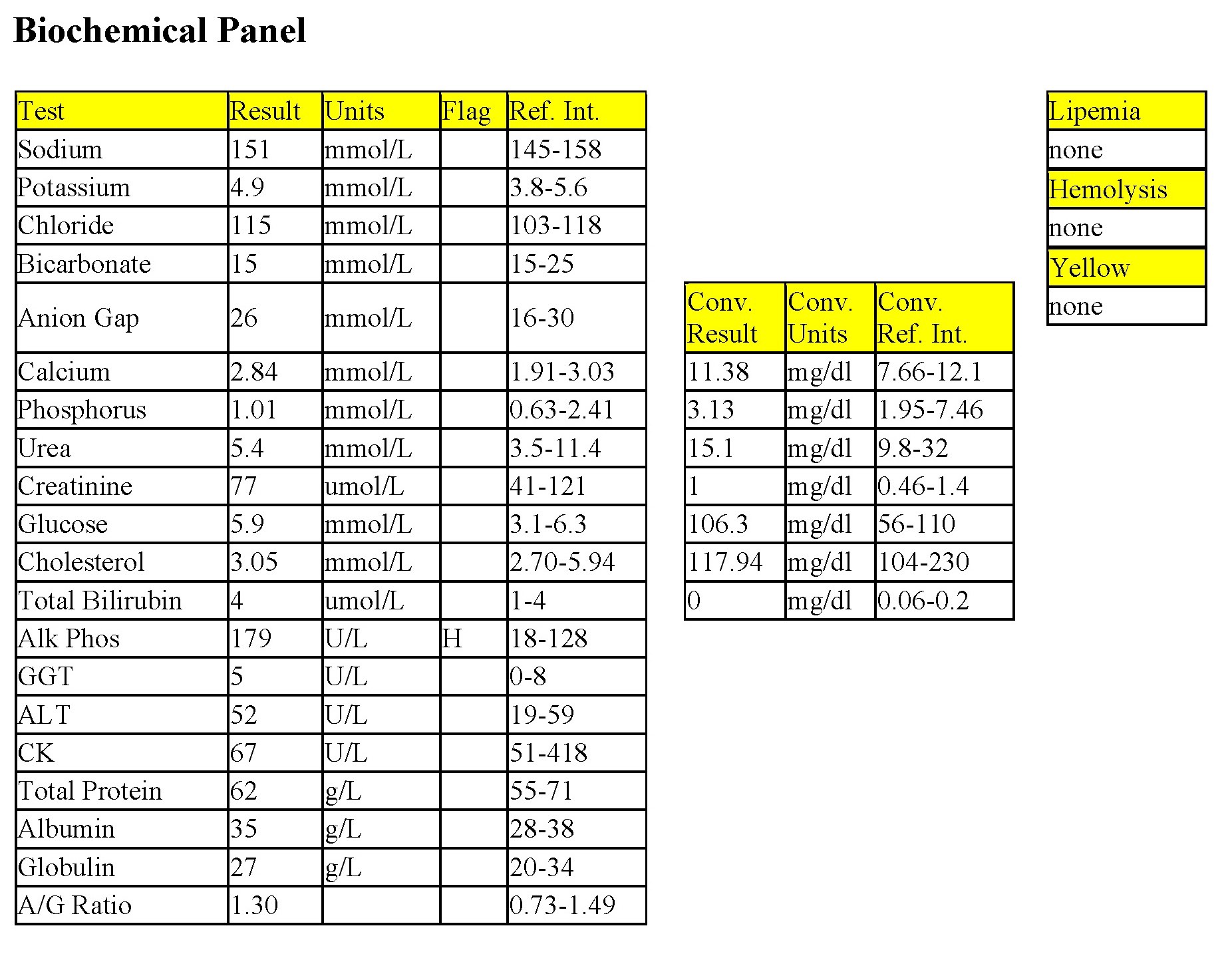
Biochemical Panel
Mild decreases in sodium and potassium, and a marked decrease in chloride may be due to decreased intake (anorexia), coupled with losses through vomiting, and replacement of electrolyte-rich fluid with electrolyte-poor fluid (assuming the patient is drinking despite the vomiting). The disproportionate decrease in chloride relative to sodium is due to selective chloride loss which can occur with gastric or duodenal foreign body, tumor, or swelling and inflammation leading to obstruction, or with gastrinoma (rare). The markedly increased bicarbonate indicates metabolic alkalosis and together with the hypochloremia, also supports upper gastrointestinal pathology and/or obstruction. The very mild increase in anion gap suggests concurrent mild metabolic acidosis, possibly due to both renal acid retention and lactic acidosis from poor tissue perfusion. Mild hypercalcemia is probably due to increased binding to protein, particularly albumin (see protein interpretation below). Mild increases in phosphorus, urea, and creatinine suggest decreased renal perfusion, likely due to dehydration (see below). Mild increases in cholesterol and bilirubin are probably due to cholestasis, which could relate to dehydration and bile inspissation (decreased fluidity). Marked hyperproteinemia is characterized by marked hyperalbuminemia, mild hyperglobulinemia and an albumin to globulin (A/G) ratio within RI.
The panhyperproteinemia and mild erythrocytosis are consistent with relative erythrocytosis related to water loss/dehydration. Urine was not obtained, but a specific gravity representing well-concentrated urine would be expected. Odie was euthanized as it was determined that he had a pyloric obstruction, possibly due to a neoplasm. A necropsy was performed and a 3 cm rubber ball was lodged at the level of the pylorus.
Note: For the purposes of presenting a case of relative erythrocytosis due to dehydration, only the erythrogram and protein concentrations require evaluation. For completeness and to explain the reason for the marked dehydration, additional laboratory data are provided. It is recommended that the reader revisit this case after studying Chapter 6. Body Water, Electrolyes, and Acid-Base Balance and Chapter 7. Renal System.
Case 2. Annie
Annie, a 12.5-year-old F Old English Sheepdog X had anorexia for 5 days. She had been polydipsic, but was no longer drinking at presentation.
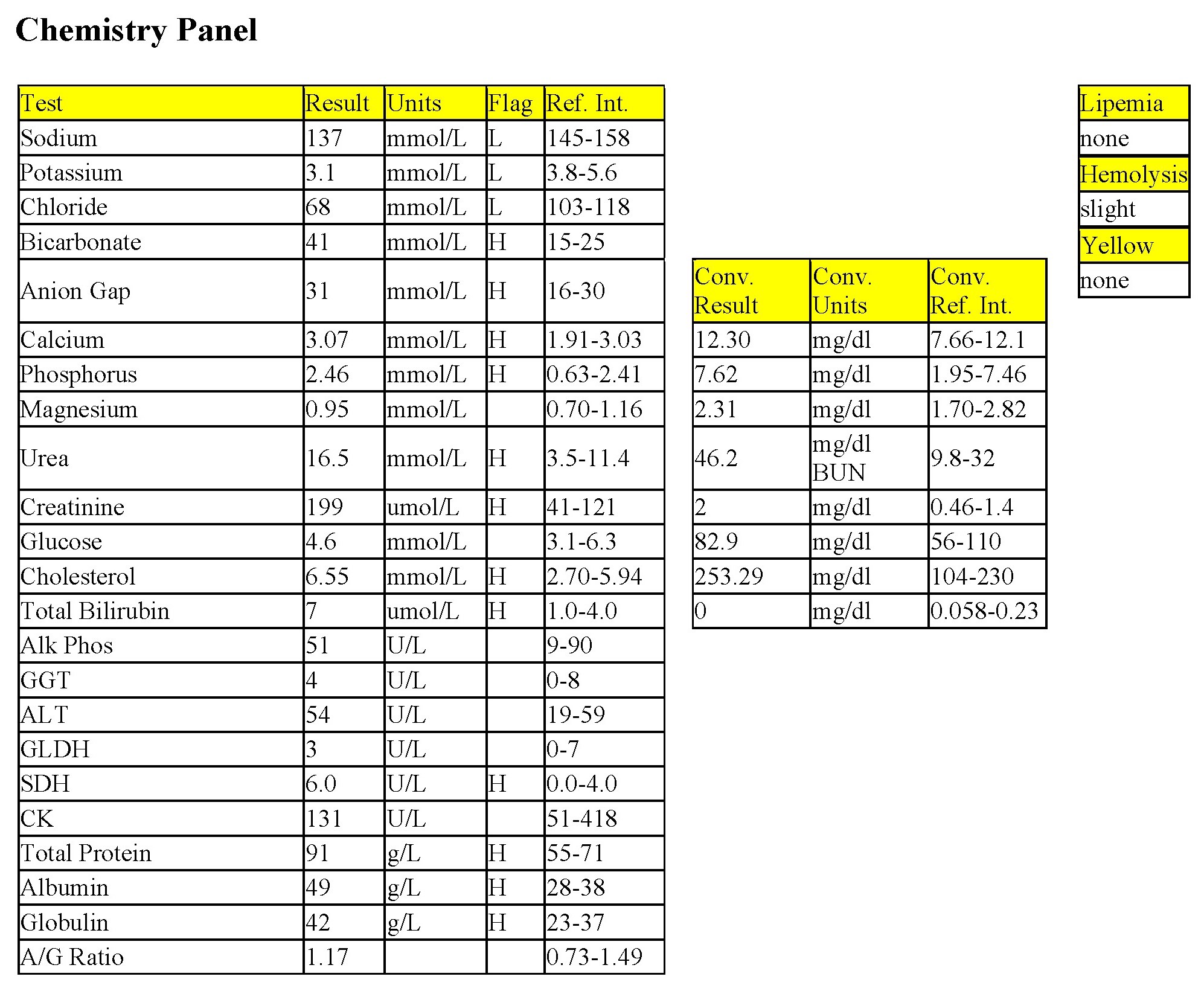
CBC
There is a mild to moderate anemia with mild regeneration. Although the reticulocyte count is 2.2%, the RPI is not increased (see Protocol Manual: RPI>1 indicates regeneration; >3 indicates strong regeneration) and there is no polychromasia noted on RBC morphology. Also, the absolute reticulocyte count is only slightly above the RI for a normal, nonanemic dog. Keratocytes at slight, may not be significant, though fibrin strand injury/shearing is possible. There is a moderate to severe leukocytosis characterized by a moderate neutrophilia with a marked left shift, toxic change, and moderate monocytosis. These leukogram changes indicate severe, ongoing inflammation. Lymphocytes are low normal, suggesting possible stress. The thrombogram and total protein are unremarkable.
Biochemical Panel
There is a mild azotemia which must be interpreted in relation to the hydration status of the dog and the USG (not available). Moderate elevations in alkaline phosphatase (ALP) and -glutamyl transferase (GGT) activities could be due to cholestasis, enzyme induction, or both. The moderate hypoalbuminemia and low A/G ratio may relate to albumin’s role as a negative acute phase protein. Albumin loss through the kidneys should also be explored by performing a urinalysis.
