Case Studies
Case 1. Jolene
Jolene, a 13-year-old F(s) Maltese dog was presented for periodic gagging and abdominal distention interpreted as ascites on physical examination.
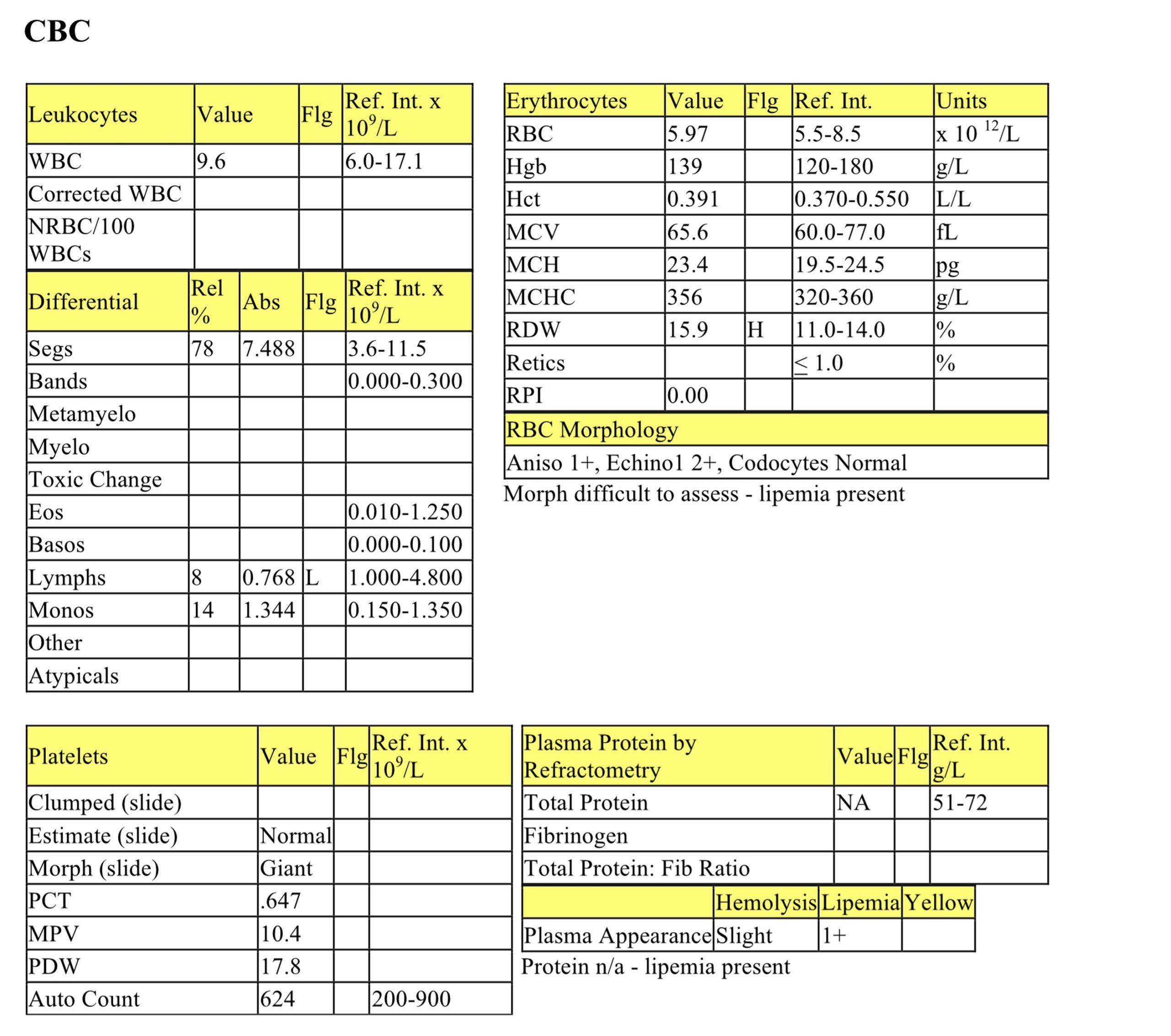
CBC
The erythrogram is unremarkable; lipemia has affected assessment of erythrocyte morphology. Mild lymphopenia is consistent with stress/cortisol influence.
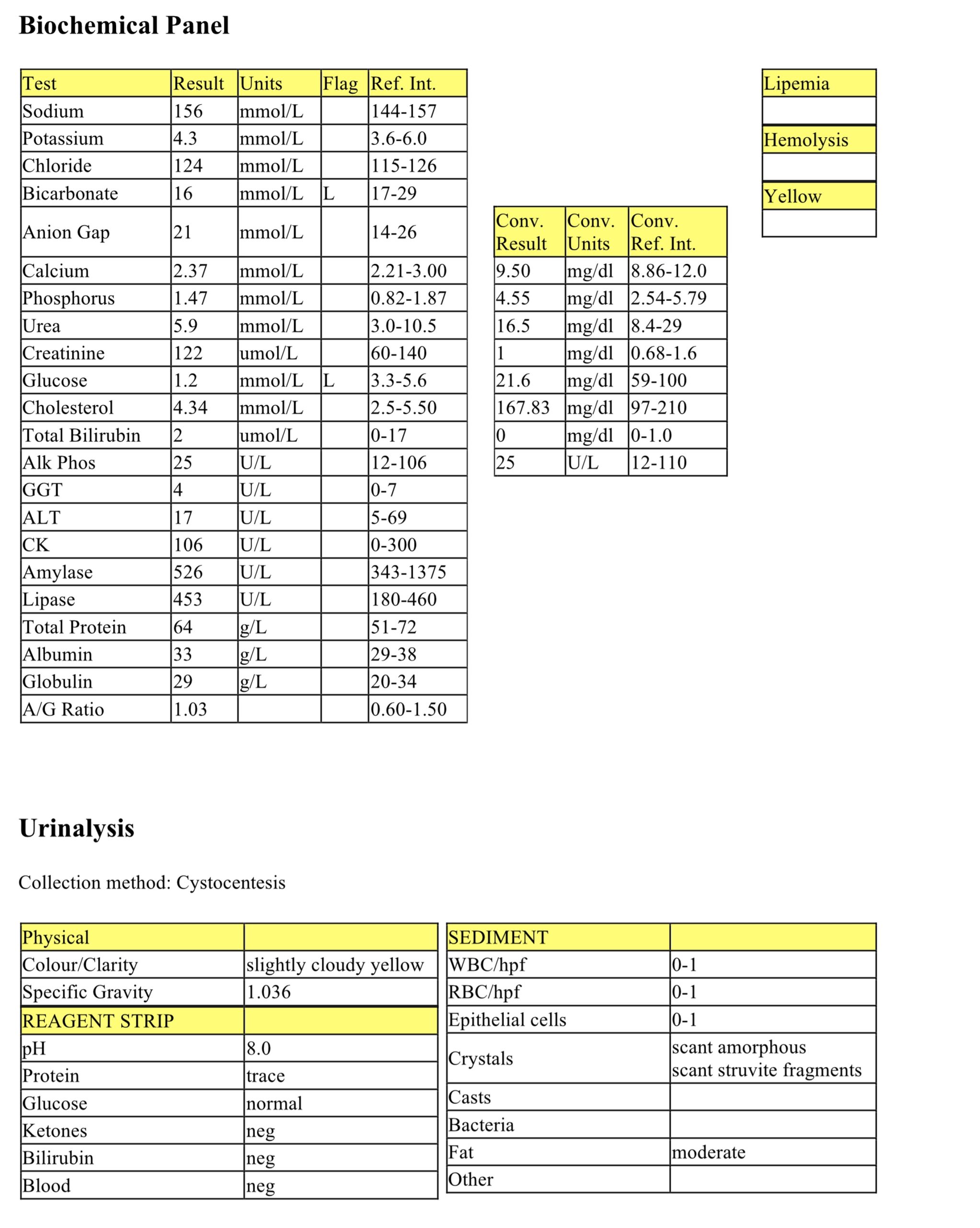
Biochemical Panel
Mild hypochloremia that is not accompanied by hyponatremia could be due to vomiting (HCl loss) although this is not indicated by the history and the acid-base status is normal. Mild creatinine concentration elevation and high normal urea concentration should be interpreted in relation to hydration status and USG (urine not submitted). Mild hyperglycemia could be postprandial sampling or stress-related. Moderate hypercholesterolemia can be associated with many endocrinopathies, abnormal lipid metabolism, cholestasis, hepatic disease, pancreatitis, and protein-losing nephropathy; in this case, HAC is the most likely cause. Postprandial sampling could not explain a cholesterol of this magnitude. Marked elevations in ALP and GGT activities and moderate elevation in ALT activity could be due to primary hepatobiliary pathology or enzyme induction and hepatopathy from high concentrations of endogenous or exogenous steroids (no history of exogenous steroid administration). Lipase activity is mildly increased. However, there is no other clinical or laboratory evidence of pancreatitis and this change may not be significant, but monitoring is recommended. Mild hyperproteinemia with high normal albumin, mildly increased globulins and normal A/G ratio suggests mild dehydration.
