Other Body Fluids
Synovial Fluid
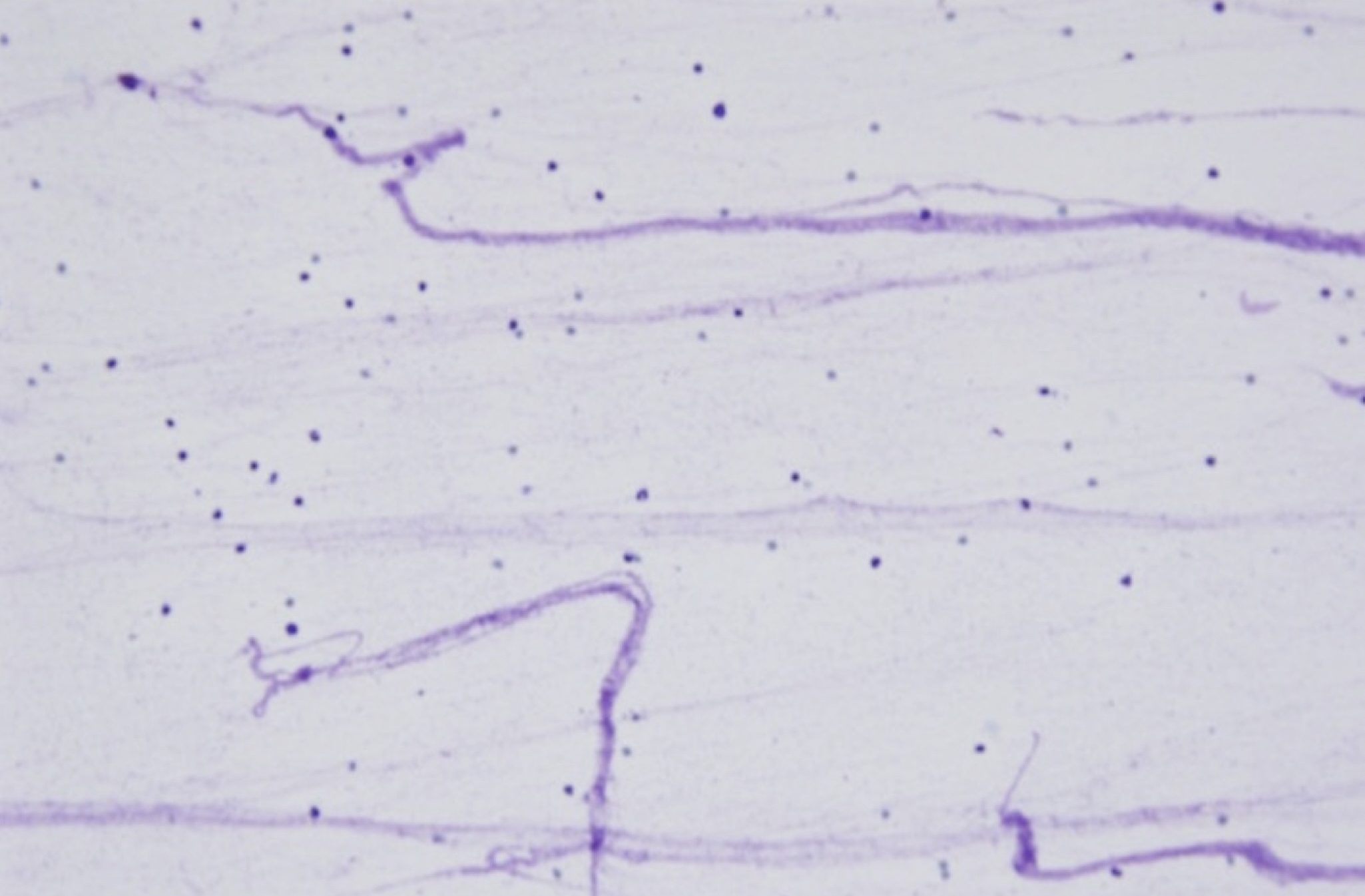
Synovial fluid is often obtained to assess lameness, joint swelling, pain, and occasionally, fever or leukocytosis of unknown origin. Normal synovial fluid is highly viscous due to the presence of hyaluronic acid, which produces a lacy pink stippled background that should not be mistaken for bacteria (Fig. 5.44). Although viscous, normal synovial fluid is clear and often straw coloured. Nucleated cell numbers are generally low (published reference intervals vary from <0.5 x 109/L to <3.0 x 109/L) and most are synoviocytes, mononuclear cells which line the synovial cavity. Protein concentration is also low (usually <25 g/L, but published reference intervals vary). The quantity of synovial fluid that is obtained varies with the joint, the size of the animal, and whether pathology is present. Often there is only sufficient fluid obtained to make direct smears, however, if about 500 µL or more is obtained, cell counts and protein determination can be done on fluid submitted in an EDTA tube and cytospin preparations may be possible.
