Case studies
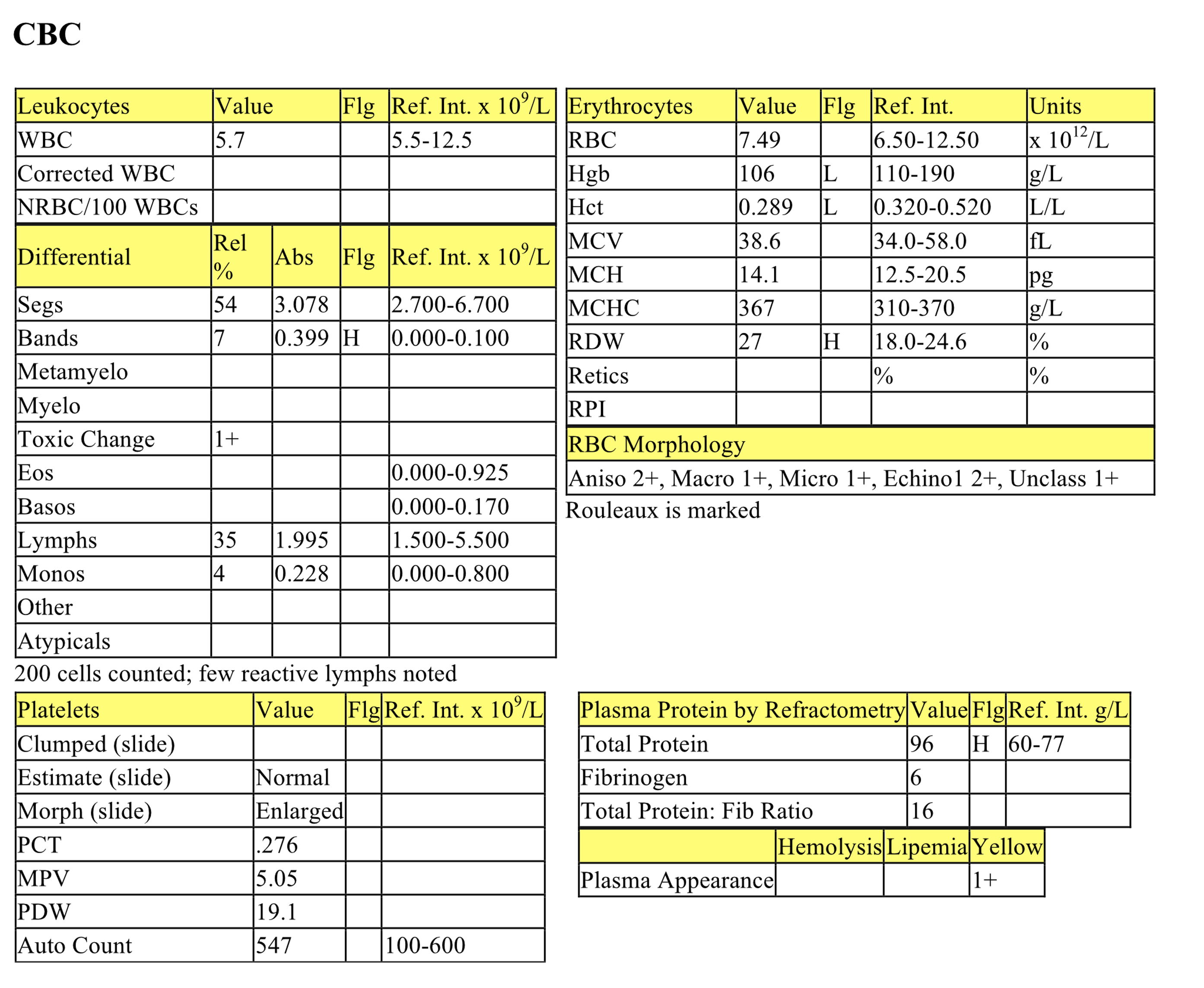
Case 1. Tess
Tess, a 5-month-old F Golden Retriever dog, had a history of poor growth.