- The history and laboratory findings support a diagnosis of pyometra in this dog. The anemia is likely due to inflammatory disease. The leukogram abnormalities are due to the demand for phagocytic cells within the uterus. Following ovariohysterectomy in such cases, neutrophil numbers will rise/rebound due to the presence of granulocytic hyperplasia in the bone marrow and the abrupt removal of the site of increased demand for neutrophils. The anemia of inflammatory disease will start to correct with resolution of the inflammation. Endotoxin release related to the pyometra may interfere with ADH activity in the renal tubules, resulting in polyuria and polydipsia. Endotoxin can also cause renal damage with secondary azotemia from tubular damage. The chronic infection/pyometra may result in deposition of antigen/antibody complexes in glomeruli resulting in proteinuria (mainly albumin) and hypoalbuminemia. These too would be expected to resolve following ovariohysterectomy, unless renal pathology was pre-existing or irreversible.
Case 3. Elmo
Elmo, an 8-month-old M Poodle dog was presented in shock with white mucous membranes.
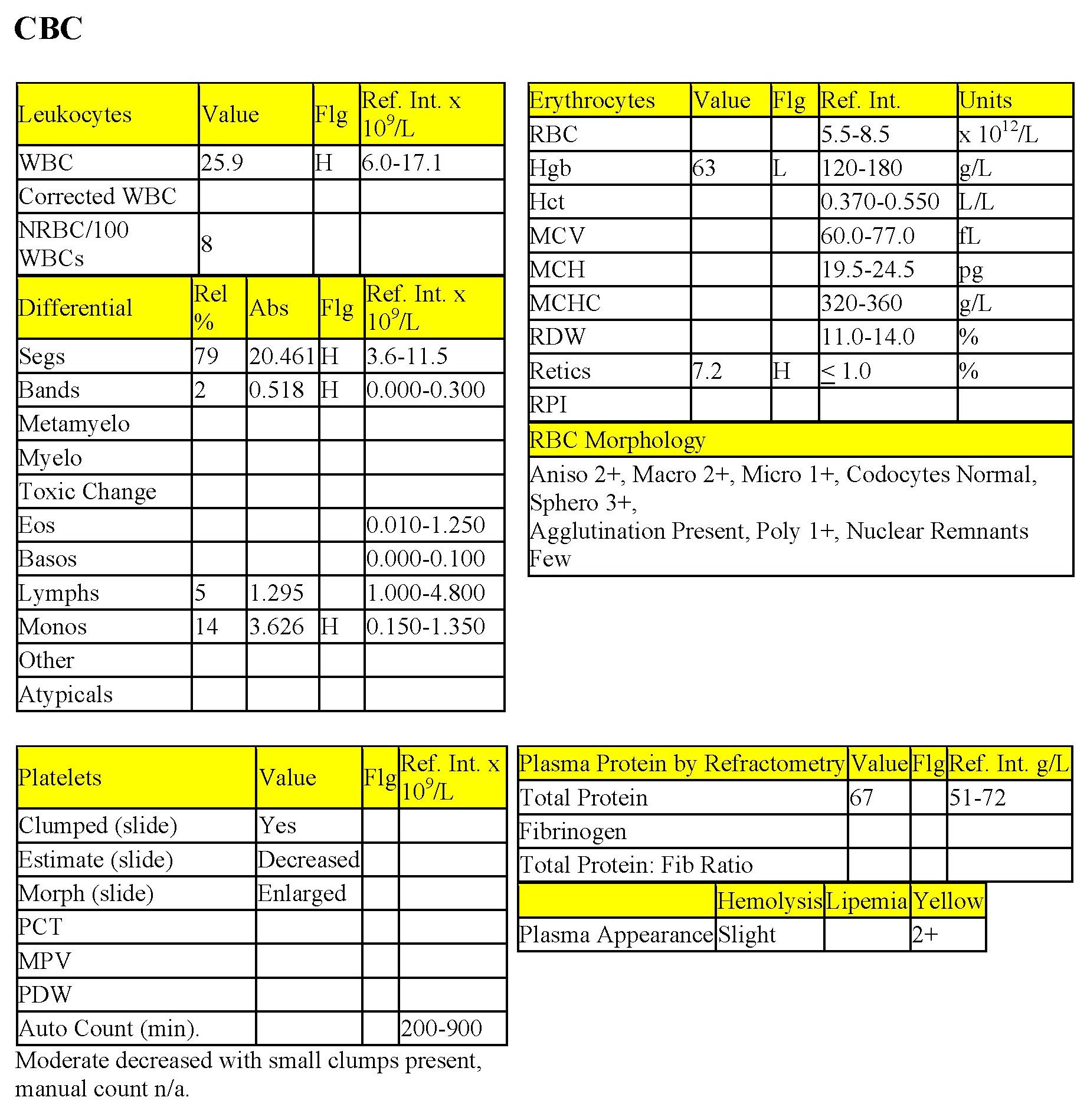
CBC
The Hct, Hgb, and RBC count are all severely decreased. Anisocytosis at 2+, macrocytosis, 1+ polychromasia, and mildly increased reticulocyte % suggest very mild/early regeneration, although the absolute reticulocyte count and RPI do not reflect regeneration at this time. Severe hypoproteinemia and severe anemia suggest acute/ongoing blood loss. Platelet numbers are decreased, although an absolute platelet count is not available. Severe hemorrhage, internal or external, can result in significant platelet loss. Absolute numbers do not usually decrease below about 80x 109/L as a result of acute severe hemorrhage, in the dog. Mild bleeding is unlikely to result in a significant drop in platelet numbers. Platelet numbers of <50 x 109/L could result in spontaneous hemorrhage due to a primary hemostatic disorder. If thrombocytopenia were the cause of the anemia in this patient, one would expect superficial bleeding, such as petechiation, epistaxis, melena, hematochezia, hyphema, etc. (see Chapter 4. Hemostasis). Total WBC count and mature neutrophil numbers are within RI; however, there is a mild left shift and moderate lymphopenia. Given the state of shock in which the animal was presented, these leukogram changes could be entirely due to stress. Concurrent mild, acute inflammation cannot be ruled out.
- Elmo had ingested rodenticide which contained a vitamin K antagonist. The dog had been bleeding into his chest cavity. Sufficient time had lapsed for low protein interstitial fluid to move into the intravascular space in an attempt to correct the hypotension. Acute/ongoing severe blood loss, whether internal or external, is typically accompanied by hypoproteinemia. Indications of regeneration should start to appear within 2-4 days of the onset of the anemia in dogs. No additional information is available for this patient.
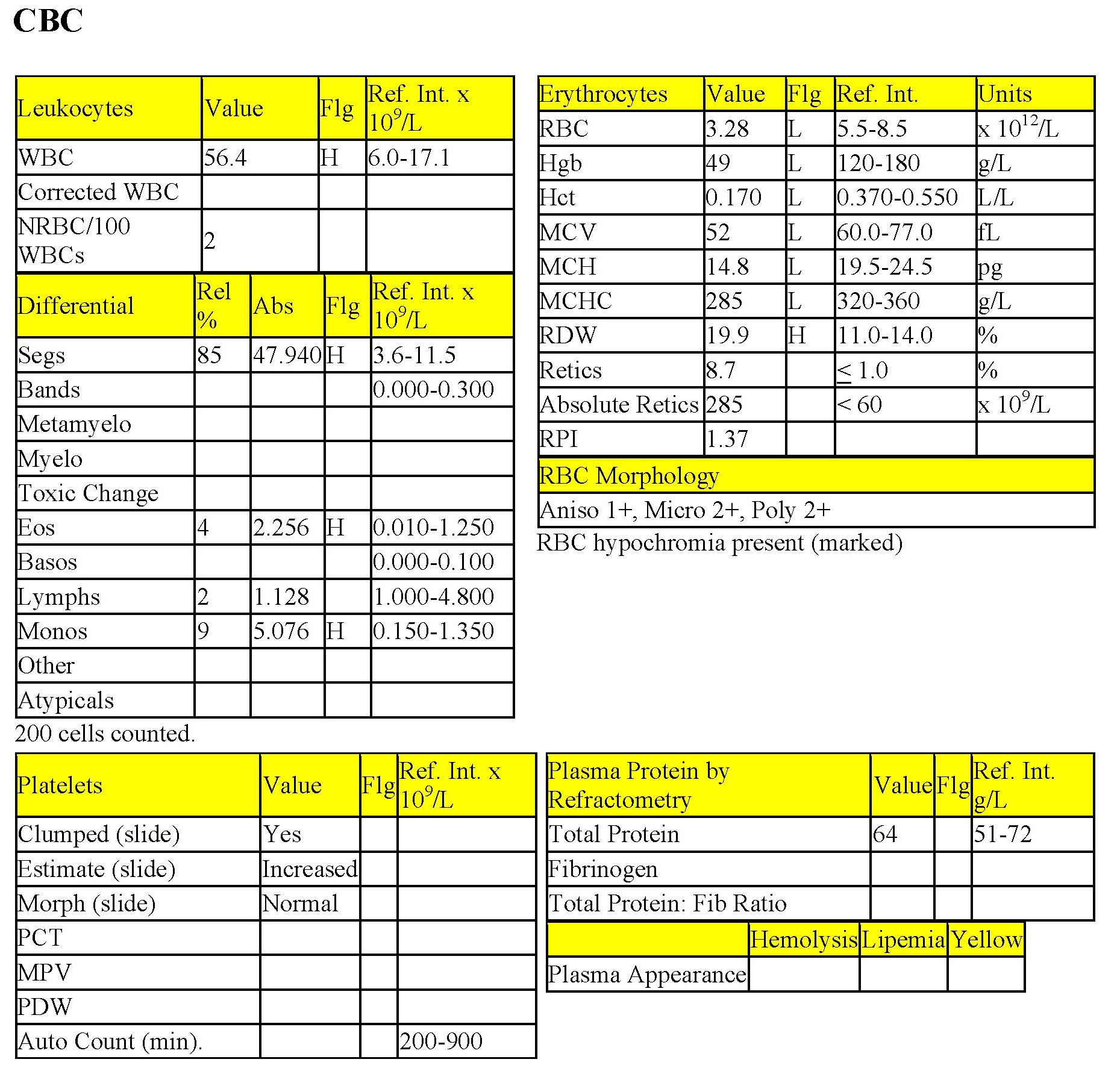
Case 4. Ricky
Ricky, a 14-year-old M(c) German Wirehair Pointer dog, was lethargic and had diarrhea (possibly with melena), and pale mucous membranes.
CBC
There is a severe anemia which is microcytic (low MCV and microcytosis on RBC morphology), hypochromic (low MCH and MCHC, and hypochromia noted on RBC morphology), and moderately regenerative (increased reticulocyte % and absolute numbers, increased RPI, and 2+ polychromasia on smear examination). These erythrogram findings suggest iron deficiency anemia. The leukogram changes include a moderate to marked leukocytosis characterized by a moderate to marked neutrophilia, moderate monocytosis, and mild to moderate eosinophilia. Lymphocyte numbers are low normal. The leukogram findings suggest chronic inflammation; eosinophilia may be due to concurrent eosinophilic inflammation, allergic disease, parasitic disease, mast cell neoplasia, or a paraneoplastic mechanism (seen most commonly with lymphoid neoplasms). Concurrent stress is likely given the borderline low lymphocyte count. Platelet numbers are increased. Thrombocytosis may accompany iron deficiency although the mechanism is not well understood. One possible explanation is based on the degree of homology between erythropoietin and thrombopoietin, such that with the long term increase in erythropoietin, expected in cases of iron deficiency anemia due to chronic blood loss, thrombopoiesis is inadvertently stimulated as well. Also, platelets may be involved in any concurrent inflammatory processes.