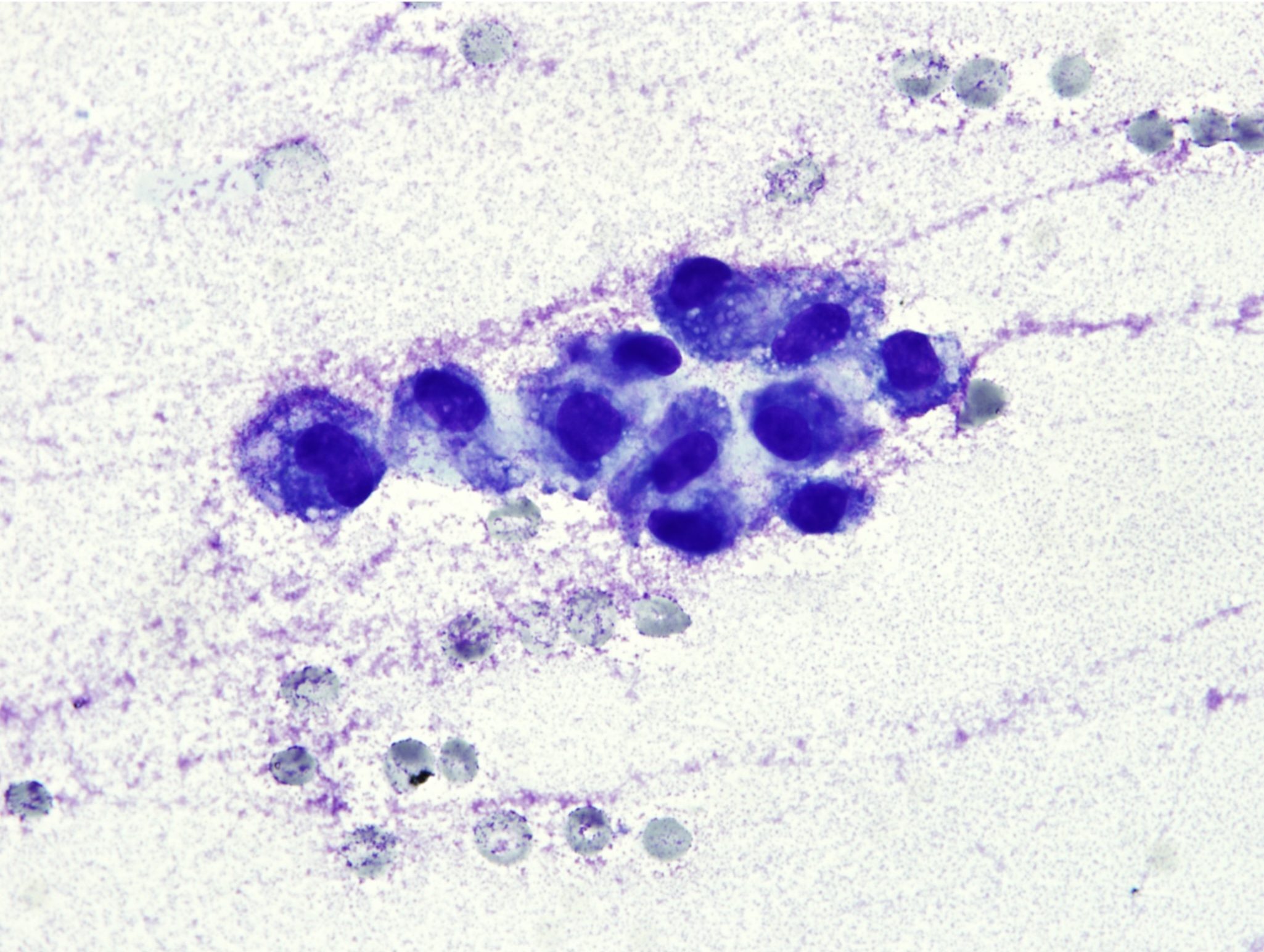
Mild changes in synovial fluid are seen in animals with degenerative joint disease (e.g. osteoarthritis secondary to a variety of conditions including joint instability, trauma, and osteochondrosis). Mildly increased numbers of mononuclear cells, often displaying vacuolated cytoplasm, are the most common finding (Fig. 5.45). Occasionally, osteoclasts may be seen if damage to articular cartilage is severe.
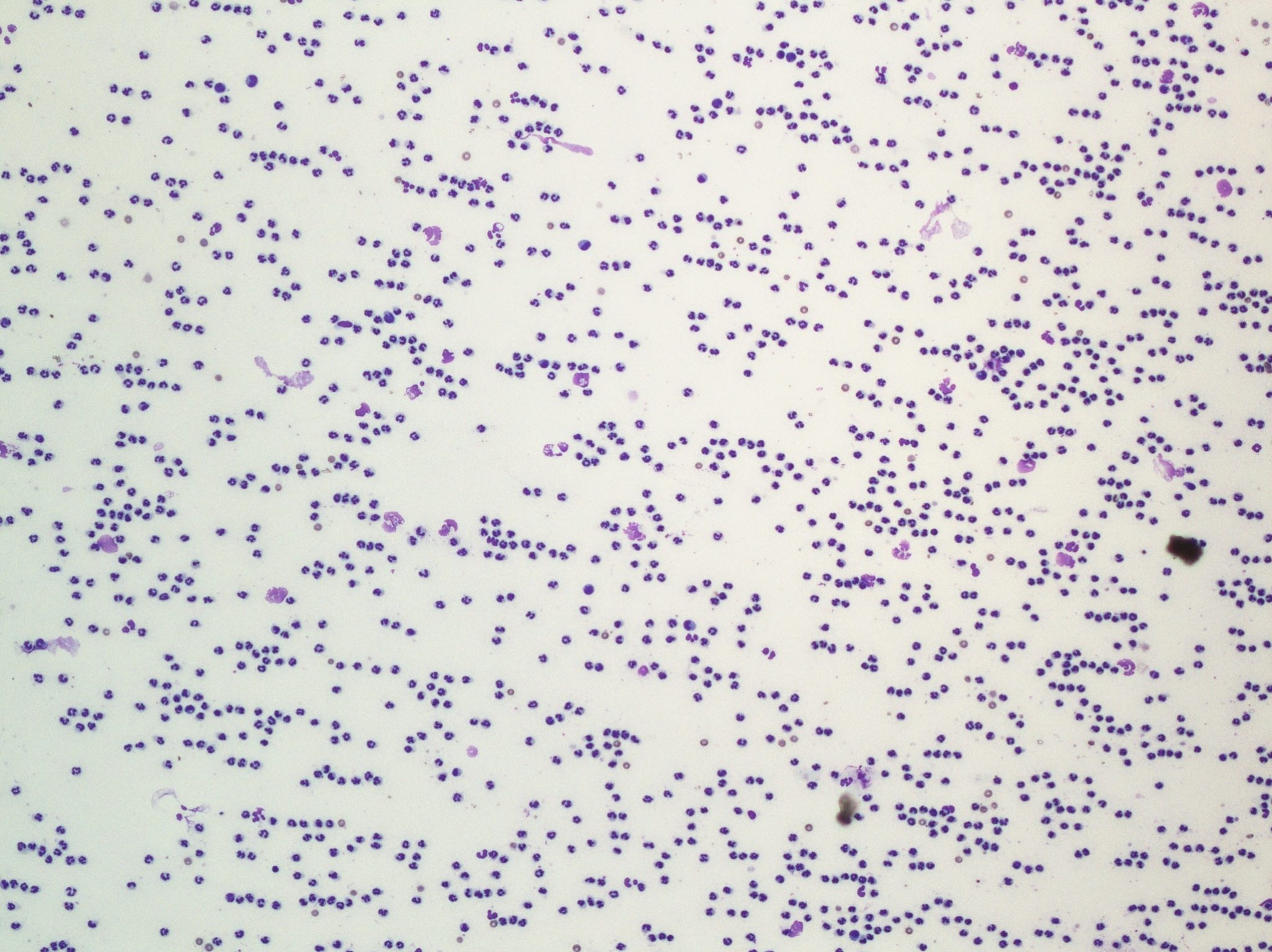
Gross turbidity or opacity of synovial fluid indicates the addition of cells, fibrin, or both, and viscosity is reduced with inflammatory processes. Increases in neutrophils are seen with septic arthritis as well as immune-mediated arthritis, and the two conditions can be difficult to differentiate. Although bacteria and degenerate neutrophils can be seen with perforating wounds into joints, these changes are not commonly seen with systemic infections leading to septic arthritis. The reason is not known, but it is possible that the organisms are sequestered in the synovial membrane and are not free in the synovial fluid. This may also result in negative culture results from synovial fluid. History, species, and additional findings may help to distinguish septic