Abdominal Fluid
The fluid is unusual in appearance, protein content (by refractometry) and nucleated cell count. Smear examination revealed an acellular preparation with amorphous deposits of mucus. Aspiration of bile from the gall bladder was suspected. Bilirubin measured on the fluid was 344 umol/L and protein content (measured spectrophotometrically) was 1.36 g/L, consistent with bile.
HAC was a suspected cause of the laboratory findings (cortisol related lymphopenia, elevated activities of hepatic enzymes, and hypercholesterolemia). Ascites was probably suspected, in retrospect, because of the pendulous abdomen and enlarged liver.
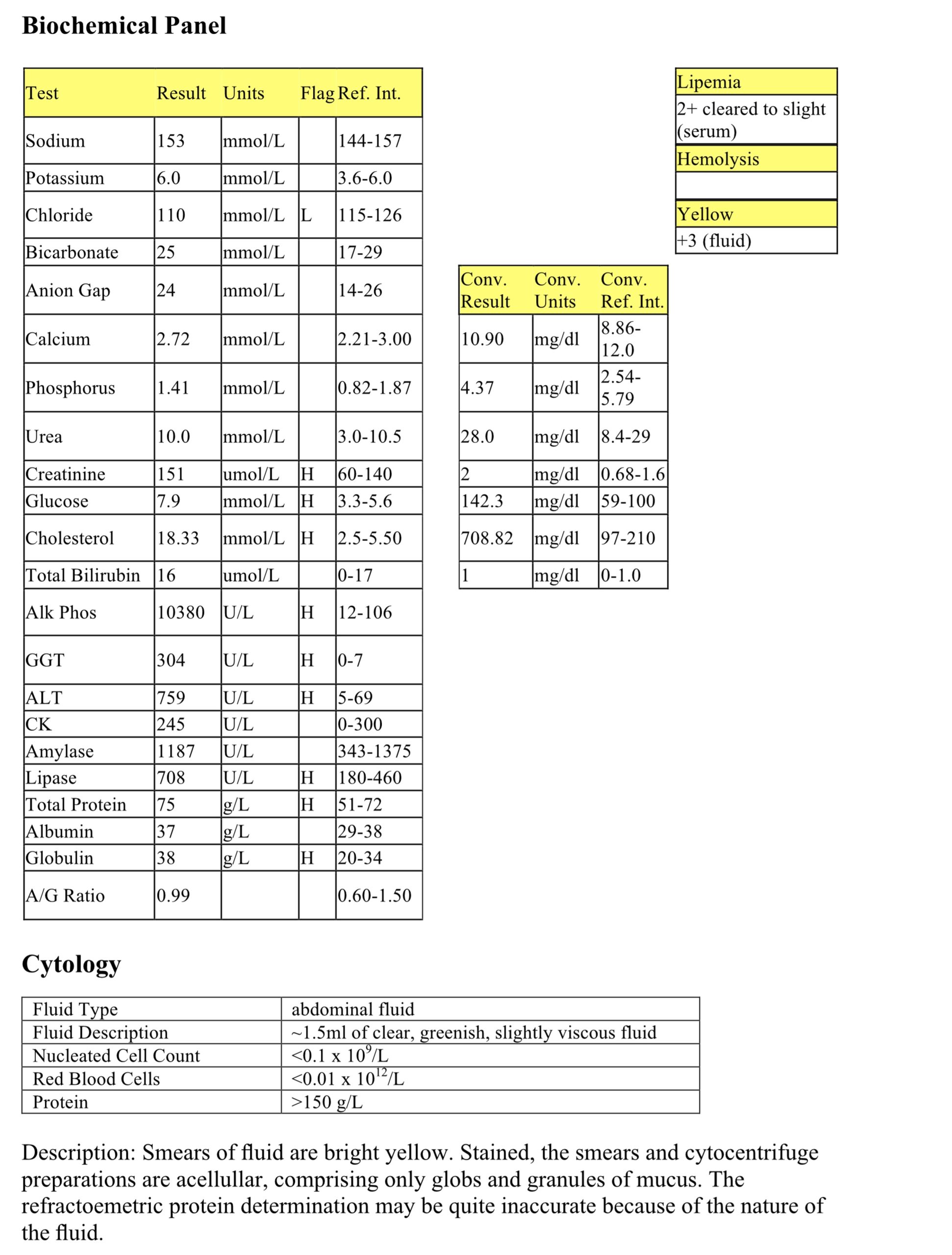
Low Dose Dexamethasone Suppression Test
No suppression of cortisol 8 hours after administration of a low dose of dexamethasone supports the diagnosis of HAC. The absence of suppression (defined as a decrease to <50% of baseline cortisol at either 3 or 8 hours, or 3 hour concentration >40 nmol/L) precludes differentiation of PDH from an AT because 25% of PDH cases and all adrenal tumors will not demonstrate suppression. The HDDST shows no suppression of cortisol at 8 hours post dexamethasone administration, however since a 3 or 4 hour sample was not obtained, suppression may have been missed. As a result, the HDDST does not allow for distinguishing PDH from an adrenal tumor. Imaging may have been useful to further evaluate the adrenal glands for the presence of an adrenal mass or bilaterally enlarged adrenal glands that may occur in cases of PDH, but was not done.
- Mitotane was administered to destroy the adrenal cortices. However, treatment was not effective, possibly due to the presence of adrenal neoplasia which is often not responsive to medical therapy. Some of the laboratory abnormalities and clinical signs that we don’t normally associate with HAC could relate to the presence of adrenal neoplasia.
Case 2. Spock
Spock, a 6-year-old M(c) Border Collie dog, had a history of ataxia for a few days prior to presentation and seizure activity on the evening of presentation.