- Ricky was diagnosed with an intestinal leiomyosarcoma, based on histopathology, which had resulted in mucosal ulceration in the duodenum, chronic blood loss, and iron deficiency. The inflammatory leukogram probably also related to the focus of ulceration as no other explanation could be found for these changes. Iron deficiency anemia in older dogs is usually caused by intestinal ulceration from chronic non-steroidal anti-inflammatory drug administration or by intestinal neoplasia. Careful history taking and ancillary testing, such as imaging studies, should help differentiate the two.
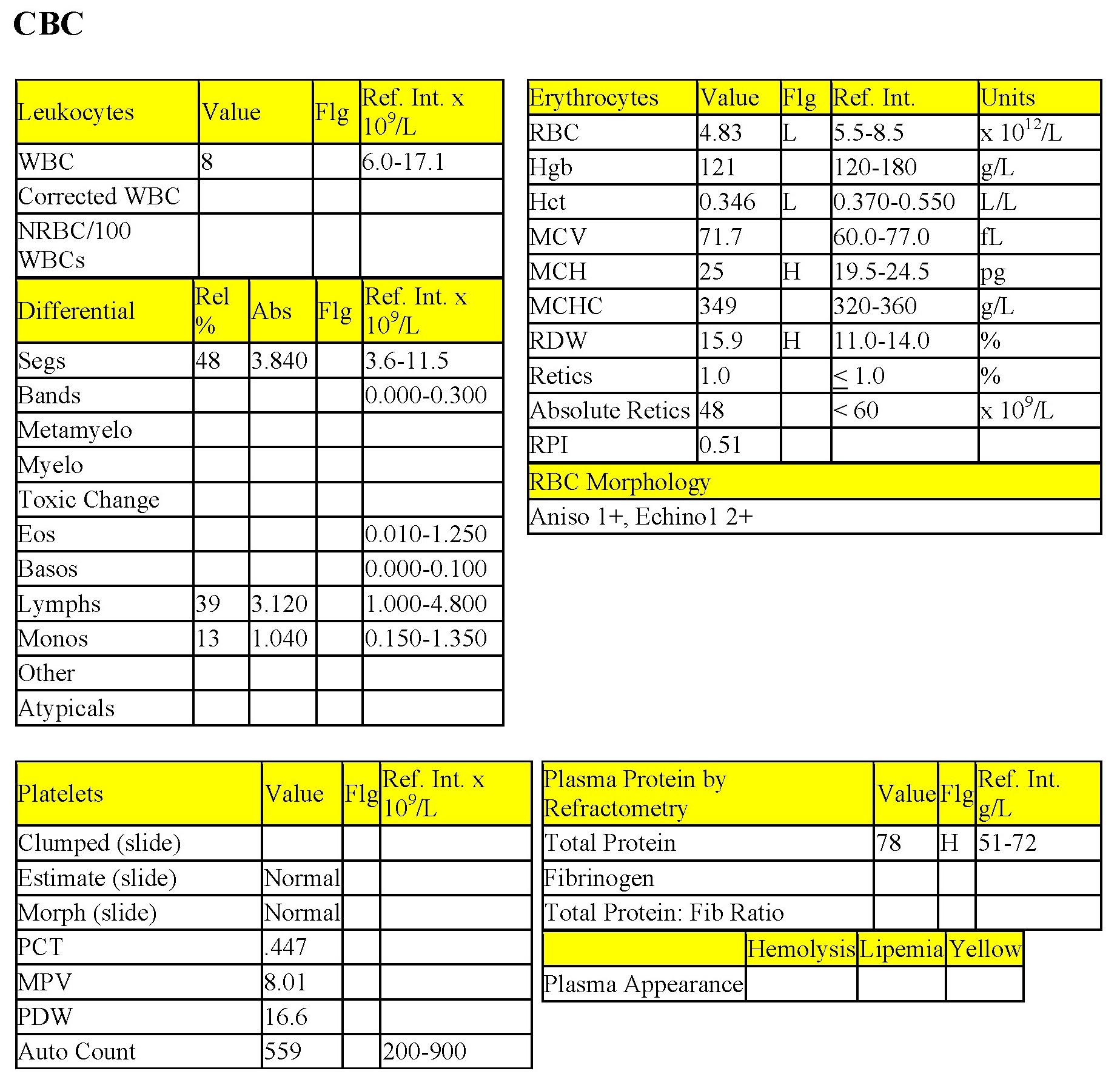
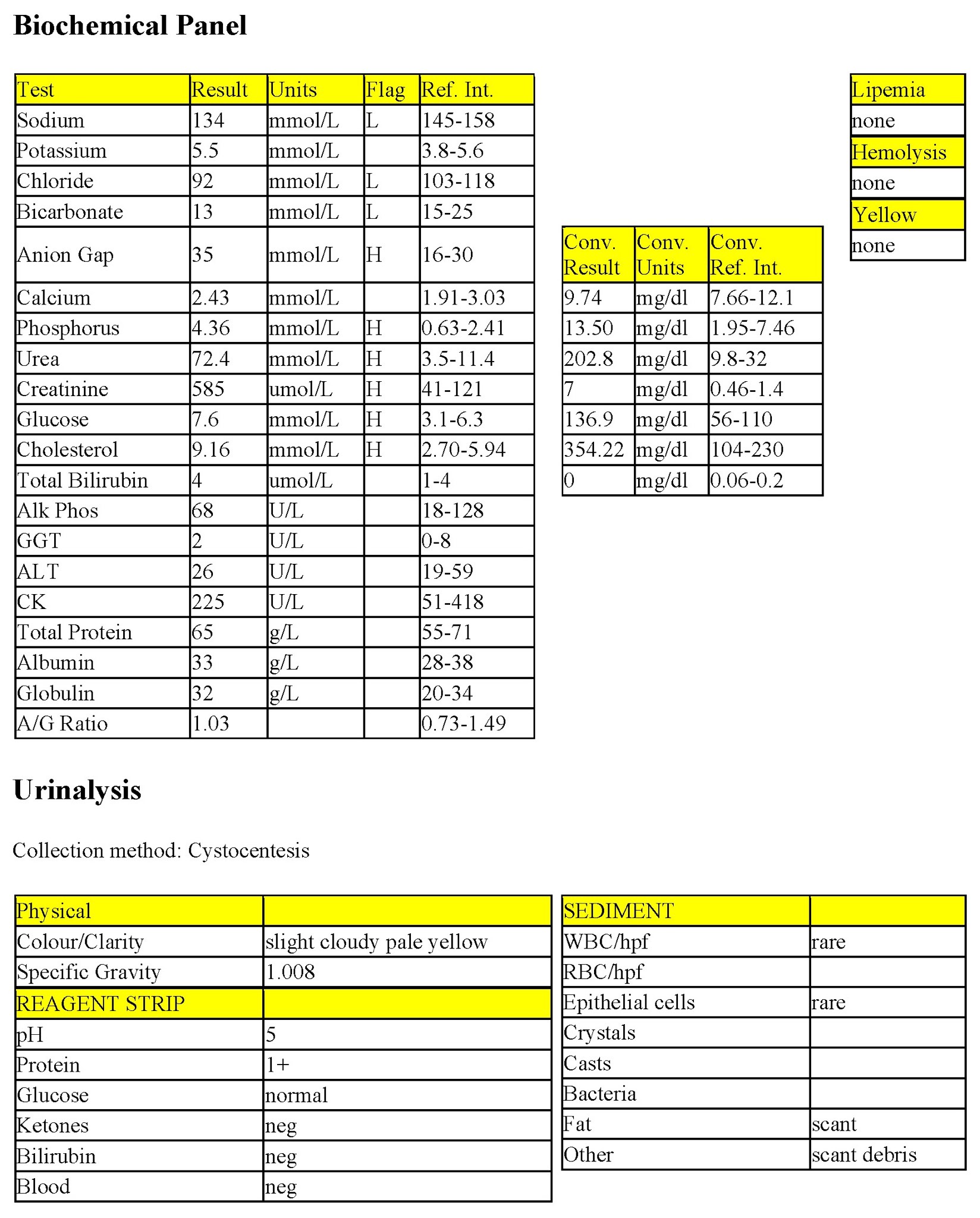
Case 5. Pansy
Pansy, a 5-year-old F(s) Jack Russell Terrier dog, had polydipsia, polyuria, and weight loss.
CBC
Mild decreases in Hct, RBC count and low normal Hgb indicate mild anemia which is nonregenerative (reticulocytes only 1%, absolute reticulocyte numbers not increased, RPI of <1, and no polychromasia on smear examination). The remainder of the CBC is unremarkable. Total proteins, at 78 g/L does not correlate well with the total protein on the biochemical panel (65 g/L), probably due to an interfering substance such as cholesterol.
Biochemical Panel
Sodium and chloride are decreased to the same degree, likely from a failure of the kidneys to conserve these electrolytes. Potassium is high normal and may also relate to failing kidneys and decreased excretion of this electrolyte. There is a high anion gap metabolic acidosis; retention of renal acids is a likely cause. Moderate elevations in phosphorus, urea, and creatinine, together with isosthenuria, confirm the diagnosis of renal disease. Mild hyperglycemia and hypercholesterolemia should be interpreted relative to whether Pansy had been fasted prior to blood collection. Hypercholesterolemia can accompany protein-losing nephropathy, which could be present in addition to renal tubular disease in this case.
Urinalysis
The “fixed” urine specific gravity (USG) (isosthenuria = SG of 1.008 – 1.012) indicates an inability to concentrate urine when accompanied by the moderate azotemia. Protein 1+ may be significant at this SG; however, a urine protein/creatinine (UPC) ratio would be required to determine if there is significant proteinuria.
- Pansy has renal disease which is probably chronic given the history and the presence of nonregenerative anemia. The anemia of chronic renal disease is mainly caused by decreased synthesis of erythropoietin, along with other mechanisms previously described.
Case 6. Thea
Thea, a 2-year-old F(s) DLH cat, had lethargy for several weeks. The owner reported improvement while on antibiotics, followed by relapse.
CBC
Thea has a mild nonregenerative anemia (low Hct and Hgb, and low normal RBC count). RBC morphology is unremarkable. Nuclear remnants and Heinz bodies are common in feline blood and are often not significant unless, in the case of Heinz bodies, there is evidence of hemolytic anemia. Heinz body hemolytic anemia is usually regenerative and the Heinz bodies are large relative to the ones commonly seen in cats. There is a moderate leukopenia characterized by severe neutropenia. There is no left shift or toxic change which suggests that the neutropenia is from lack of production rather than from increased demand (inflammatory disease). The remainder of the leukogram, the thrombogram, and the total protein are within RI. Bicytopenia (nonregenerative anemia and neutropenia) points to a bone marrow disorder. Bone marrow examination would be required to determine if neoplasia, hypoplasia, myelodysplasia, or other marrow pathology is present.