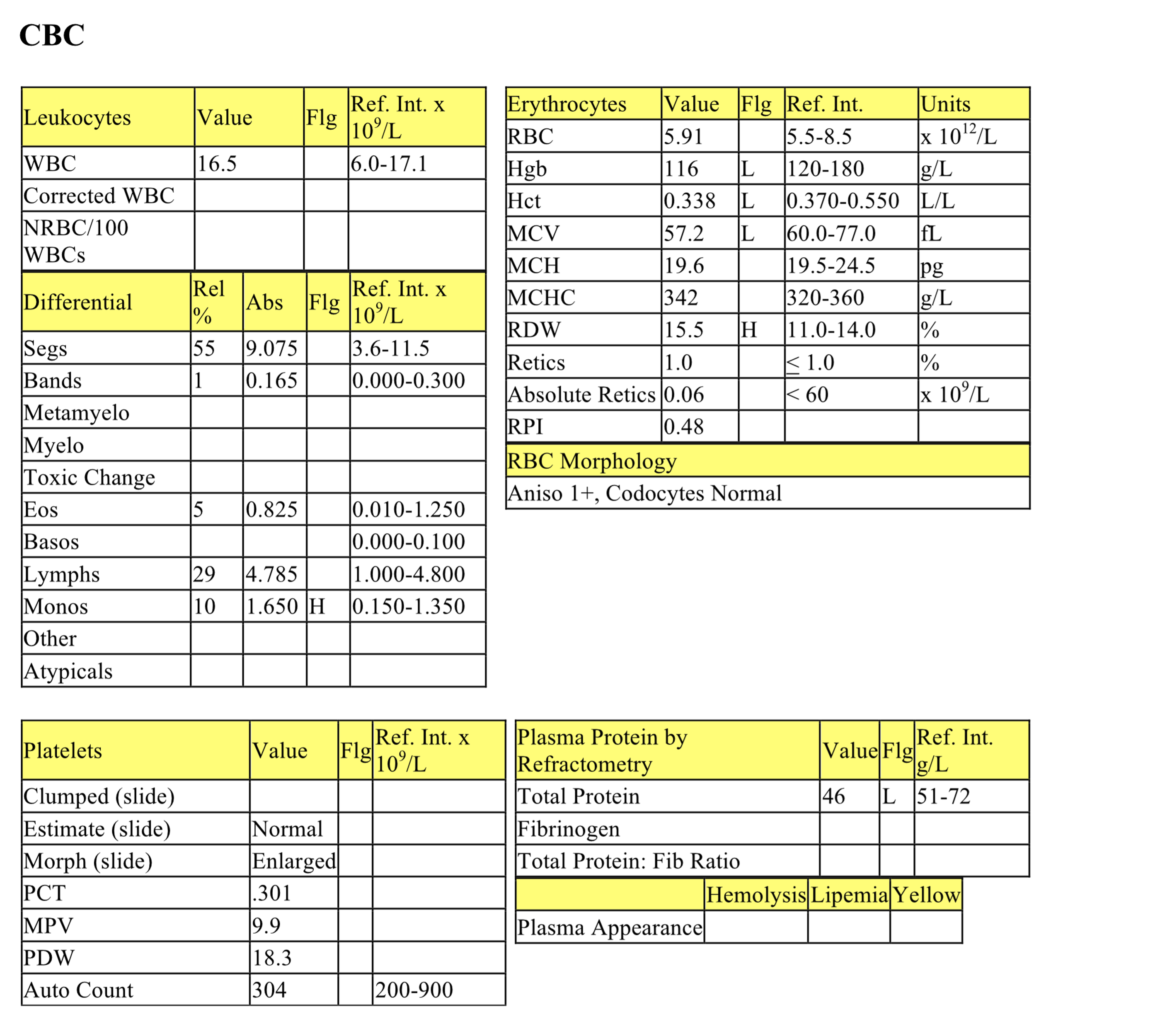
CBC
There is a mild anemia that is nonregenerative and slightly microcytic (decreased MCV). The WBC count is high normal and the leukogram is characterized by normal neutrophil and eosinophil numbers, high normal lymphocytes, and mild monocytosis. High normal lymphocyte numbers probably relate to antigenic stimulation from receiving the first vaccination series. Mild monocytosis may indicate increased demand for macrophage activity. Hypoproteinemia together with nonregenerative anemia could result from acute blood loss with insufficient time to mount a regenerative response; however, the history does not support this interpretation. The anemia may be due to serious underlying disease. Microcytosis may be seen with hepatic disease (PSS), especially in young dogs. Iron stores are adequate in these cases. The hypoproteinemia likely relates to lack of production by the liver.