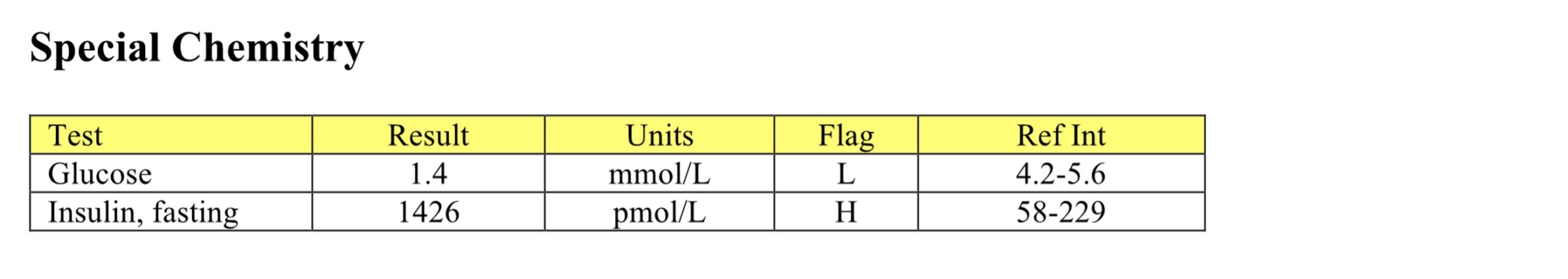
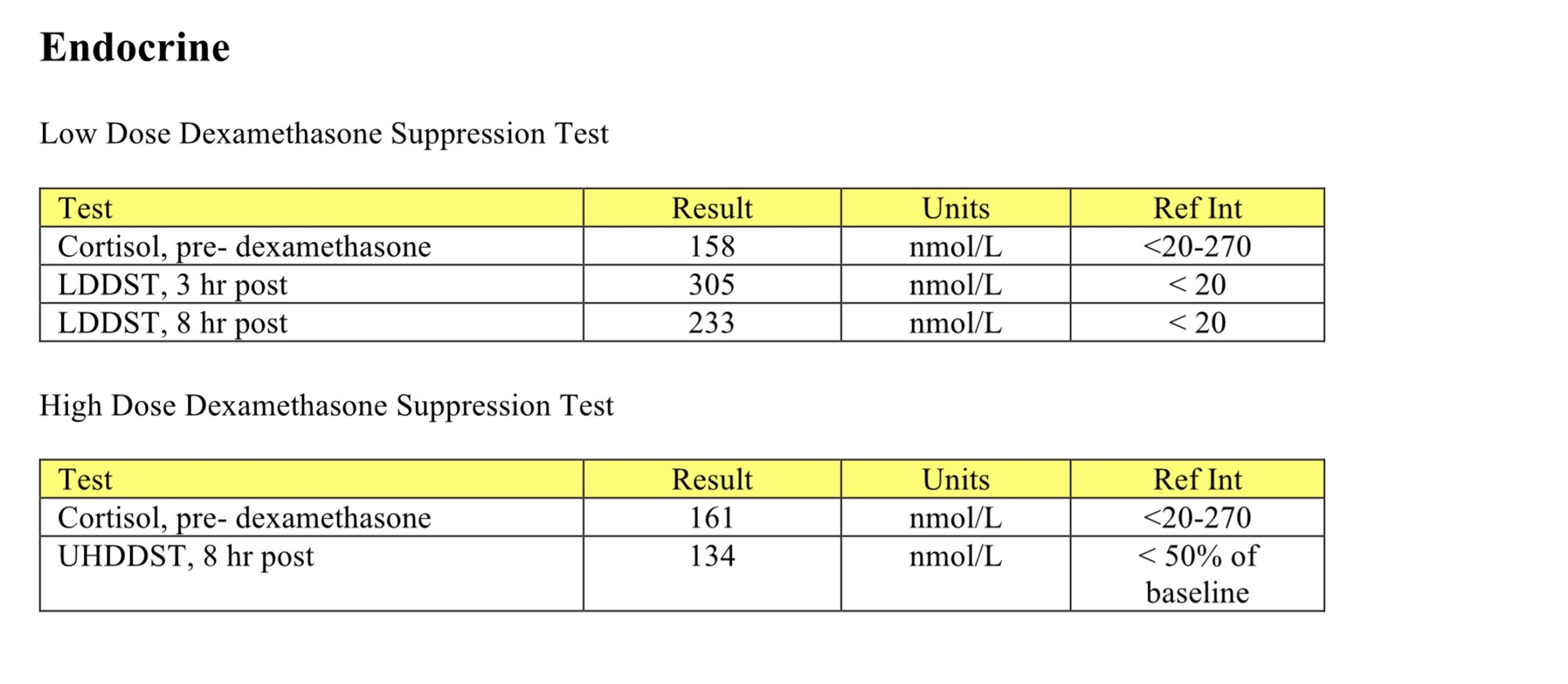
CBC
The erythrogram is generally unremarkable. The mildly elevated RDW does not correlate with an increase in anisocytosis and is unlikely to be significant. The leukogram indicates mild leukocytosis characterized by mild neutrophilia and mild lymphopenia and can be entirely explained by stress. Although the automatic platelet count is below the RI, there is platelet clumping present and the numbers on the smear are estimated as normal.
Biochemical Panel
Very mildly decreased bicarbonate and normal anion gap suggest bicarbonate loss, either through the intestinal tract or kidneys. Severe hypoglycemia, in isolation and in a mature dog, suggests inappropriate insulin secretion. Hypoglycemia may be seen in some dogs with atypical hypoadrenocorticism, however the leukogram changes do not support glucocorticoid lack.
Urinalysis
Urinalysis is unremarkable; urine is concentrated. The trace protein is unlikely significant in this concentrated sample, however should be monitored for persistence.
Glucose and Insulin
Fasting insulin is markedly increased in the presence of hypoglycemia, supporting the diagnosis of an insulin-secreting tumor. Note that the RI for glucose differs from the biochemical panel because the glucose was measured by the referral laboratory that measured the insulin concentration (a send-out test). It is important to always use the RI provided by the laboratory performing the test.
- Seizure activity could not be controlled despite administration of glucose-containing fluids and anticonvulsants. Spock was euthanized and submitted for necropsy. A single 1.5 cm diameter pancreatic nodule was immunohistochemically confirmed to be a β-cell tumor. Although metastases were not found, these neoplasms are usually malignant. Metastatic masses can be very small and difficult to identify on gross examination.
Case 3. Gavino
Gavino, a 12.5-year-old M(c) Arabian horse, had a history of weight loss despite good appetite, polyuria, and polydipsia. Physical examination revealed a long hair coat, low muscle mass, and excessive sweating.
CBC
Mild anemia cannot be further characterized, given the species, but may be due to underlying illness. There is a mild neutrophilia and lymphopenia consistent with a stress leukogram; concurrent inflammation is also possible since fibrinogen is high normal. Interference with the refractometric protein determination is likely, given the lack of protein elevation on the biochemical panel.
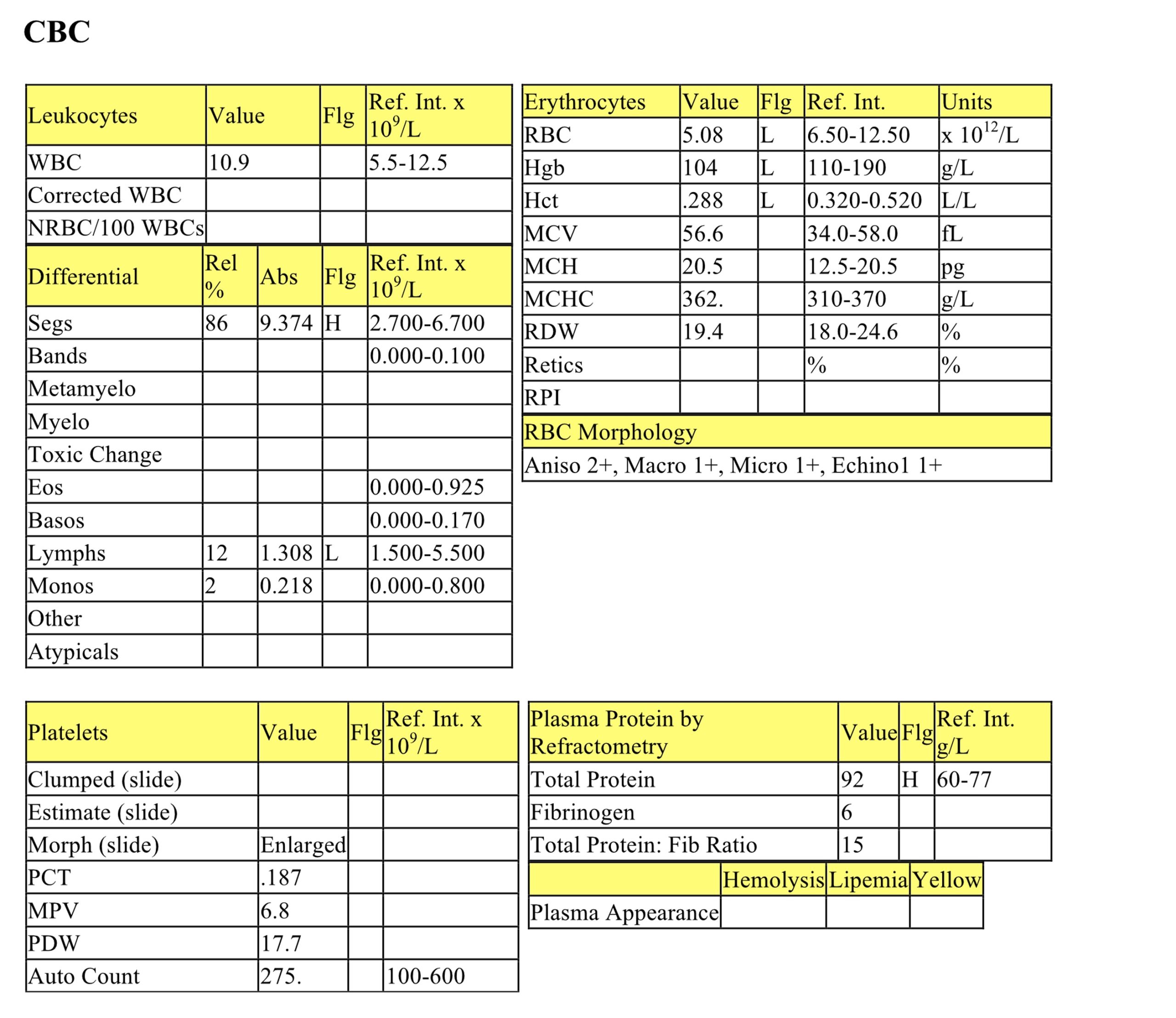
Biochemical Panel
Mild hyponatremia and hypochloremia that are nearly proportional are probably due to osmotic diuresis from hyperglycemia (if chronic), perhaps coupled with movement of water from the intracellular to intravascular space due to hyperglycemia. Mild decreases in calcium and phosphorus may relate to reduced dietary intake. Moderately low creatinine suggests reduced muscle mass. Moderate hyperglycemia is due to insulin resistance from increased cortisol and is the most consistent serum biochemical finding in horses with PPID. Mild to marked increases in activities of all hepatic enzymes suggest hepatobiliary pathology. Elevated AST activity is likely hepatic source not muscle, given the lack of increased CK activity. Insulin resistance can lead to a fatty liver. Increased hepatic enzyme activities in this horse also may be related to glucocorticoid hepatopathy.