- Enzyme-linked immunosorbent assays (ELISA) were done to detect feline leukemia virus (FeLV) antigen and feline immunodeficiency virus (FIV) antibody. Thea was positive for FeLV. Thea lived for 2 more years before succumbing to erythrocyte neoplasia. Although the neutropenia resolved, the anemia worsened and remained nonregenerative. Thea developed erythrocyte macrocytosis (high MCV), probably from asynchronous maturation of the cytoplasm and nucleus in the bone marrow (megaloblastic change, 1.20). Thea’s last peripheral blood sample contained very high numbers of nucleated erythrocytes, rubriblasts through to metarubricytes, without any polychromasia and no reticulocytes seen on NMB staining. These findings suggested the possibility of erythrocytic sarcoma/erythremic myelosis, one of the acute myeloid neoplasms (see Chapter 3. Hemopoietic Neoplasia). Bone marrow was not examined.
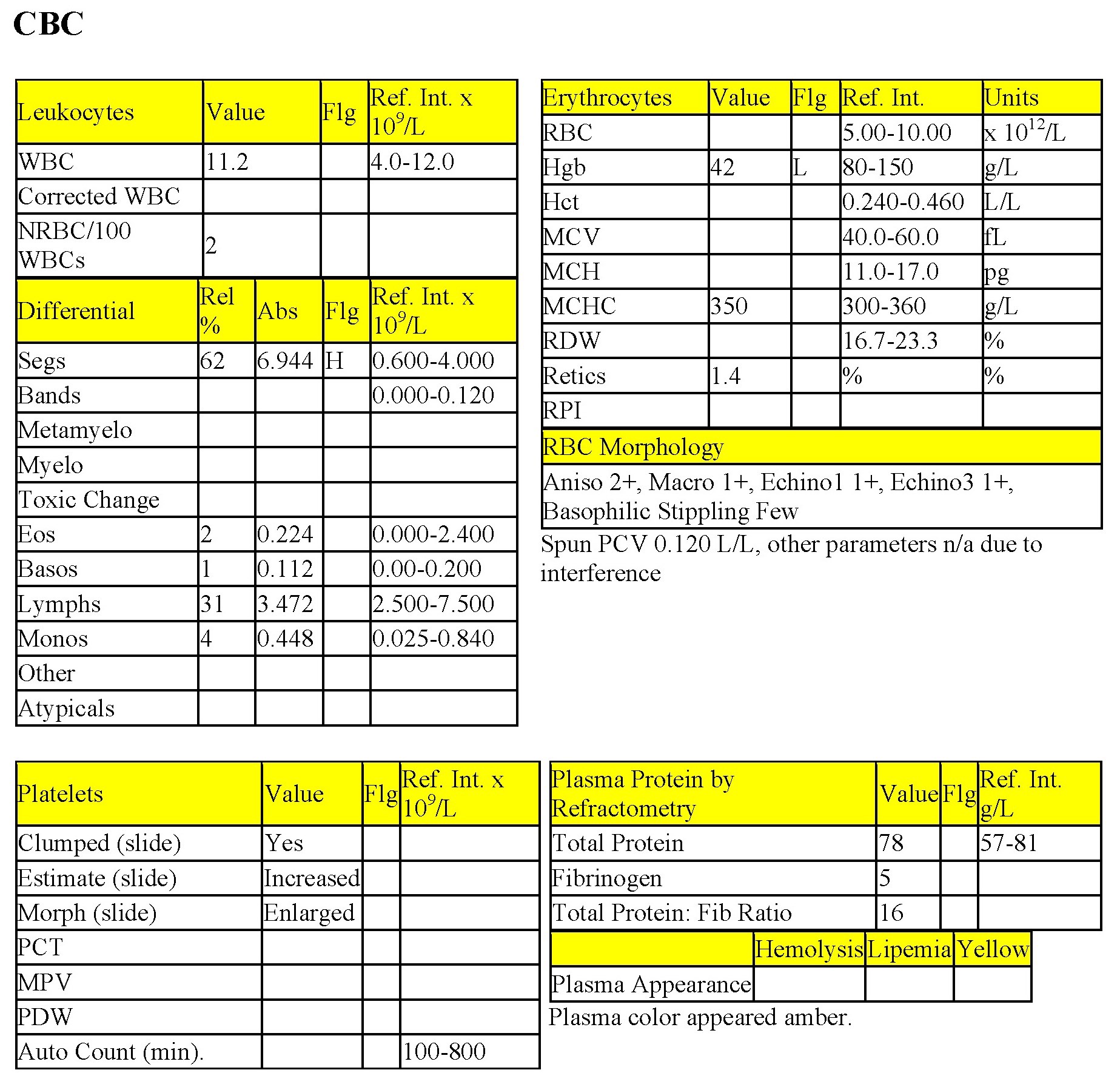
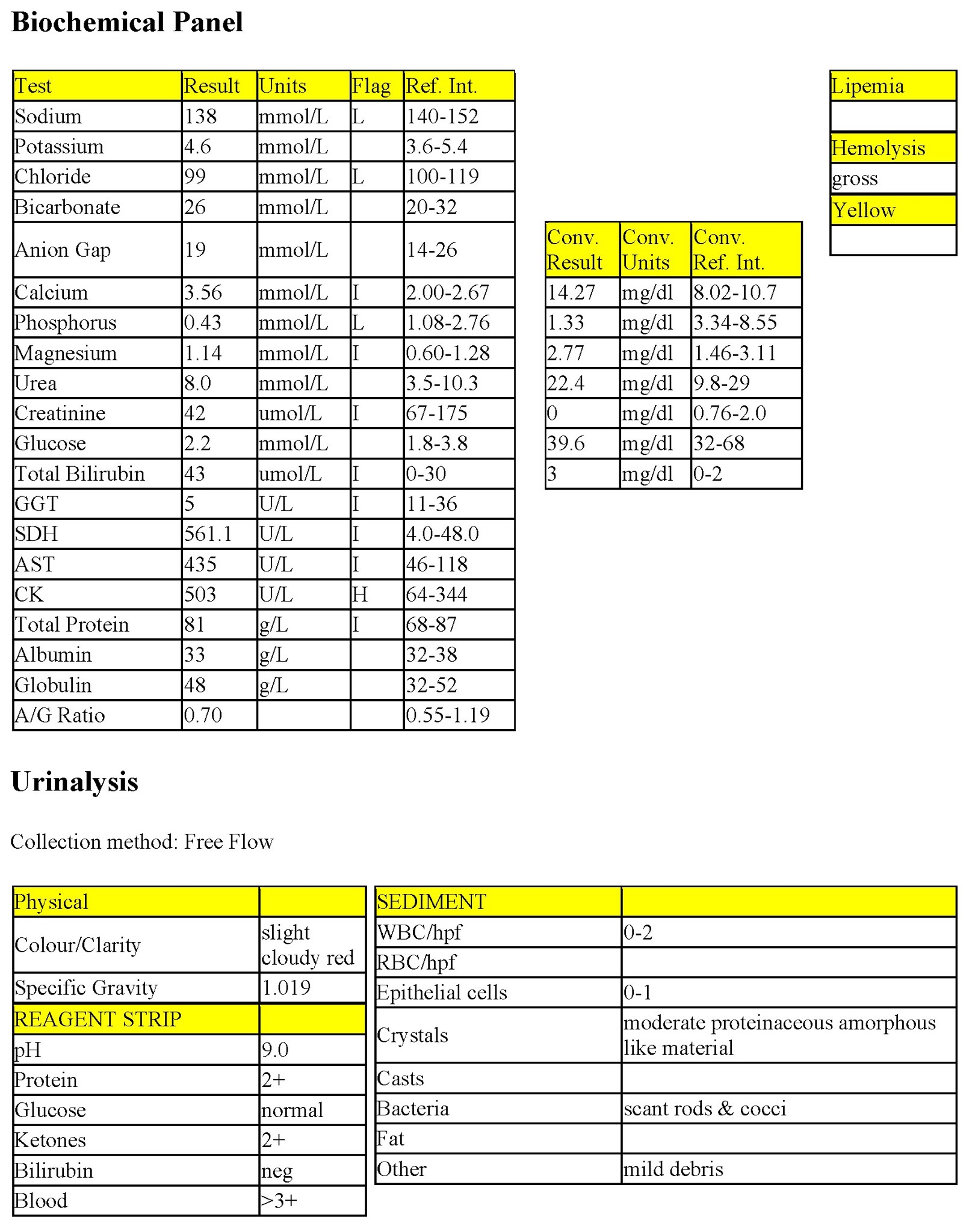
Case 7. Gerda
Gerda, a 10-year-old Jersey cow, calved 2 weeks earlier without difficulty. When presented, she had bloody urine for 1 week and was inappetent.
CBC
There is a severe anemia with some evidence of very mild/early regeneration. Although polychromasia is not noted, there are other subtle indicators of regeneration: reticulocytes are slightly increased, and nucleated RBCs, basophilic stippling and macrocytes are present. Other RBC parameters could not be obtained due to gross hemolysis of the sample. The cause of the increased platelet numbers is not known, but thrombocytosis can accompany inflammatory processes. Total WBC count is high normal and there is a mild neutrophilia, possibly due to stress, inflammation, or both. Total protein is high normal. The fibrinogen is <7 g/L, which does not support inflammation; however, hyperfibrinogenemia is not a consistent finding with inflammation and levels can fluctuate quickly.
Biochemical Panel
Hemolysis has interfered with many of the measurements on the biochemical panel (I = interference). Sodium and chloride are slightly decreased, probably from decreased intake. Phosphorus is moderately decreased, which could relate to low phosphorus in the diet as well as increased losses. Creatine kinase (CK) activity is only mildly increased so significant muscle injury is not present. Although interference is present, aspartate aminotransferase (AST) and sorbitol dehydrogenase (SDH) activities are likely increased suggesting hepatocellular injury/leakage, probably from the severe anemia (hypoxic hepatic damage).
Urinalysis
The urine is red and positive on the reagent strip for blood. Hemoglobin, intact RBCs, and myoglobin in the urine can all produce a positive blood reaction. RBCs were not seen on the sediment examination and there is unlikely to be myoglobinuria given the lack of increase in CK activity. Also, the hemolysis noted on the plasma and serum would correlate with hemoglobinuria. Hemoglobinuria may also account for the protein at 2+. Ketonuria is due to negative energy balance in this cow. Free flow collection of the urine probably explains the presence of debris, amorphous material, and scant bacteria seen on urine sediment examination. There is no evidence of urinary tract inflammation.
- Intravascular hemolysis is occurring and although red urine has been seen for several days, RBC regeneration is only beginning. Reticulocyte numbers would be expected to increase over the following few days. The hypophosphatemia and other laboratory and historical findings lead to a diagnosis of postparturient hemoglobinuria/hypophosphatemia. Gerda had experienced a similar problem with her previous calving. She responded to supportive therapy (no blood transfusion) and recovered fully.
Case 8. O’Reilly
O’Reilly, a 3-year-old male DSH cat, had been adopted from the SPCA 2 years previously and had not received vaccinations since that time. He was thin, icteric, and dehydrated.