and nonseptic arthritis. Idiopathic, immune-mediated polyarthritis is mainly seen in dogs and is characterized by very high numbers of nondegenerate neutrophils and decreased viscosity involving several joints, often with a waxing and waning course of lameness, fever, and inflammatory leukogram (Fig. 5.46).
Cerebrospinal Fluid
Cerebrospinal fluid is (CSF) clear and colorless, with a very low protein concentration (<0.25 g/L for most species) and nucleated cell count (<5 x 106/L) (see Protocol Manual). Most cells are mononuclear, presumably monocytes and small lymphocytes, though it is sometimes difficult to distinguish between the two. Abnormal samples can also be clear and colourless as turbidity is not noted until nucleated cell numbers are >500 x 106/L. Nucleated cell numbers are not always greatly elevated when pathology is present, therefore, cytologic examination to determine the cell types is very important. CSF samples must be processed immediately because nucleated cells disintegrate very rapidly in the low protein fluid once removed from the body. Even when pathology is present, the nucleated cell count and protein concentration are generally too low to be measured using an automated instrument and spectrophotometer, respectively.
Bright red discoloration could be due to iatrogenic blood contamination or very recent hemorrhage. Careful observation during sample collection may help differentiate between the two. A sample that is clear initially and then becomes red during collection has probably been contaminated with peripheral blood. Dull red or yellow (xanthochromic) discoloration indicates old hemorrhage. An elevation in protein concentration is significant but nonspecific. With meningitis and encephalitis, neutrophils and sometimes macrophages are increased. Parasitic inflammatory diseases may be associated with a predominance of eosinophils. Noninflammatory conditions, such as neoplasia and degenerative diseases, may be associated with increased numbers of mononuclear cells. Neoplasms only rarely exfoliate into the fluid. Significant central nervous system disease can exist in the absence of changes in the CSF, and even when CSF is abnormal there are often many possible differential diagnoses.
Urine
Microscopic evaluation of the urine sediment can provide valuable information about the urinary and sometimes genital tracts. See Urinalysis section of Chapter 7: Renal System.
Mononuclear cell lining the synovial cavity that may be seen on smears of joint fluid.