Urinalysis
The urine is not concentrated which supports the history of polyuria and polydipsia. Marked glucosuria reflects hyperglycemia. Ketones at 1+ indicate a negative energy balance in this horse and utilization of fat stores rather than carbohydrate for energy.
Given the clinical signs, species, and laboratory findings, PPID was suspected and dexamethasone suppression test recommended.
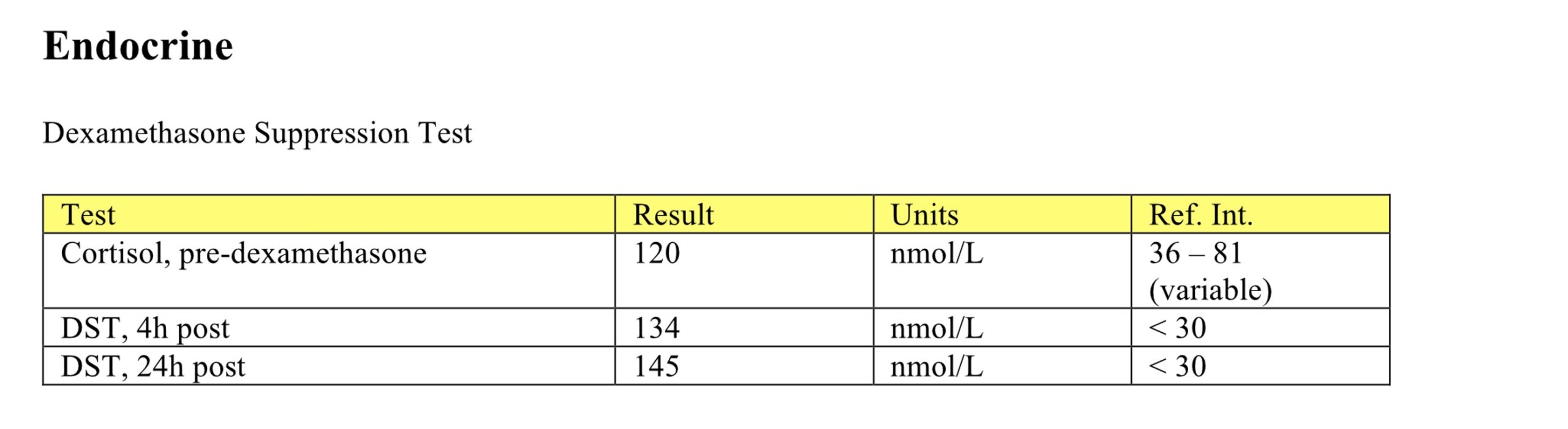
Dexamethasone Suppression Test
Lack of cortisol suppression following administration of dexamethasone is strong evidence of PPID.
- In horses, adenoma(s) or hyperplasia of the pars intermedia of the pituitary gland is responsible for this condition. Although hyperglycemia and glucosuria indicate a diabetic condition, insulin therapy is ineffective because PPID causes insulin-resistance. Gavino was treated with a dopamine agonist and responded well for at least several months. Later follow up is not available.
Case 4. Malika
Malika, a 17-year-old F(s) DSH cat, had a history of polydipsia for several months and was not eating for 1 week. Physical examination revealed a palpable thyroid nodule and a grade III/VI heart murmur.
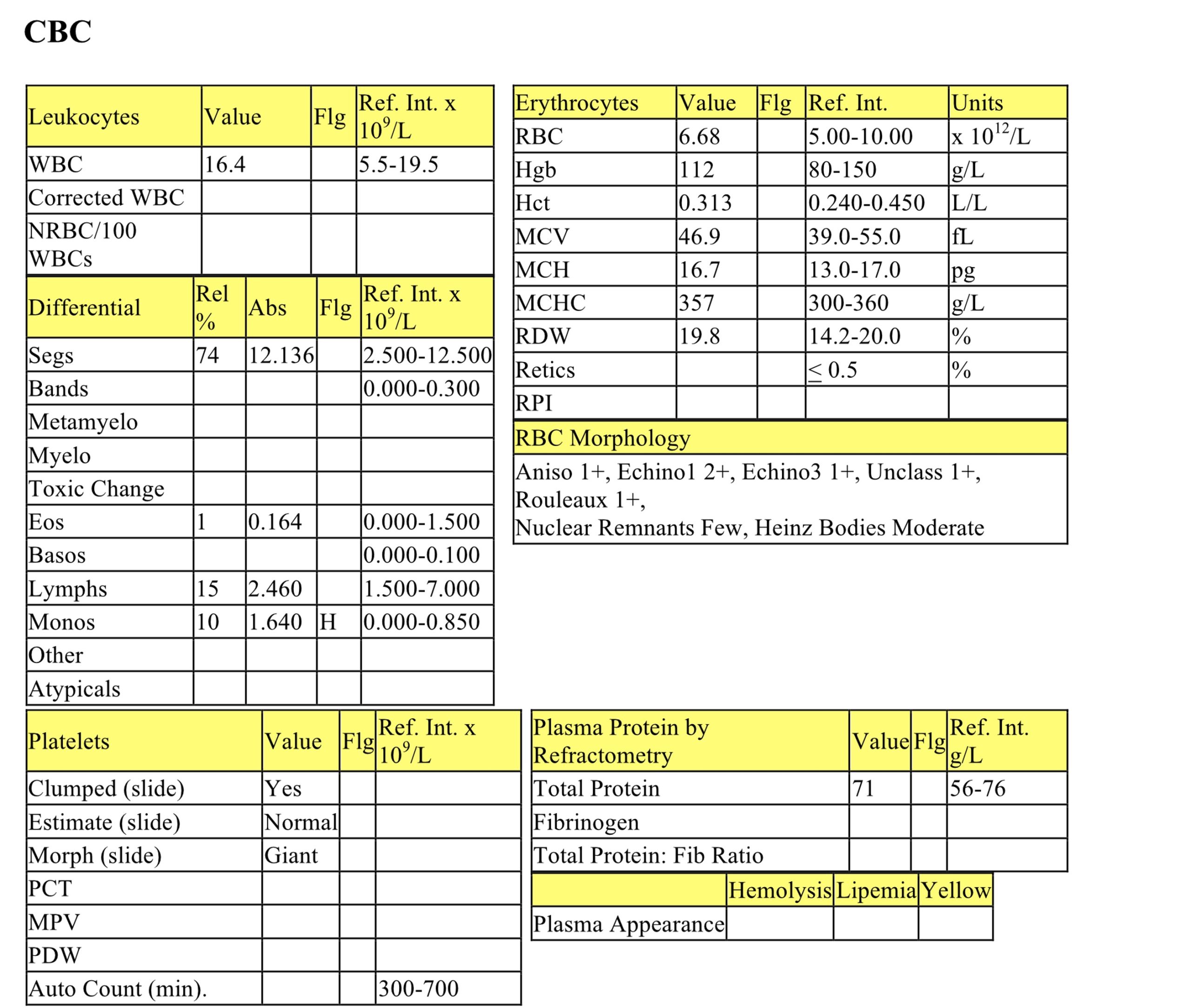
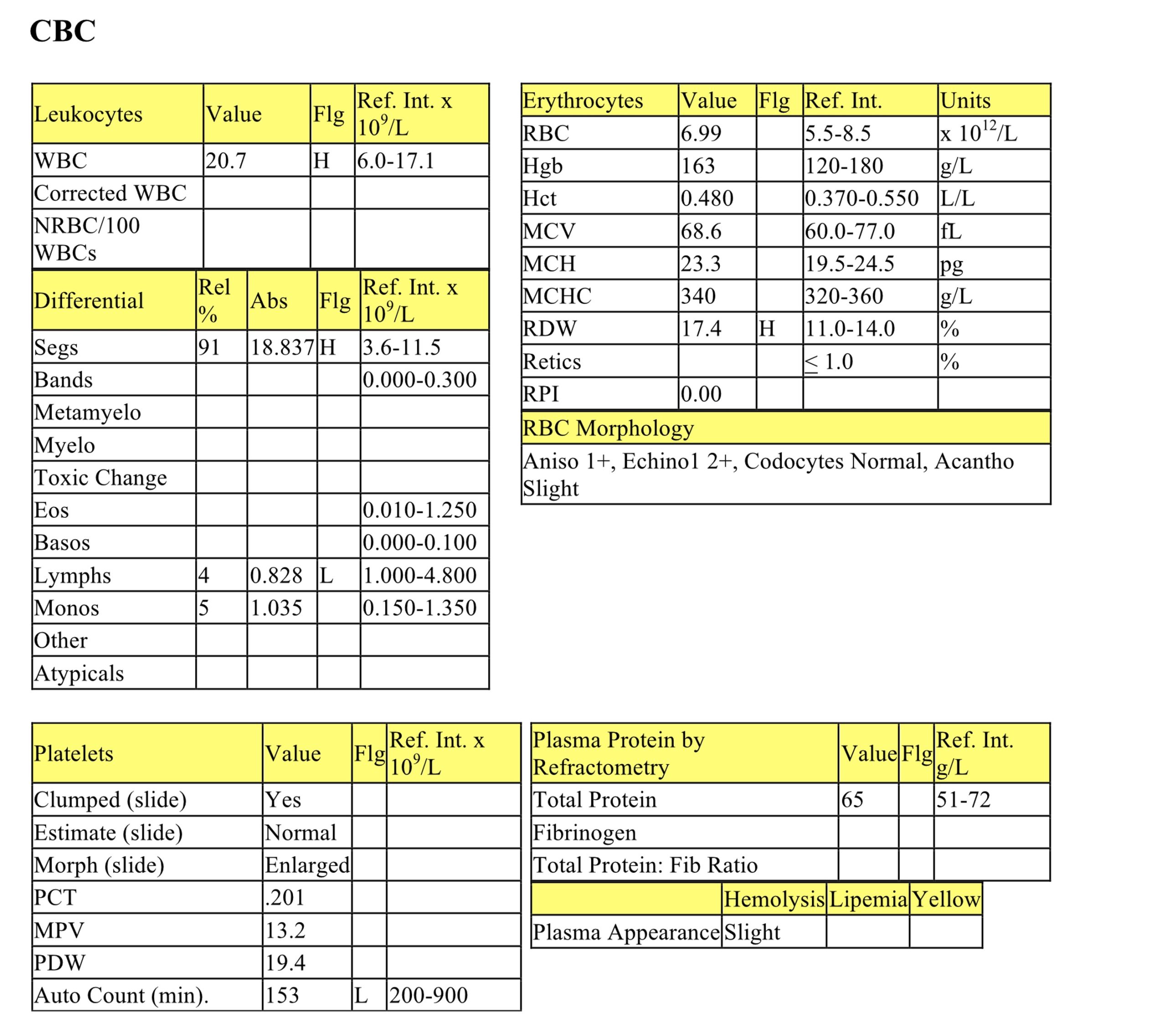
CBC
The erythrogram is unremarkable except for the presence of echinocytes (type 1 and 3) which can be associated with electrolyte and acid-base disturbances, or can be in vitro changes. Unclassified poikilocytosis is non-specific but mechanical injury to erythrocytes could result from increased cardiac turbulence. Moderate Heinz bodies are not likely significant as there is no anemia. Mild monocytosis suggests increased demand for macrophage activity. Monocytosis can also accompany a stress response, but lymphopenia is not present.
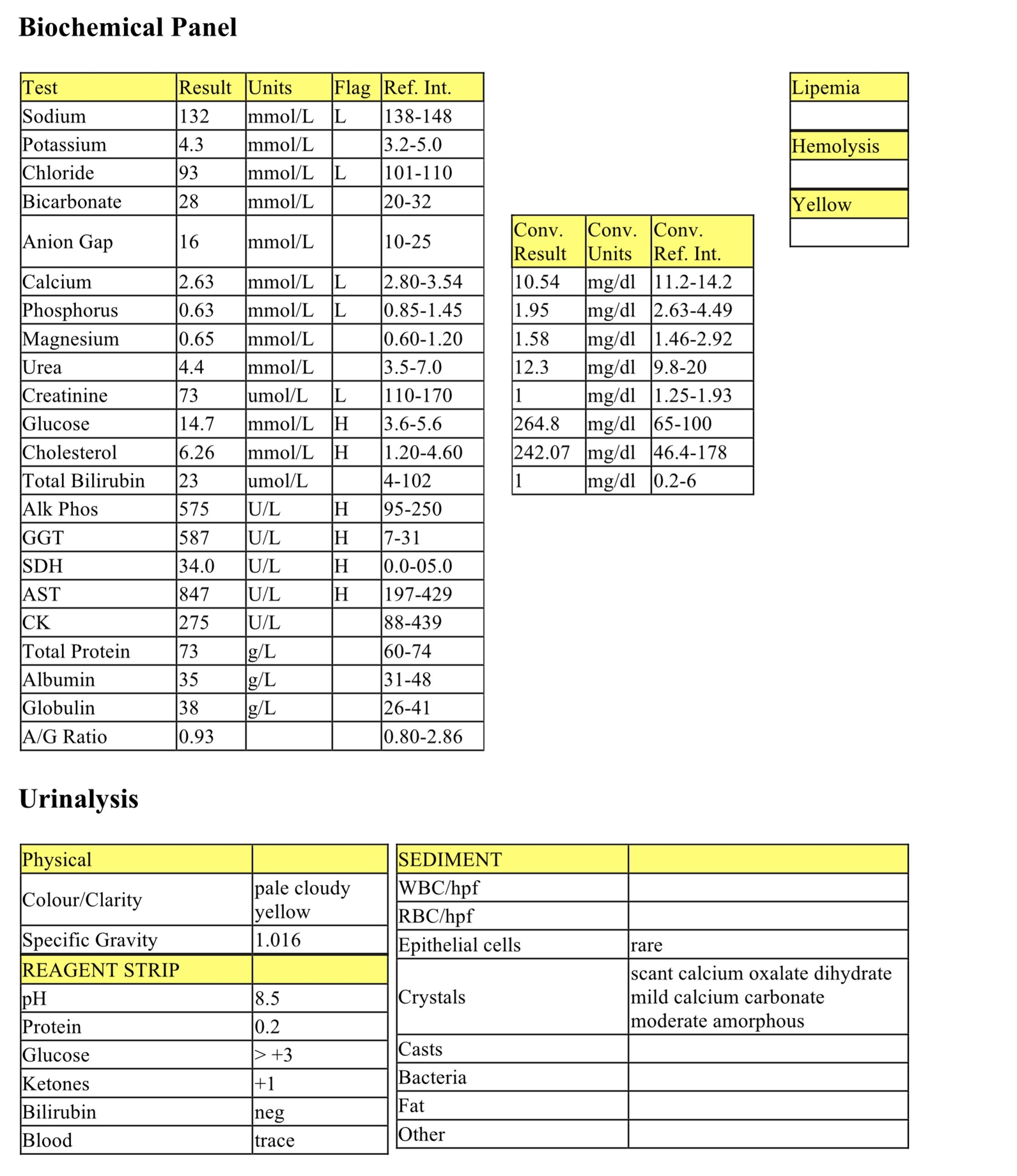
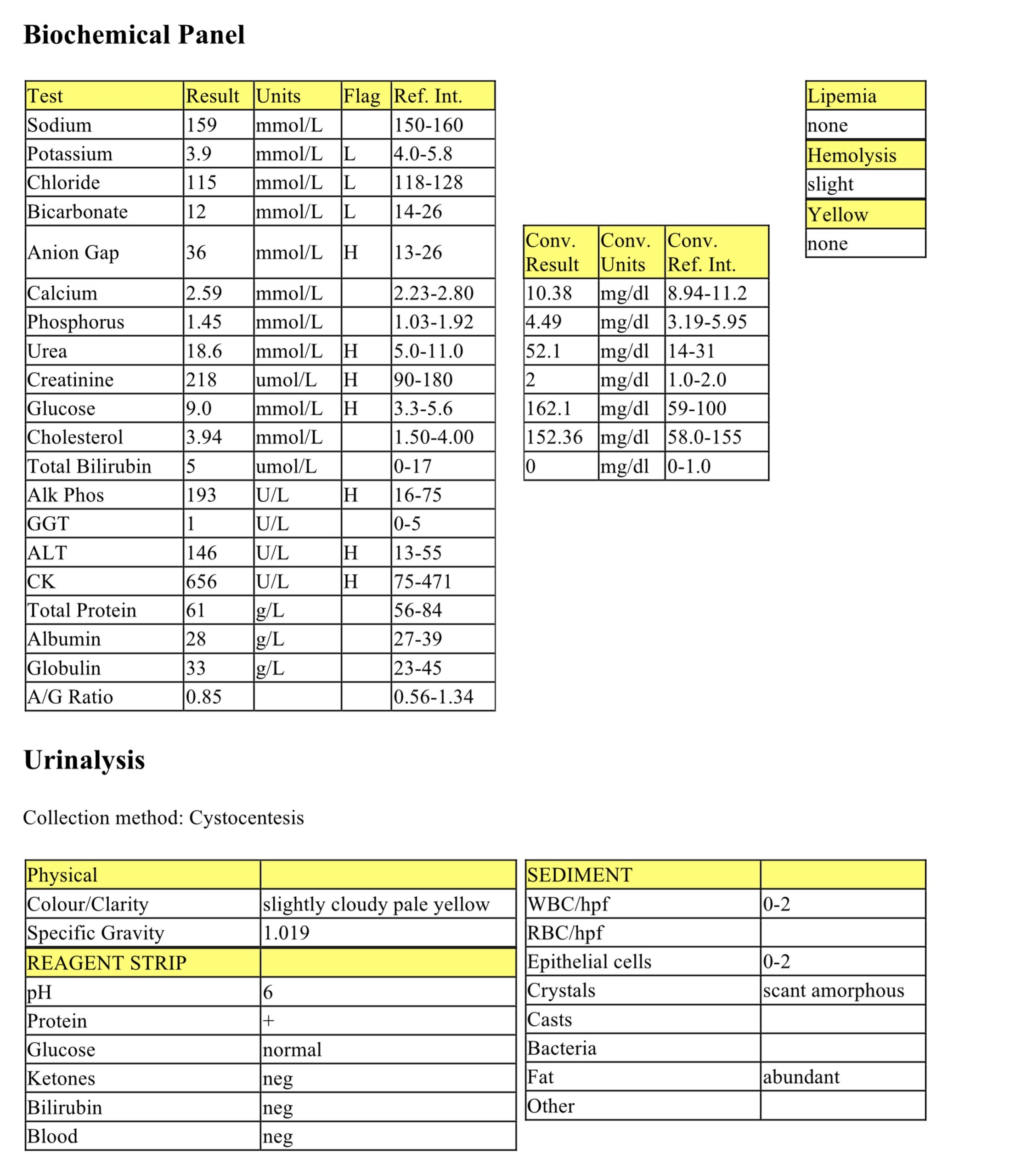
Biochemical Panel