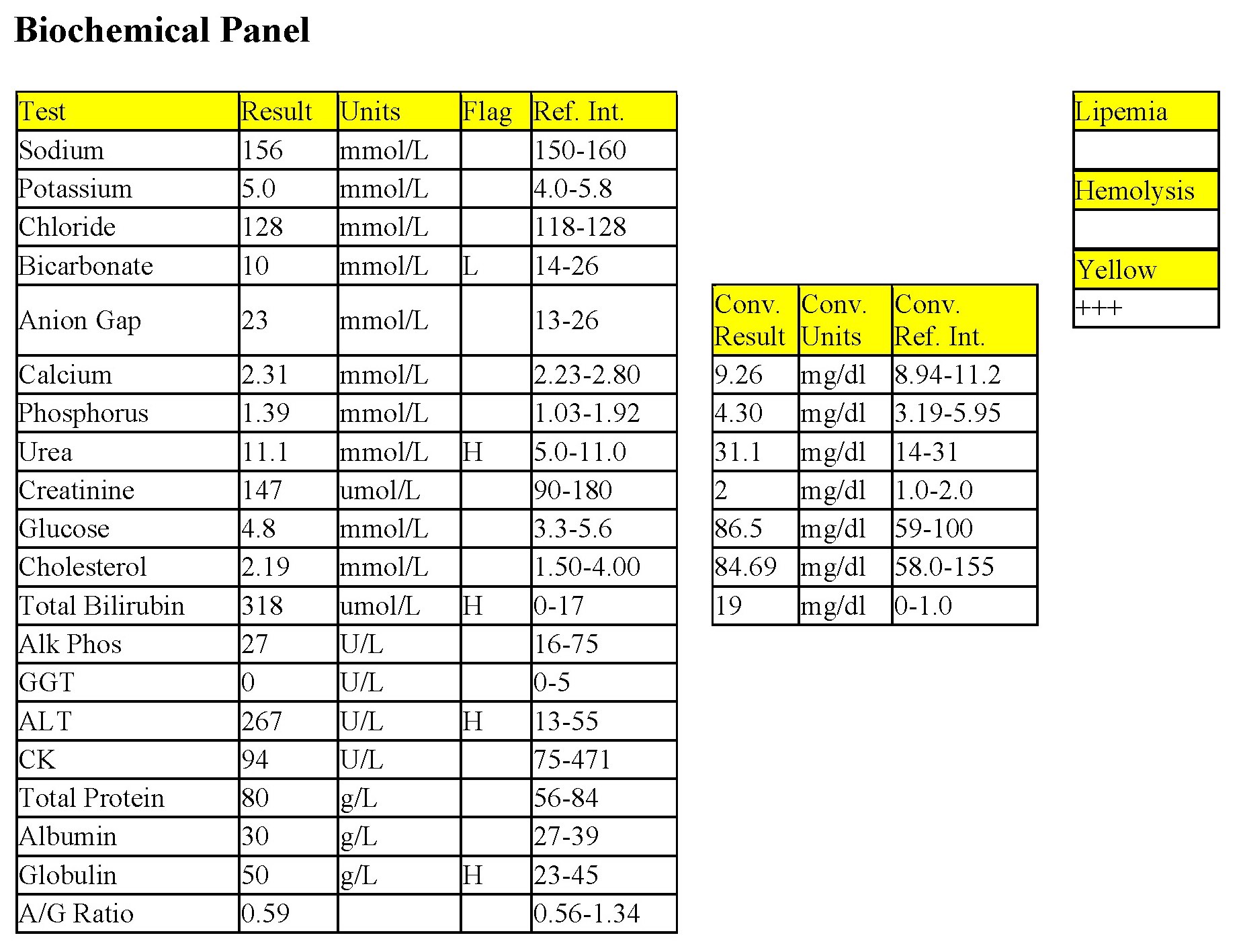
CBC
Marked decreases in Hct, Hgb, and RBC count indicate severe anemia which is moderately to markedly regenerative (very high reticulocyte %; high absolute reticulocyte count; increased MCV from increased numbers of large, immature RBCs; polychromasia; basophilic stippling; macrocytosis; nucleated RBCs). All leukocyte numbers are within RI. The lack of lymphopenia in an obviously stressed (high levels of endogenous glucocorticoid) or ill animal could be due to one of many reasons: epinephrine response – cats and young horses may release lymphocytes into the circulation when very excited, a likely explanation in the case of O’Reilly; lymphocytic leukemia; antigenic stimulation from recent vaccination (especially in young animals receiving a vaccination series) or other antigenic stimulation; the animal is not as stressed/ill as thought; lack of glucocorticoid (hypoadrenocorticism, which is predominantly a disease of dogs). Total protein (by refractometry) is increased and total protein is high normal on the biochemical panel. Volume contraction is likely, particularly given the history. Yellow plasma correlates with hyperbilirubinemia (see below).
Biochemical Panel
The metabolic acidosis (low bicarbonate) is not due to acid gain, but rather, to bicarbonate loss (anion gap not elevated). High normal urea could be due to decreased renal perfusion; this may not be reflected in the creatinine concentration if the patient has low muscle mass. There is a marked hyperbilirubinemia which, in this case, is due to extravascular hemolysis. Hypoxic injury to hepatocytes explains the increased alanine aminotransferase (ALT) activity.
- O’Reilly is experiencing extravascular hemolysis from Mycoplasma haemofelis infection (Fig. 1.12). This extracellular organism becomes intimately associated with the RBC membrane, and is recognized as a foreign antigen by the MPS. Affected RBCs are phagocytized resulting in extravascular hemolytic anemia. Icterus (hyperbilirubinemia) develops as RBCs are degraded by macrophages and biliburin is transported to the liver for conjugation and excretion. Although the organism was seen on RBCs in O’Reilly’s blood smear (information not provided earlier), this is not always the case. Polymerase chain reaction testing is available to confirm infection with this organism when it cannot be identified on blood smear evaluation. This test can also differentiate between Mycoplasma haemofelis and Mycoplasma haemominutum, the latter of which is considered to be a less pathogenic organism. O’Reilly recovered with appropriate therapy although it is controversial whether animals ever completely eliminate the organism, which may reside in a latent state in the spleen.
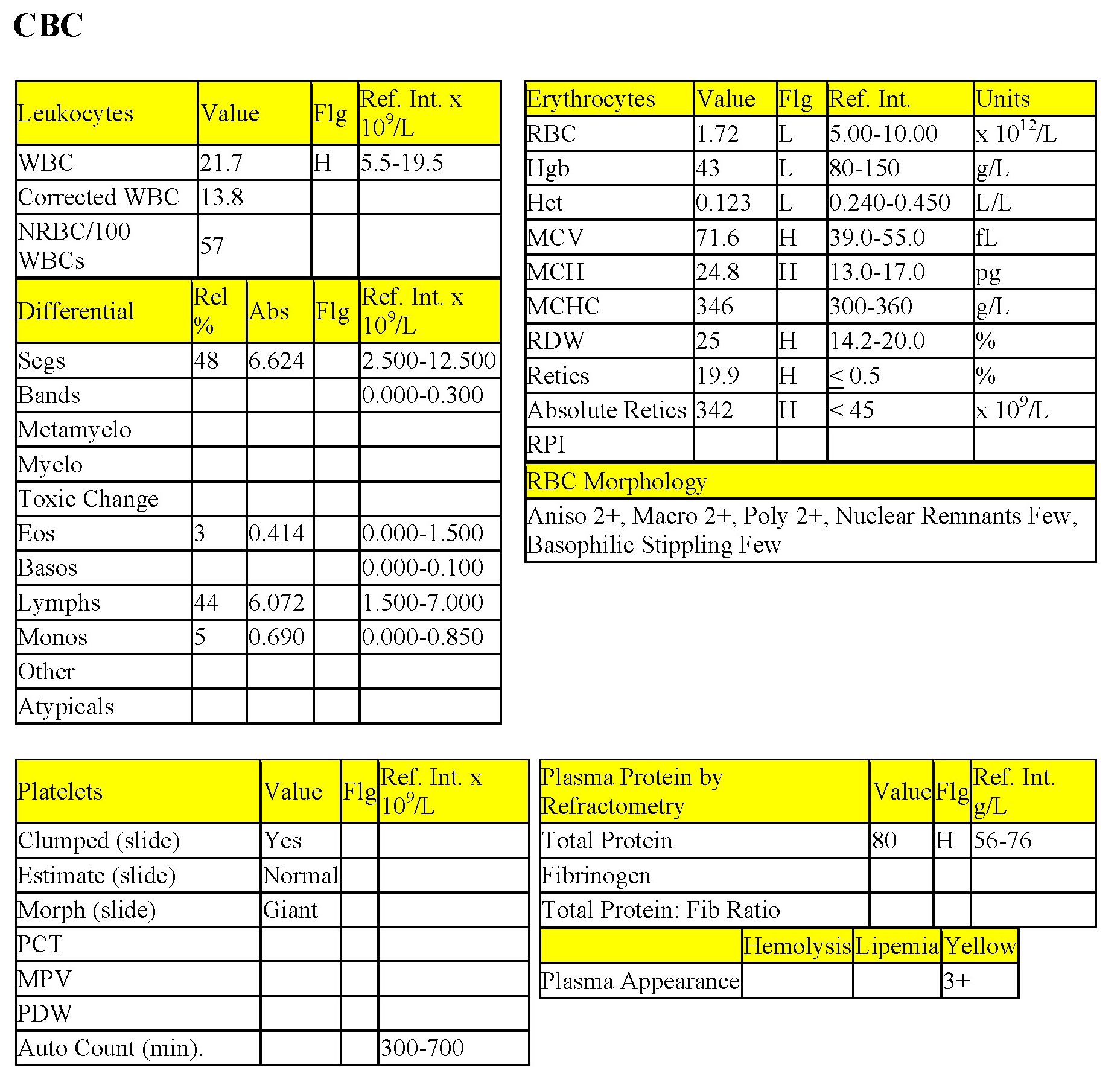
Case 9. Skippy
Skippy, a 12-year-old F Border Collie X dog, had been lethargic for a few days. She had a transient episode of unconsciousness on the day prior to examination.
