Hypercalcemia
Hypercalcemia must be evaluated in relation to hydration status, serum protein and albumin concentrations, and patient age. If ECF volume contraction, hyperproteinemia and/or hyperalbuminemia are ruled out as causes of increased total calcium, and if age is not considered a factor (mild hypercalcemia may be present in young growing animals, particularly dogs), then hypercalcemia should always be investigated by first rechecking the total serum calcium to determine if the finding is persistent and not a sampling or laboratory error. Following this, if a true hypercalcemia is suspected, measurement of free calcium is recommended to determine if the biologically active form of calcium is elevated. Elevated free calcium is often associated with polyuria due to its antagonism of ADH at the level of the renal tubules. Soft tissue mineralization may occur when the product of total calcium x phosphorus, exceeds 6 mmol/L (70 mg/dL). Short-term hypercalcemia may lead to muscle dysfunction and cardiac arrhythmias, whereas long-term hypercalcemia may lead to nephropathy from calcium deposition in renal tubules.
Primary hyperparathyroidism
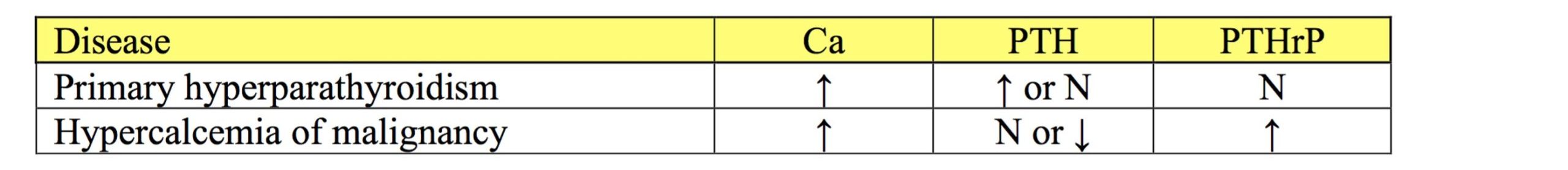
Primary hyperparathyroidism is an unusual cause of hypercalcemia in domestic animals. However, functional parathyroid tumors are associated with excess PTH release resulting in hypercalcemia, mainly due to calcium resorption from bone, and hypophosphatemia, due to the potent phosphaturic action of PTH. The diagnosis is made based on hypercalcemia and high normal to increased PTH concentration. See Table 10.2 below.
Hypercalcemia of malignancy
Hypercalcemia of malignancy is the most important cause of persistently increased free calcium concentration in the dog. Several neoplasms, most importantly T cell lymphosarcoma, have been associated with increased production of a parathyroid hormone-related protein (PTHrP). Although several normal cells produce PTHrP, increased serum concentrations are generally due to production by neoplastic cells. In addition to lymphosarcoma, apocrine gland adenocarcinoma of the anal sac (in dogs), mammary adenocarcinoma, squamous cell carcinoma, and malignant melanoma (in dogs), and others, may produce PTHrP. Serum PTHrP is increased and serum PTH is normal to decreased in the face of hypercalcemia and variable serum phosphorus, depending on the balance between the phosphaturic action of PTHrP and GFR. See Table 10.2.
Neoplasms that do not produce PTHrP can also be associated with hypercalcemia. Certain tumors may produce osteoclast activating factor, prostaglandins, or vitamin D-like steroids which increase serum calcium by promoting bone resorption. Malignant plasma cell tumors may produce bone lysis by elaborating osteoclast activating factor. Lameness is sometimes the first clinical sign noted by owners of animals with this tumor. Other tumors which have metastasized to bone can also cause osteolysis and hypercalcemia.
Hypoadrenocorticism
Hypercalcemia is seen in about 30% of dogs with hypoadrenocorticism. The pathophysiology of the increased serum calcium is not clear but appears to relate to decreased renal excretion of calcium. Cortisol normally promotes renal calcium excretion and this hormone is decreased in dogs with hypoadrenocorticism. Treatment with cortisone rapidly corrects the hypercalcemia by promoting renal calcium excretion.
Idiopathic
Occasionally hypercalcemia and increased free calcium are found in cats for no apparent reason. This condition has been called idiopathic hypercalcemia of cats and is a diagnosis of exclusion.
Hypervitaminosis D
Hypervitaminosis D results in hypercalcemia and hyperphosphatemia. Vitamin D toxicity can occur from increased dietary intake due to excessive supplementation or feed errors; ingestion of medications, rodenticides, or plants containing vitamin D or its precursors; neoplasms or granulomatous lesions which produce vitamin D-like hormones or stimulate vitamin D synthesis. In the case of granulomatous disease, particularly blastomycosis, increased vitamin D synthesis is thought to result from intensified macrophage activity.
Renal disease
Hypercalcemia occasionally occurs with renal disease, particularly in horses and in young dogs with congenital renal diseases. Horses and young dogs have higher serum calcium concentrations than other domestic species and adults, respectively. Metabolic acidosis can accompany renal disease and may explain some instances of hypercalcemia seen with renal failure. Otherwise, serum calcium is variable in acute and chronic renal failure and can be below, within, or above the RI.
With chronic renal failure, mobilization of calcium from bone usually occurs. The failing kidneys have reduced ability to excrete phosphorus which causes vitamin D activation to be suppressed. Synthesis of vitamin D is also compromised by the loss of proximal renal tubular epithelial cells which normally produce this hormone. A secondary consequence of reduced vitamin D activity is decreased serum calcium which triggers increased PTH secretion. PTH causes calcium and phosphorus to be resorbed from bone. Therefore, serum phosphorus continues to rise while calcium may be maintained within the RI. The net effect of renal secondary hyperparathyroidism is osteodystrophy and a condition commonly called rubber jaw.
Unusual cause of hypercalcemia due to increased PTH release from a functional parathyroid tumor.
Increase in free calcium that may accompany certain neoplasms, often due to tumor cell production of parathyroid hormone-related protein (PTHrP)
Solid malignant lymphoid tumor.
Parathyroid hormone-related protein; may be produced by certain neoplasms and result in hypercalcemia.
Malignant neoplasm of epithelial origin, e.g. squamous cell carcinoma.
Terminally differentiated B lymphocyte that secretes specific antibody.
Also called Addison’s disease; endocrine disease of dogs associated with decreased production of mineralocorticoids, glucocorticoids, or both due to adrenocortical pathology.
Of unknown cause.
Mononuclear phagocyte found in tissues that develops from circulating blood monocytes and fulfills many roles in normal immune function including antigen presentation.
Constellation of: retention of metabolic waste products, acid-base and electrolyte disturbances, and compromised urine concentrating ability that develops when the functional mass of the kidneys is reduced by 70% or more; may be acute or chronic.
Referring to cells of the skin and adnexa, lining of the airways, intestines, and urinary tract, renal tubules, liver, and glandular tissues.

