Parathyroid Gland
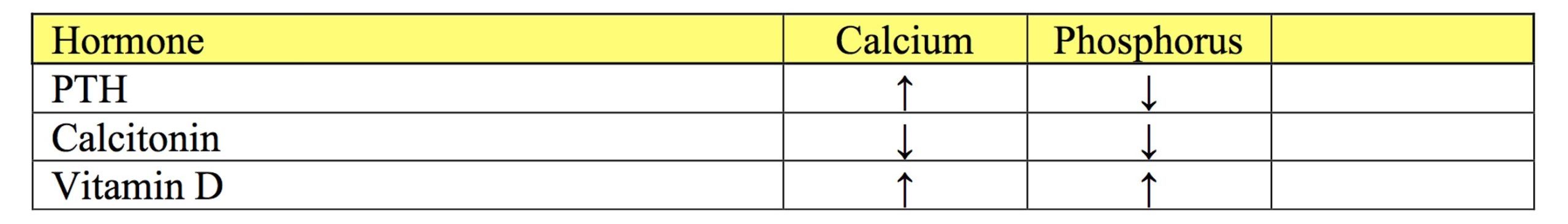
The parathyroid glands regulate calcium and phosphorus metabolism in the body through the actions of parathyroid hormone (PTH), calcitonin, and vitamin D. PTH is released in response to small decreases in free calcium concentration and acts in the distal tubules and collecting ducts of the kidneys to promote calcium reabsorption, in the intestine to promote calcium absorption in the presence of vitamin D, and in bone to promote release of calcium and phosphorus. Conversely, PTH acts to decrease serum phosphorus by promoting phosphorus excretion by the kidneys. Calcitonin is produced by the parafollicular or C-cells of the thyroid gland in response to hypercalcemia. Calcitonin inhibits bone resorption by PTH and promotes phosphorus excretion by the kidneys. Vitamin D increases serum calcium and phosphorus by acting at the level of the kidneys, intestine, and bone (Table 10.1).
Free calcium participates in several important processes in the body and serum concentrations are tightly controlled. There are serious consequences of both hypocalcemia and hypercalcemia. Normally, total serum calcium is measured and comprises three forms: calcium bound to protein, albumin primarily, but also globulins (~40%); calcium complexed with nonprotein anions such as citrates and phosphates (~10%); and calcium which is free/unbound (~50%). Free calcium is often incorrectly referred to as ionized calcium but in fact all calcium in body fluids is ionized, not only the free form.
Total calcium is affected by changes in protein and albumin. Decreases in protein or albumin concentrations result in decreased total calcium due to the large component which is protein bound. However, the active, free calcium component is not affected by these changes. Similarly, hemoconcentration causing hyperproteinemia and hyperalbuminemia results in relative hypercalcemia. Clinical signs of hypercalcemia and hypocalcemia do not occur with increased and decreased protein concentrations since the free calcium component is unchanged. Formulas are available to correct serum calcium according to changes in protein. However, the adjusted value is only an estimate and may not provide additional information beyond the basic principle that total calcium varies directly with protein concentration. Acid-base disturbances also affect the proportion of calcium which is free/unbound. Acidosis increases free calcium concentration and alkalosis decreases free calcium concentration.
PTH; hormone that increases serum calcium levels.
Hormone produced by the parathyroid gland that acts to decrease serum calcium levels.
Calcium that is not bound to proteins in serum and is biologically active.
Most abundant plasma protein in health; maintains oncotic pressure.
Ions with a negative charge.
Process that adds base (HCO3-) to the blood or removes acid (H+); blood pH may or may not be increased.