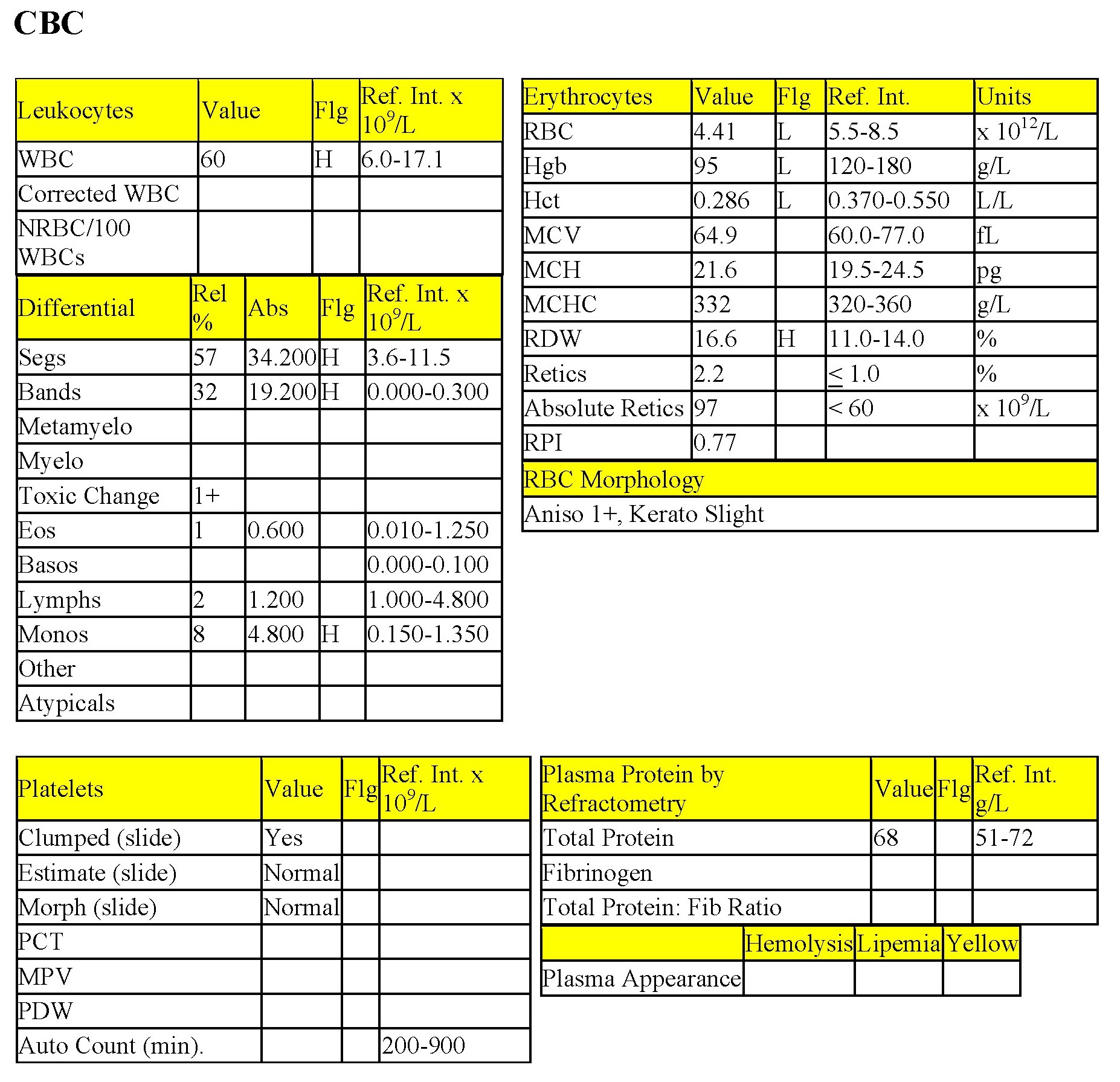
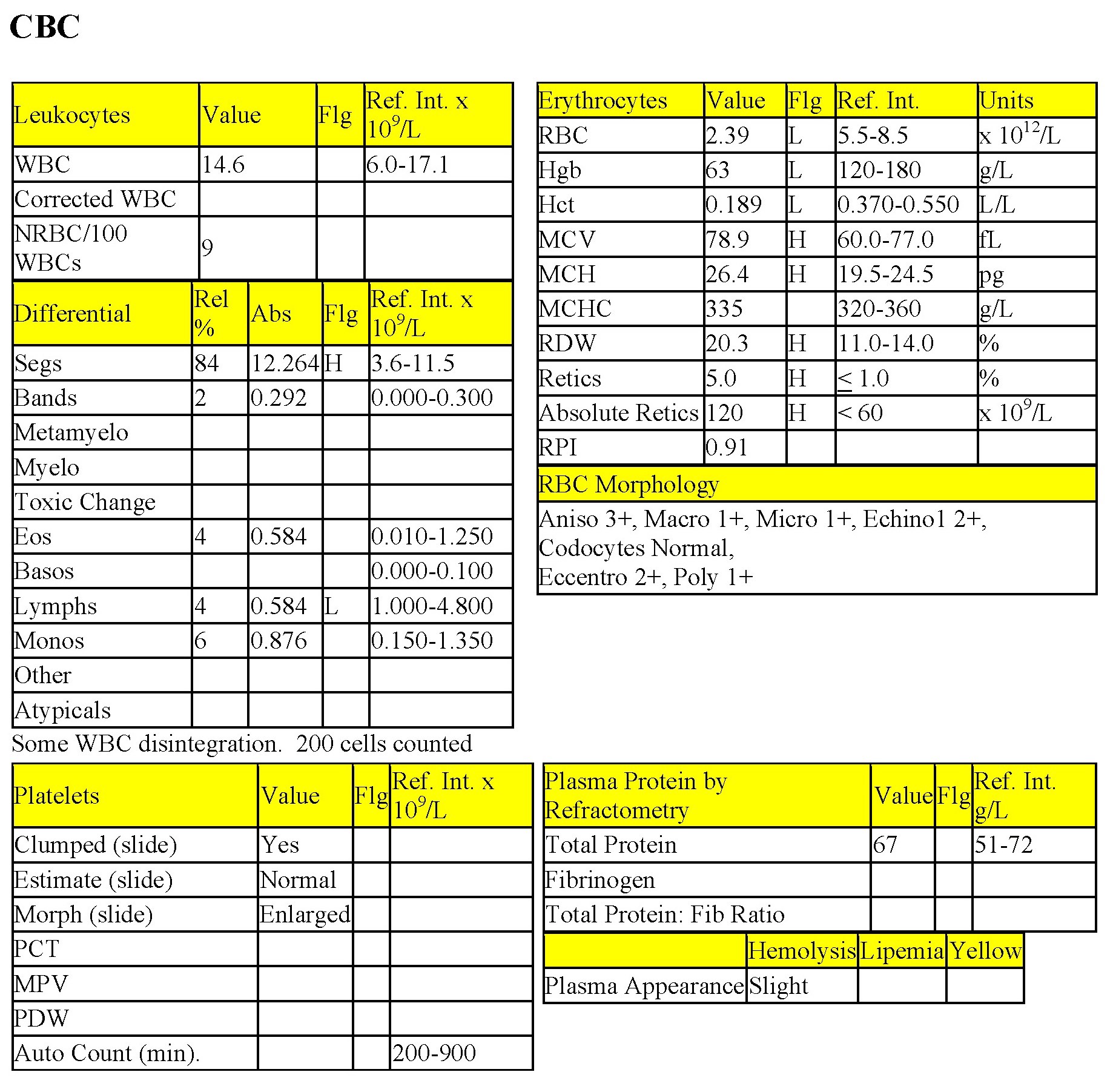
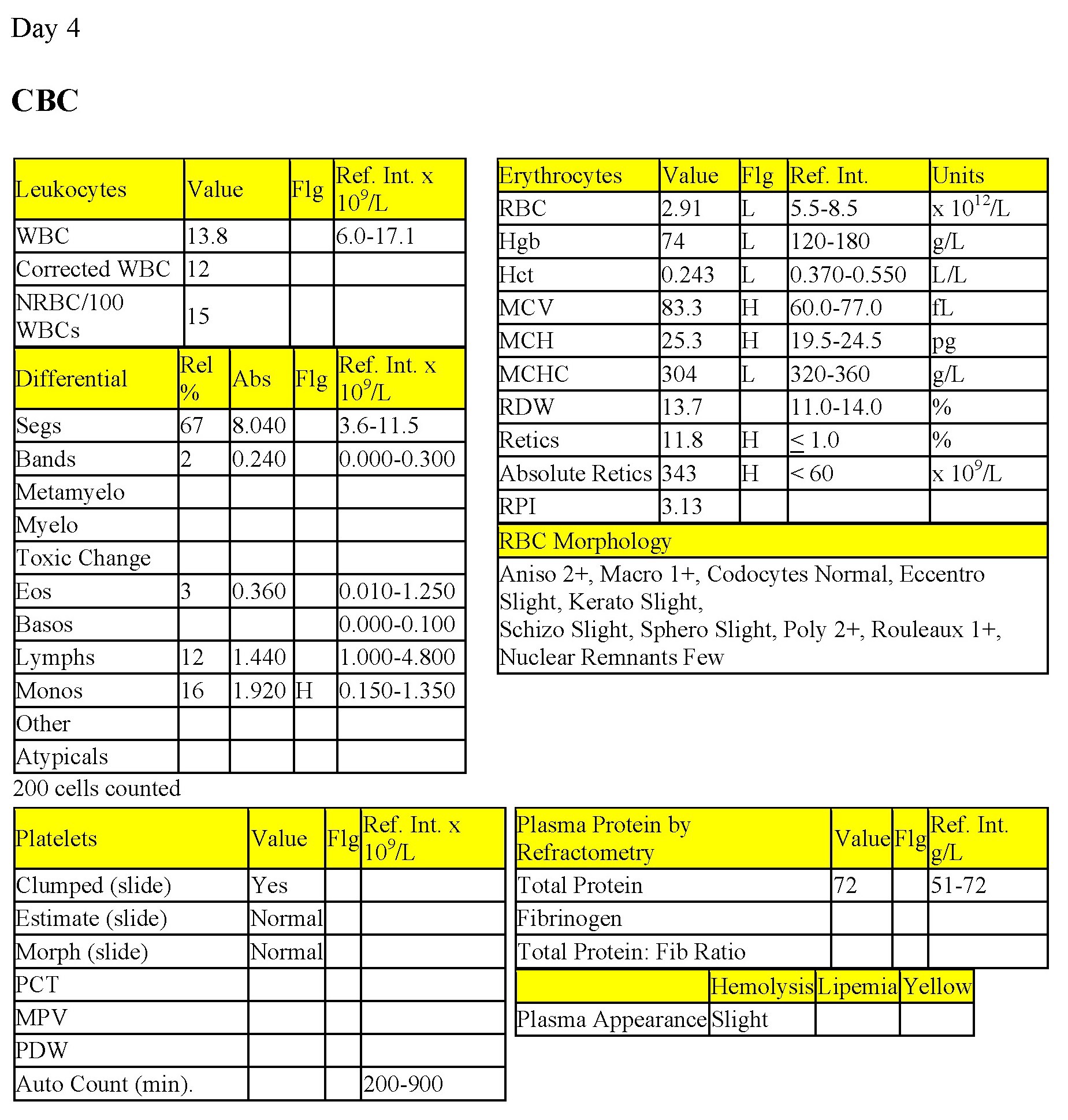
CBC
On day 1, there is a severe anemia with mild to moderate regeneration (increased anisocytosis, macrocytes, polychromasia, mildly increased MCV, and increased reticulocytes [% and absolute count], although the RPI is not increased). In this case the increased anisocytosis correlates with the increased RDW. The presence of eccentrocytes at 2+ is highly significant and indicates oxidative damage to RBC membranes (Fig. 1.15). Intravascular hemolysis and extravascular hemolysis are probably both occurring. Total WBC count is within RI but there is a mild neutrophilia and moderate lymphopenia, consistent with stress. Skippy received fluid therapy and general supportive care. On day 4, the Hct is beginning to recover and the reticulocyte response is more pronounced. The RPI now indicates marked regeneration. The increased MCV relates to the presence of additional large, young RBCs. Eccentrocytes are now only slight. Keratocytes and schizocytes are due to fragmentation of damaged RBCs. There is no longer a stress leukogram, and the mild monocytosis may relate to increased demand for phagocytic cells to remove damaged RBCs and free RBC membranes from the peripheral blood.
