Neutrophil Response and Bone Marrow Activity
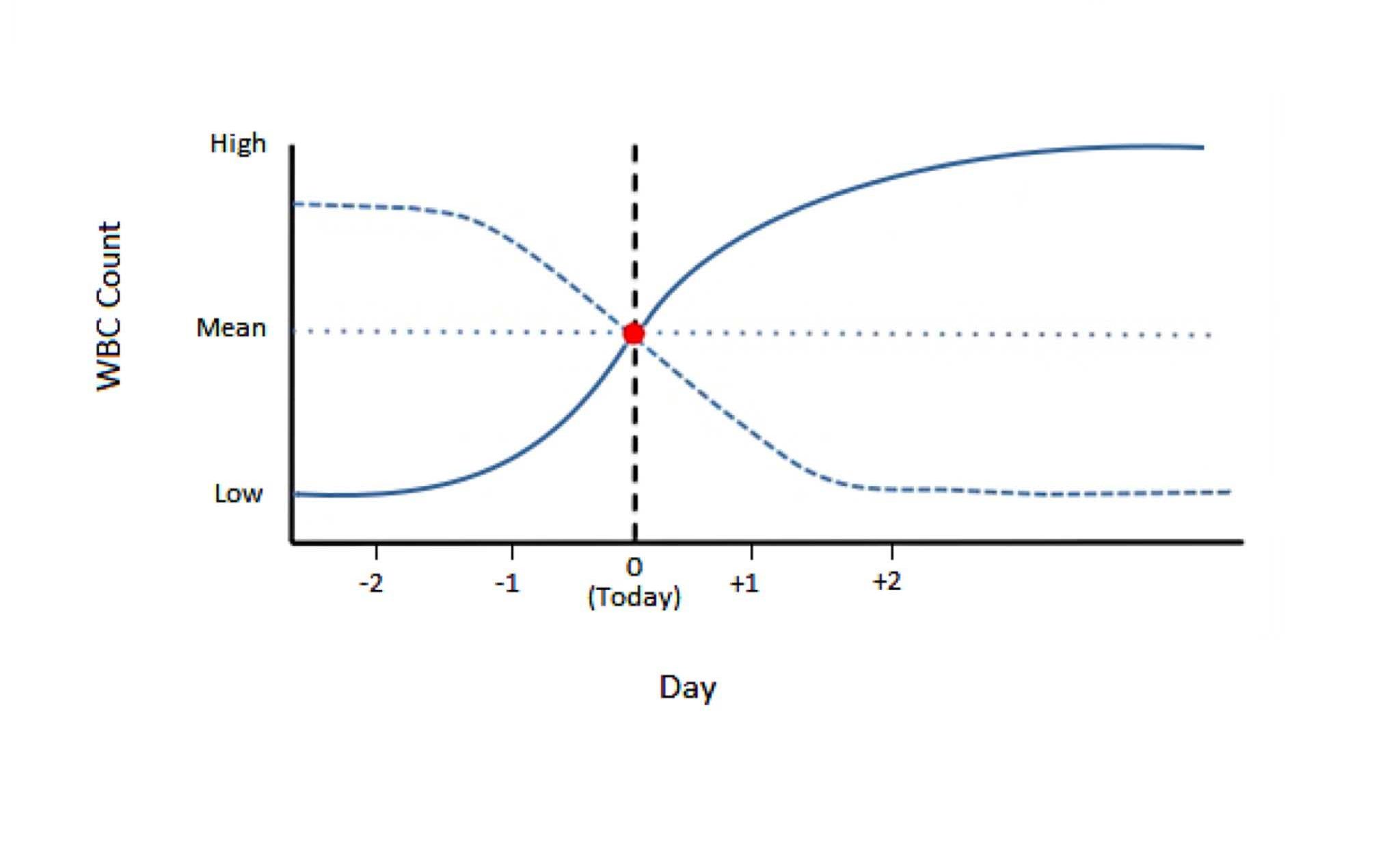
A time frame for the inflammatory process can sometimes be determined by evaluating changes on the CBC, particularly when changes are extreme. Neutropenia (neutrophil absolute numbers below the RI), accompanied by increased numbers of immature neutrophils and toxic change, usually indicates acute severe inflammation. Chronic inflammation is often associated with marked neutrophilia, with or without an increase in bands, and a low grade of toxic change. However, a duration for the inflammation can often not be accurately determined based on the results of a single CBC, particularly for more moderate inflammatory processes which we see most commonly. Anatomic pathologists are well-situated to assess duration of an inflammatory process because the hallmarks and layers of the cellular and tissue response can be visualized relative to the entire lesion by histologic examination. When we sample the peripheral blood, we are assessing a dynamic process at one point in time (Fig. 2.5). The CBC findings enable assessment of the bone marrow’s response to the inflammation. However, monitoring the CBC changes over several days may be necessary to detect trends, predict the outcome, and facilitate patient management.
Neutrophilia is most often associated with significant inflammatory lesions in domestic animals. The duration and severity of the inflammation and the bone marrow response to the inflammation will determine the degree of neutrophilia and whether there is an accompanying left shift. Severe neutrophilia with little or no left shift suggests chronic inflammation and neutrophilic hyperplasia would be expected on bone marrow examination. If the demand for neutrophils is great and persistent, hyperplasia may be present in the marrow without being reflected as neutrophilia in the peripheral blood. For example, pyometra in the dog may result in neutrophil numbers within the RI or mildly increased, but accompanied by a moderate to severe left shift. In this situation, there may be a steady-state established between neutrophil production and egress into the uterus, even though bands are also being released. Therapeutic removal of the uterus eliminates the source of inflammation and a rebound neutrophilia may occur reflecting the degree of neutrophilic hyperplasia present in the bone marrow. Several days may be required before the peripheral blood leukocyte profile returns to normal. Leukogram changes associated with pyometra are variable, although all would be expected to reflect significant inflammation. Factors that can influence the laboratory findings include, but are not restricted to: the duration of the condition; the point at which the patient is presented for medical care; whether there are secondary complications (e.g. anemia of inflammatory disease, endotoxemia affecting renal tubular function, hyperglobulinemia affecting glomerular filtration); and whether spontaneous drainage from the uterus is occurring.
Persistent neutrophilia should be thoroughly investigated to rule out foci of chronic inflammation, abscesses, necrosis, or neoplasia. Sites of inflammation which can be difficult to identify without additional tests are joints (polyarthritis), central nervous system (meningitis), cardiovascular system (endocarditis), and intestinal tract (associated with ulcers).
Neutrophilia associated with neoplasia includes primary neutrophilic leukemia (sometimes called granulocytic or myelogenous) and secondary neutrophilia due to elaboration of cytokines by tumors of various origins. Neutrophilia may also accompany neoplasms, such as hemangiosarcoma of the spleen, that contain areas of significant necrosis, in an effort to assist in ridding the body of damaged cells and necrotic debris.
Decrease in the number of neutrophils in peripheral blood below the reference interval for the species.
Release of less mature neutrophil stages (bands, metamyelocytes, myelocytes) from the marrow into the peripheral blood in response to inflammation.
Decrease in hematocrit (PCV) recognized on the complete blood count (CBC); usually hemoglobin concentration and RBC numbers are also decreased.
Of myeloid origin.