Very mild hypokalemia could relate to renal loss with possible contributions from inappetence. Mild hypochloremia without hyponatremia could be from vomiting, but this is not given in the history. The high anion gap metabolic acidosis may be due to retention of renal acids. Hypochloremia as well as a bicarbonate that is perhaps not as low as might be expected with the degree of increased anion gap suggests a concurrent metabolic alkalosis and, therefore, a mixed acid-base disorder. Mild increases in urea and creatinine indicate renal azotemia, given the lack of urine concentration noted on the urinalysis. Hyperglycemia is probably due to stress or excitement. Moderate increases in ALP and ALT activities suggest hepatobiliary pathology, likely secondary to the heightened metabolic state of hyperthyroidism in this case. The bone isoform also contributes to the increased ALP activity with this disease. Mild increase of CK activity indicates mild muscle injury that may be due to restraint for venipuncture.
Urinalysis
The urine is not concentrated in the face of azotemia, indicating renal disease. Protein at +1 may be significant in this unconcentrated urine and UPC would be recommended to further assess this finding.
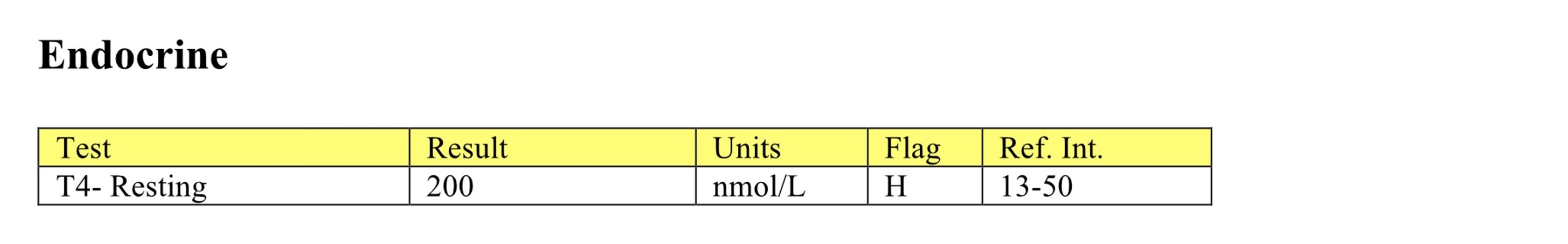
T4
T4 is very high, confirming the diagnosis of hyperthyroidism.
- Malika has both renal disease and hyperthyroidism, a common occurrence in geriatric cats. Hyperthyroidism may cause tachycardia and eventual cardiac disease. No follow-up is available on Malika. As mentioned earlier in this chapter hyperthyroidism increases GFR therefore treatment for hyperthyroidism may exacerbate the renal disease and close monitoring is required.
Case 5. Marigold
Marigold, a 5-year-old F(s) Retriever dog, had a history of obesity and pale mucous membranes.
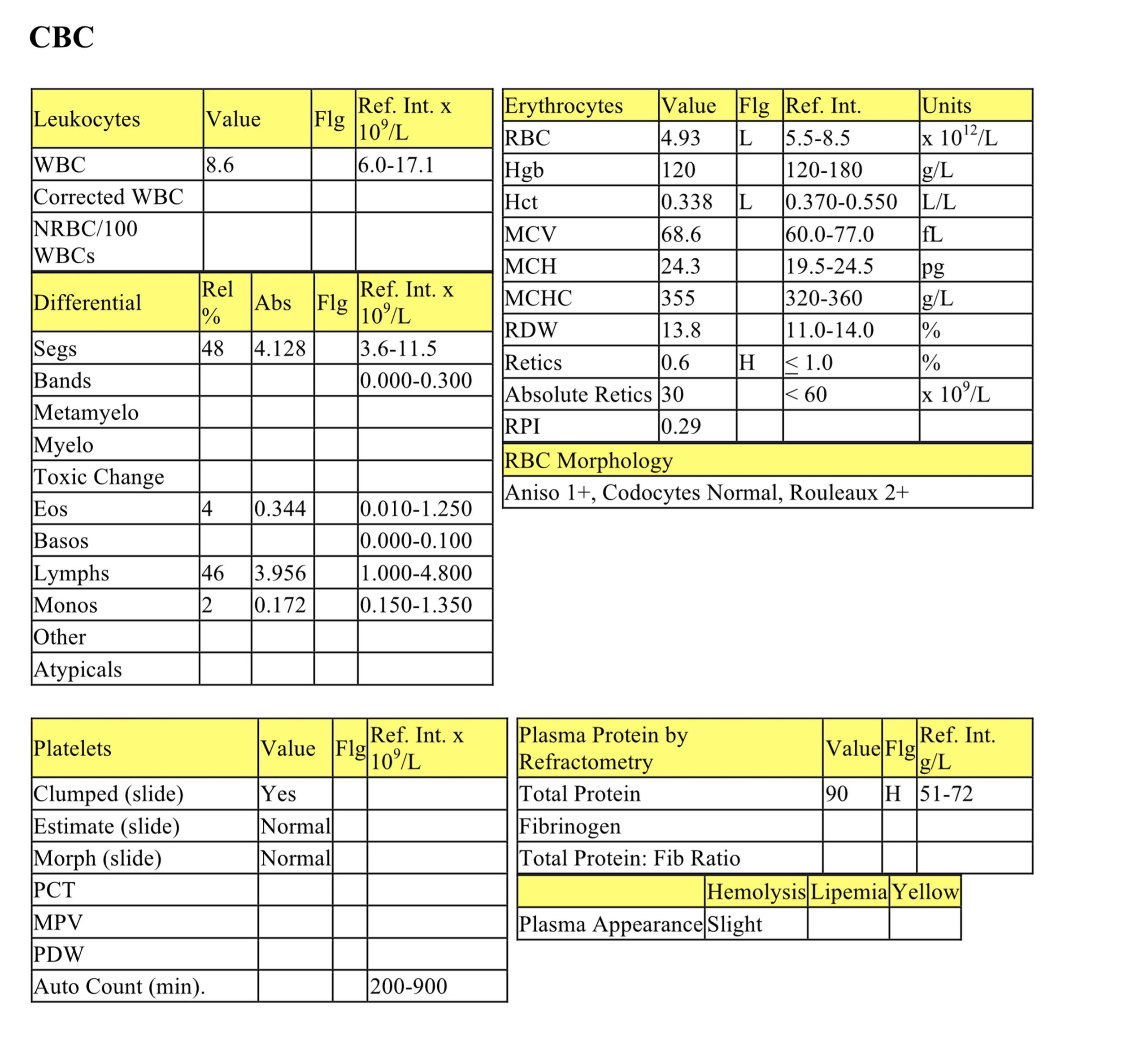
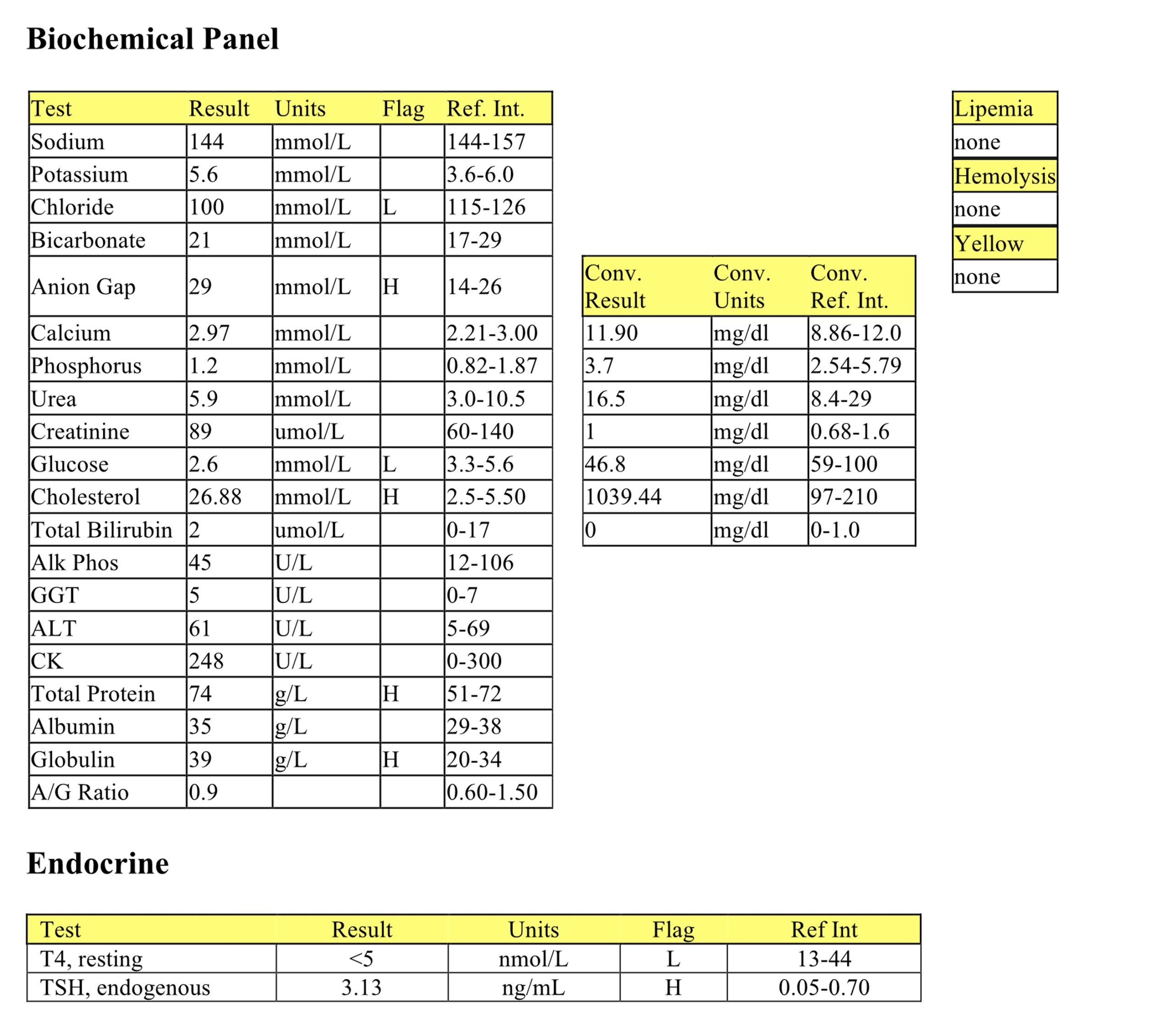
CBC