- Skippy had eaten sautéed onions that had been scraped off the top of a take-out steak into the garbage. Onions contain an oxidizing agent which can cause lipid peroxidation of the RBC membrane and can also overwhelm the hexose monophosphate shunt resulting in formation of eccentrocytes, Heinz bodies, or both. Skippy recovered fully. Ingestion of zinc-containing foreign bodies, including coins, may represent an even more urgent situation as these generally must be removed surgically in order to halt the hemolysis.
Case 10. Brutus
Brutus, a 12-year-old M(c) Labrador Retriever X dog, had a history of constipation and a distended abdomen.
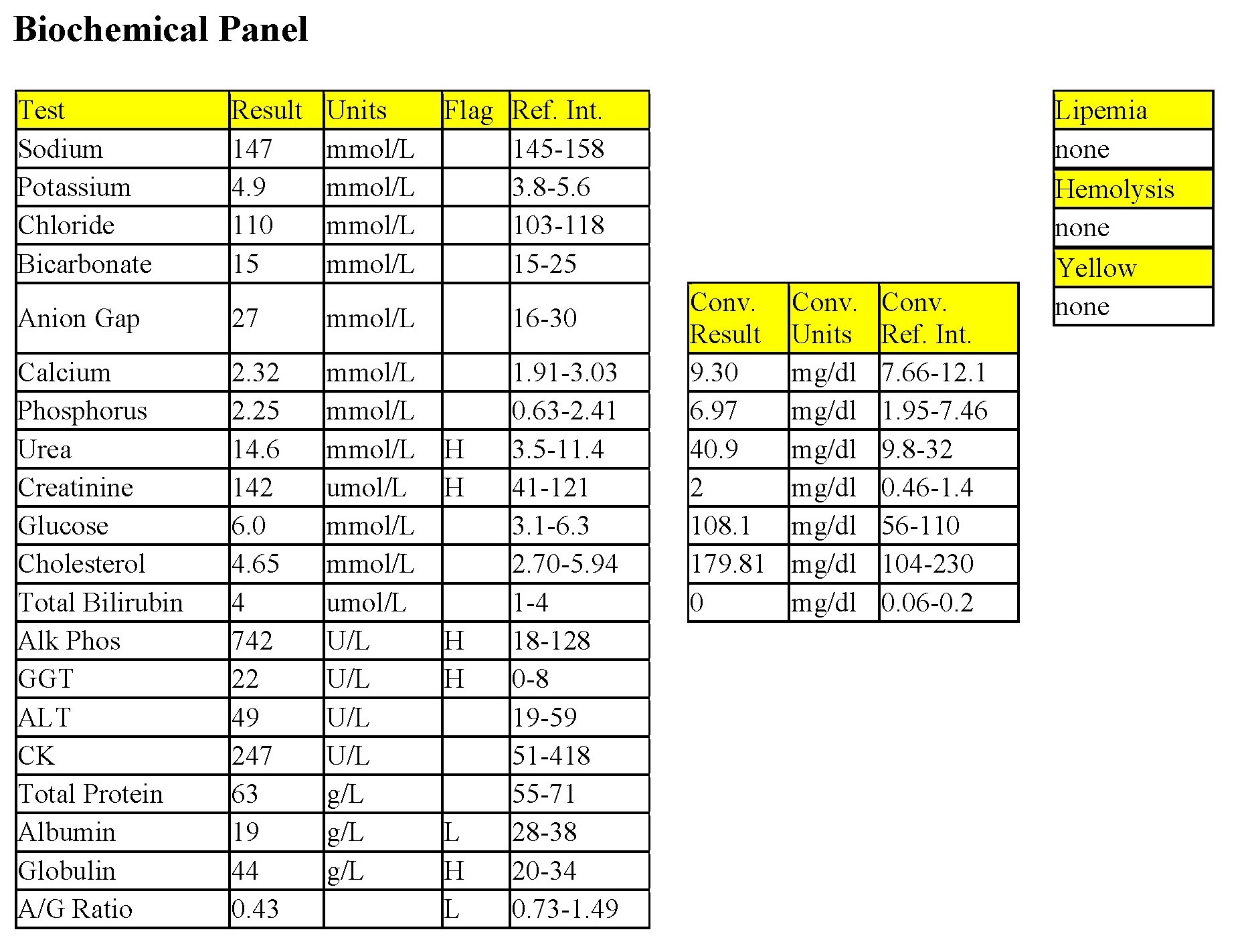
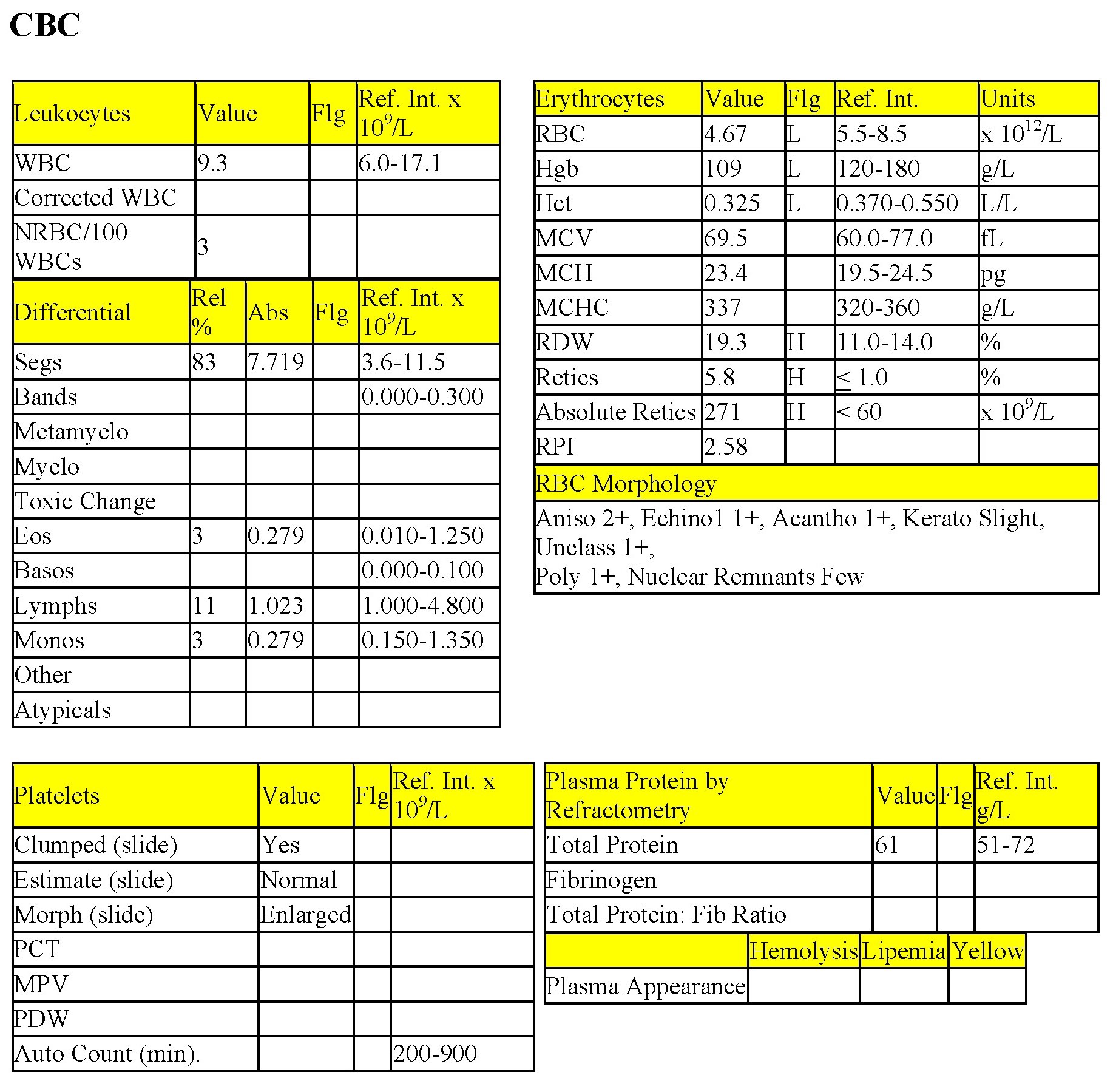
CBC
There is a mild anemia with a mild to moderate regenerative response (increased reticulocyte % and count; increased RPI; polychromasia; nRBCs; and increased anisocytosis and RDW). Acanthocytes noted on smear evaluation can be seen with hemangiosarcoma, high fat diets, hepatic disease, or as an incidental finding (Fig. 1.22). Given the age and breed of dog, clinical signs, and presence of a regenerative anemia, hemangiosarcoma is suspected. The leukogram is unremarkable, although lymphocyte numbers are low normal (approaching a stress lymphopenia). Thrombogram and total protein are unremarkable.
Biochemical Panel
The mild increase in ALP activity could be due to cholestasis or enzyme induction from chronic illness/stress.
- Brutus underwent splenectomy and histopathology of the spleen confirmed the presence of hemangiosarcoma. The mechanism of acanthocyte formation with this tumor is not known; however, the following is proposed: hemangiomas and hemangiosarcomas frequently contain cavernous spaces filled with blood. With cell death, membrane lipids, including cholesterol, are released into the milieu and cholesterol loading of viable RBC membranes may occur. Excess cholesterol renders the RBCs more rigid such that a section(s) of membrane may shear off. The cell then assumes an abnormal shape with several uneven projections and a loss of central pallor since the cell is now smaller and more condensed. In addition to intralesional bleeding, these tumors frequently rupture resulting in bleeding into a body cavity, the peritoneal space in the case of Brutus. Clinical signs depend on volume of blood lost and how rapidly this occurs; hypovolemic shock can develop with acute severe internal hemorrhage. Icterus can also occur as macrophages phagocytose and degrade free red cells and bilirubin is transported to the hepatobiliary system.
Case 11. Tonka
Tonka, a 5-year-old F Labrador Retriever X dog, was lethargic and anorexic for 2 days. She was icteric and had palpable organomegaly in the cranial abdomen.
CBC
Many of the erythrocyte parameters are not available because of agglutination. There is a moderate to severe anemia with moderate regeneration (increased reticulocyte %, macrocytes, and polychromasia). Microcytes and spherocytes are significant and, together with the agglutination and regenerative anemia, signal the presence of immune-mediated hemolytic anemia (Figs 1.9 and 1.11). The mild leukocytosis is characterized by a mild neutrophilia, mild left shift, and moderate monocytosis indicating concurrent inflammation. An inflammatory leukogram is commonly seen with IMHA and may relate to the red cell destruction as well as hypoxic injury to tissues. Accelerated granulopoiesis from cytokine stimulation of marrow precursors may also play a role. Platelets are moderately decreased; a platelet count is not available due to platelet clumping. Immune-mediated thrombocytopenia (IMTP) may accompany IMHA. Presumably, platelets numbers are not sufficiently low (<50 x 109/L) to result in spontaneous bleeding, but without an accurate count, this remains unknown. Disseminated intravascular coagulation and fibrinolysis (DIC&F) is a frequent sequela to immune-mediated hemolysis and could also explain the thrombocytopenia, although there are no keratocytes and schizocytes to support fibrin strand injury to RBCs. The yellow plasma is due to extravascular hemolysis. Total plasma protein is within RI.