There is a mild nonregenerative anemia that may be due to significant underlying illness/disease. Increased rouleaux may relate to increased protein. There is interference with the refractometric measurement of protein, as the protein is only mildly elevated on the chemistry panel. In this case, increased cholesterol is probably responsible for the discrepancy.
Biochemical Panel
Moderate hypochloremia with normal bicarbonate and increased anion gap indicate a mixed metabolic alkalosis and acid gain metabolic acidosis. Metabolic alkalosis may be due to vomiting, although this is not reported in the history. The cause of the high gap metabolic acidosis is unclear, but indicates acid gain. In vitro glycolysis explains the low glucose since the serum was not separated from cells prior to submission. Moderate hypercholesterolemia can occur with many conditions, but is most likely due to hypothyroidism in this case. Mild hyperproteinemia with a normal A/G ratio suggests mild dehydration, however there is also a mild hyperglobulinemia that may suggest mild antigenic stimulation.
Given the history and findings of nonregenerative anemia and hypercholesterolemia, hypothyroidism was strongly suspected and T4 and endogenous TSH measurement were recommended.
T4 and Endogenous TSH
Very low T4 and elevated endogenous TSH, in a dog that is not clinically ill (therefore, not “sick” euthyroid), confirm the diagnosis of hypothyroidism.
- Marigold was treated with thyroid hormone supplementation and responded very well. Although the CBC and biochemical panel were not repeated, anemia and hypercholesterolemia tend to correct rapidly with appropriate treatment for hypothyroidism.
Case 6. Marly
Marly, an 8-year-old F(s) Maltese dog, had a history of vomiting and listlessness for 2 days, and was presented in a state of collapse.
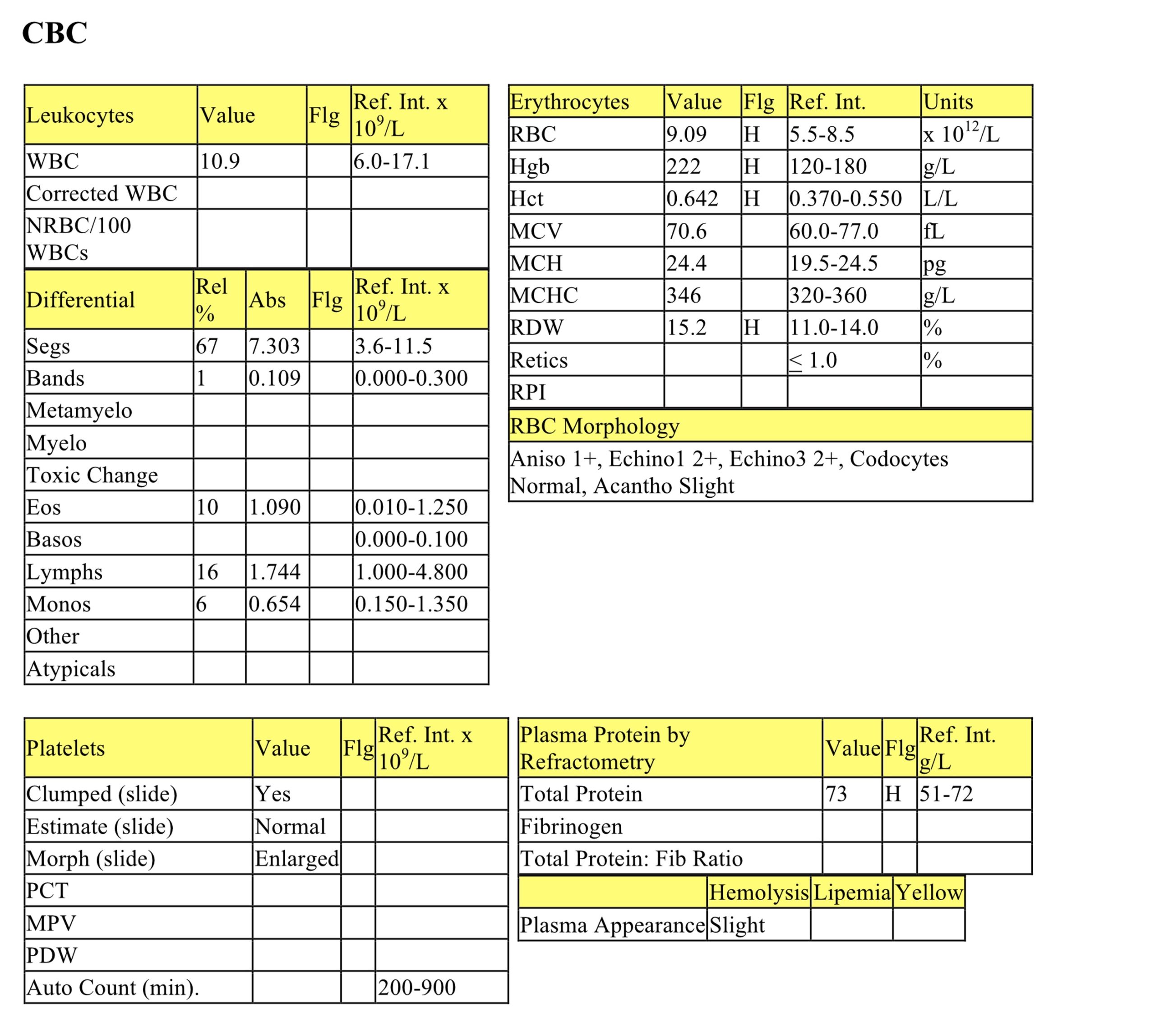
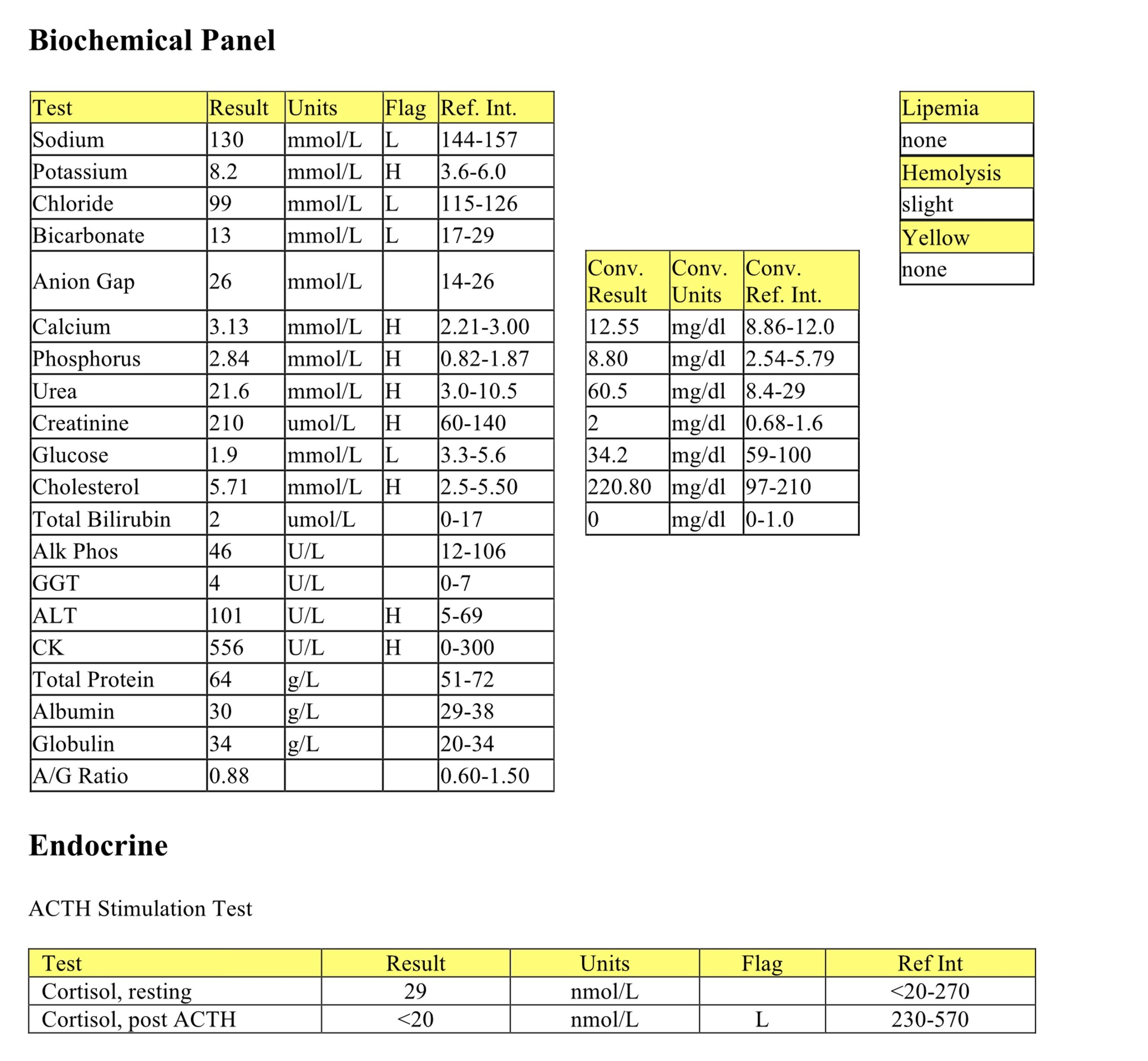
CBC
Moderate erythrocytosis is likely from dehydration, although this is not reflected in the protein (on the biochemical panel). The plasma protein is higher than the serum protein likely due to interfering substances (such as urea and cholesterol in this case) that may interfere with the refractometric protein reading, falsely increasing the result. There is a lack of a stress leukogram in a very ill dog, which could signal hypoadrenocorticism.
Biochemical Panel
Moderate hyponatremia and hypochloremia, together with marked hyperkalemia, suggest mineralocorticoid lack. The Na:K ratio is <23:1 at 15:1. Metabolic acidosis without an increased anion gap reflects bicarbonate loss via the intestine or kidney. There are many differentials for hypercalcemia, but glucocorticoid lack is most likely in this case. Hyperphosphatemia may be secondary to decreased GFR. Mild azotemia is probably prerenal from reduced renal perfusion in this hypovolemic patient. Urine was not available. The low glucose is accurate in this case, and is due to glucocorticoid lack. Mild hypercholesterolemia is present; dogs with hypoadrenocorticism may have decreased, normal, or increased cholesterol concentrations. Mildly increased ALT activity is probably from poor perfusion of the liver under this shock-like condition. The mild increase in CK activity may be from handling/venipuncture, however decreased muscle perfusion due to hypovolemia may also be possible. Hypoadrenocorticism, with both glucocorticoid and mineralocorticoid lack, is suspected, and ACTH stimulation testing is recommended.
ACTH stimulation
Resting cortisol is low normal and there is no response to ACTH, confirming the diagnosis of hypoadrenocorticism.
- Marly was treated with fluids, prednisone, and fludrocortisone and responded very well. The initial dehydration was not reflected in Marly’s protein concentration. Hypoproteinemia often accompanies hypoadrenocorticism and is poorly explained. Hypercalcemia is corrected with therapy; glucocorticoid promotes calcium excretion by the kidneys. Urine is often not concentrated with