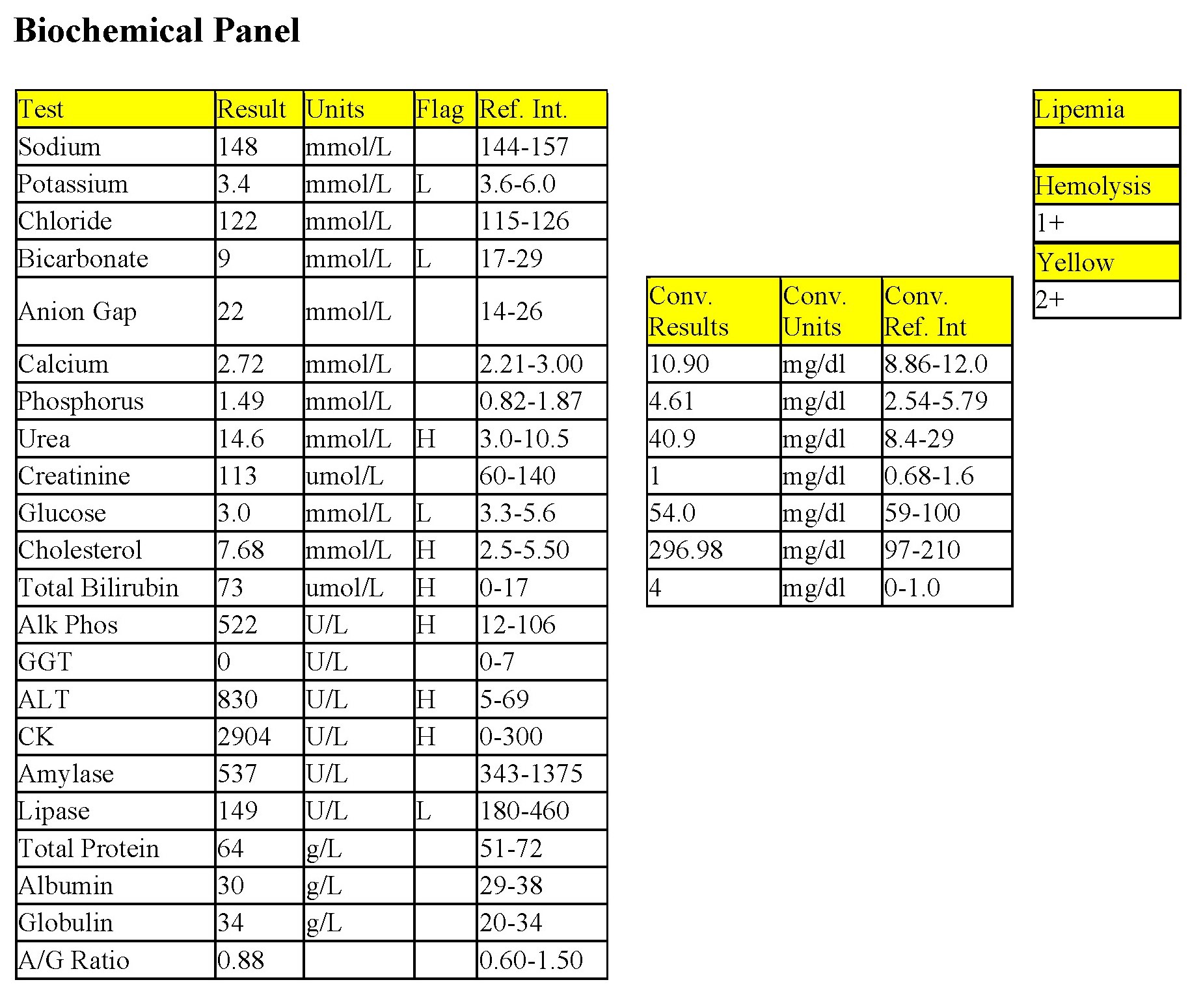
Biochemical Panel
The markedly decreased bicarbonate indicates metabolic acidosis, which is not due to acid gain (anion gap not elevated). Intestinal and/or renal bicarbonate losses would be suspected. Urea elevation could be due to decreased renal perfusion, although creatinine is not also elevated. Intestinal bleeding could also explain the urea elevation without creatinine and phosphorus elevations. Intestinal bleeding could occur with severe thrombocytopenia and/or shock. The mildly decreased glucose is inaccurate, in this case, as there was a delay before separating serum from cells (in vitro glycolysis). Moderate hyperbilirubinemia is due to extravascular hemolysis. Hyperbilirubinemia, mild hypercholesterolemia, and mild to moderate increase in ALP activity indicate cholestasis. The moderately increased ALT activity indicates hepatocellular damage, probably from hypoxia secondary to the acute development of hemolytic anemia. CK activity is mildly increased suggesting myocyte leakage, possibly from poor muscle perfusion or trauma related to restraint/venipuncture.
- Tonka developed red urine, suggesting hemoglobinuria and intravascular hemolysis, and was clinically deteriorating. She was euthanized and a necropsy was not done. IMHA is a common disease in dogs. Immunoglobulin (Ig) G antibody is most often present and in sufficiently high concentrations to cause RBC agglutination. IgM involvement is much less common. Complement may be bound and this accelerates phagocytosis of affected cells, forming spherocytes if only a portion of the membrane is phagocytosed, or totally engulfing RBCs if the macrophage is able and the cell is coated with antibody. Also, complement binding can proceed to assembly of the membrane attack complex which leads to pore formation in RBC membranes and leakage of hemoglobin into the plasma (hemoglobinemia) leaving behind a rim of cell membrane (ghost cell). The prognosis is worse if both intravascular and extravascular hemolysis are occurring. Similarly, the prognosis is worse if the animal is experiencing both IMHA and IMTP, or if the animal develops DIC&F. An inflammatory leukogram is very common with IMHA and can be much more severe than in Tonka’s case. If the anemia is nonregenerative but with hallmarks of IMHA, monitoring the CBC is useful to watch for regeneration. A persistent lack of regeneration occurs with IMHA if the antibody is directed against an RBC precursor. Bone marrow examination may reveal a maturation arrest which signals the erythrocyte stage at which the antibody is directed. The prognosis is often poorer in these situations. A direct antiglobulin test (DAT) or Coombs’ test can be done to detect antibody bound to RBC membranes. False negative results do occur. Flow cytometry to detect RBC-bound antibody appears to be a more sensitive test than DAT. However, if classical signs of IMHA are present on the CBC, additional testing is usually unnecessary. Underlying disease must also be considered. Neoplasia, particularly lymphosarcoma, can first be manifested as IMHA, IMTP, or both. Possible mechanisms involved are a deranged immune system response or RBC-bound tumor antigen which is seen as foreign by the immune system.
Increase in the number of neutrophils in peripheral blood.
Increase in the number of monocytes in peripheral blood.
Process that adds base (HCO3-) to the blood or removes acid (H+); blood pH may or may not be increased.
Difference between unmeasured anion and cation concentrations, calculated using the formula: (Na+ + K+) minus (Cl- + HCO3-.)
Process that adds acid (H+) to the blood or removes base (HCO3-); blood pH may or may not be decreased.
Most abundant plasma protein in health; maintains oncotic pressure.
Impaired bile flow.
The end product of coagulation, produced by the conversion of fibrinogen.
Release of less mature neutrophil stages (bands, metamyelocytes, myelocytes) from the marrow into the peripheral blood in response to inflammation.
Cytoplasmic abnormalities seen in neutrophils that have not matured normally in the bone marrow. Abnormalities include retention of primary granules, vacuolation, darker staining due to retention of ribosomes, and deposits of rough endoplasmic reticulum (Döhle bodies).
All tests on the CBC that evaluate leukocytes. Also, that part of the leukon which is evaluated by examination of a peripheral blood sample (typically does not include leukocyte precursors).
All tests on the complete blood count (CBC) that evaluate platelets. Also, that part of the thrombon which is evaluated by examination of a peripheral blood sample (typically does not include platelet precursors).
Increases serum urea and/or creatinine.
Granulocyte with fine, inconspicuous cytoplasmic granules and a segmented nucleus; important in phagocytosis and killing of bacteria.
Decrease in the number of circulating platelets below the reference interval.
Results in bleeding due to the requirement of vitamin K for normal synthesis of coagulation factors II, VII, IX, X.
Increase in the number of eosinophils in peripheral blood.
Mononuclear, granular leukocyte important in hypersensitivity reactions.
Signs and symptoms that are a consequence of the presence of a neoplasm, but not due to the local presence of cancer cells. An example would be the effects of hypercalcemia of malignancy related to production of PTHrP by neoplastic T lymphocytes.
Growth factor that maintains platelet mass.
Part of hemopoiesis dealing with the production of platelets from stem cells to megakaryocytes to circulating platelets.
Substances which exist in solution as positively and negatively charged ions.
Urine specific gravity between 1.008 and 1.012, reflecting urine that has been neither diluted nor concentrated by the kidneys.
Piece of the nucleus that persists in the mature erythrocyte. May be seen in healthy animals, especially cats, and those with regenerative anemias, or hypofunctioning spleens.
Decrease in the number of neutrophils in peripheral blood below the reference interval for the species.
Defective or abnormal development of any cell line within the bone marrow; may culminate in neoplastic disease.
Type of non-lymphoid bone marrow derived neoplasm in which there are high numbers of blast cells in the bone marrow, cell lineage may not be obvious based on morphology alone, and the clinical course is often rapidly deteriorating following diagnosis.
Enzyme that is released into the peripheral blood following muscle injury.
Nonspecific term for sublethal or lethal injury to hepatocytes due to various causes, e.g. hypoxia, toxins, infection.
Heme protein responsible for oxygen transport in muscle.
Anucleate (in mammalian species), immature erythrocyte containing cytoplasmic RNA and ribosomes which are precipitated by staining with new methylene blue.
Method of measuring the protein content of a fluid that relies on refraction of light, which is proportional to the quantity of solids in solution.
Typical change seen in peripheral blood of an ill or stressed animal (with increased cortisol levels), consisting of lymphopenia which may be accompanied by neutrophilia and monocytosis (species differences exist).
Erythrocyte with little central pallor and several irregular membrane projections.
Part of hemopoiesis dealing with the production of granulocytes from stem cells to mature circulating neutrophils, eosinophils, and basophils.
Thrombocytopenia due to destruction of platelets that is caused by antibodies produced by the animal’s own immune system.
See Secondary hemostasis.
Process in which fibrin is broken down, resulting in clot dissolution.
Disseminated Intravascular Coagulation & Fibrinolysis; simultaneous disorders of coagulation and fibrinolysis due to generalized derangement of hemostasis.
Solid malignant lymphoid tumor.