hypoadrenocorticism because chronic hyponatremia impairs the corticomedullary concentrating gradient in the kidney, and azotemia is common. Similar electrolyte and acid-base abnormalities can also be seen with renal disease, and this could lead to a misdiagnosis of renal disease. In Marly’s case, the lack of a stress leukogram and hypoglycemia were important clues that supported the diagnosis of hypoadrenocorticism. Also, the azotemia was not sufficiently severe to explain the marked electrolyte changes and clinical presentation. Renal concentrating ability is restored when the sodium concentrations are returned to normal with appropriate mineralocorticoid supplementation. Marly continues to thrive, several years following the initial diagnosis.
All tests on the complete blood count (CBC) that evaluate erythrocytes, including morphologic examination on the peripheral blood smear.
Impaired bile flow.
Break-down product of hemoglobin.
Abnormal uncontrolled growth of cells that are unresponsive to normal physiologic growth controls; may be benign or malignant.
Variation in cell size.
An anucleate (in mammalian species) cytoplasmic fragment arising from a megakaryocyte; vital for primary hemostasis.
Glycogen accumulation within hepatocytes due to chronically increased corticosteroid levels (e.g. due to treatment with glucocorticoids or hyperadrenocorticism)
Erythrocyte with even projections all around its membrane; often an artifact but can be a pathologic change. Echinocytes are classified as types 1 and 3 depending on the length and sharpness of the projections (spicules).
Disorder in which there is a concurrent acidosis and alkalosis; pH and bicarbonate values may be within reference intervals.
Azotemia due to renal disease.
“Stack” of red blood cells resembling a roll of coins; prominent in equine and often feline blood. Formation increases as negative charges between RBCs decrease (e.g. with increased plasma proteins).