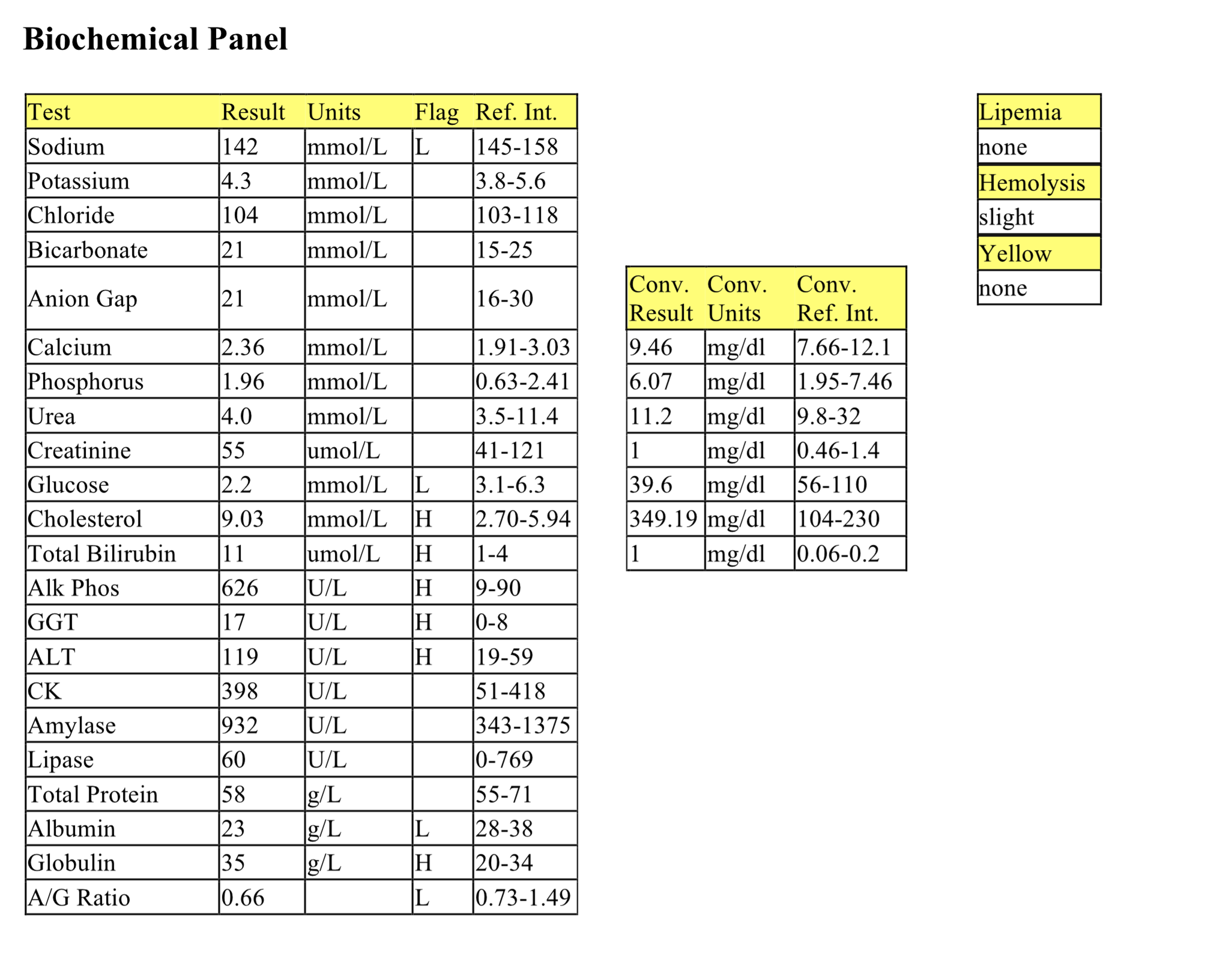
Biochemical Panel
Slightly low anion gap is from low albumin (“unmeasured” anion, not used in the calculation of anion gap). Mild hyperphosphatemia and increased ALP activity are from bone growth and turnover in this young dog. ALP activity could also signal cholestasis. Low urea can occur with low protein intake, diuresis, or decreased urea synthesis by the liver, the latter two possibilities being most likely in this case. Low normal creatinine suggests low muscle mass, which is not unusual in young animals. Mild hyperglycemia could be postprandial sampling or stress-related. Mildly increased ALT activity indicates mild hepatocellular injury. Mild to moderate panhypoproteinemia (decreased total protein with low concentrations of both albumin and globulin) is typically due to increased loss of all proteins (e.g. as with protein-losing enteropathy), or decreased production. Hepatic dysfunction most commonly causes hypoalbuminemia; globulins are more variable and can be decreased, normal, or increased. Low concentrations of globulins suggest decreased production of lipoproteins, several transport proteins, and acute phase proteins, along with possible decreased stimulation of the immune system.
Urinalysis
The specific gravity represents hyposthenuria and indicates that Tess is probably polyuric and polydipsic. These clinical signs are common in animals with hepatic dysfunction, particularly when urea synthesis is affected. Urea contributes to the corticomedullary concentrating gradient in the kidney and very low concentrations can result in an inability to concentrate urine. The remainder of the urinalysis is unremarkable. Ammonium urate crystals are not present.
Bile Acids
The fasting bile acid concentration is only mildly elevated, but the postprandial concentration is very high. Increased bile acids indicate abnormal enterohepatic circulation and reuptake of bile acids by hepatocytes.
- Tess was diagnosed with an intrahepatic PSS. Large breed dogs more commonly have intrahepatic shunts, whereas small breed dogs and cats generally have extrahepatic shunts. Tess underwent surgery to correct the shunt and responded well.
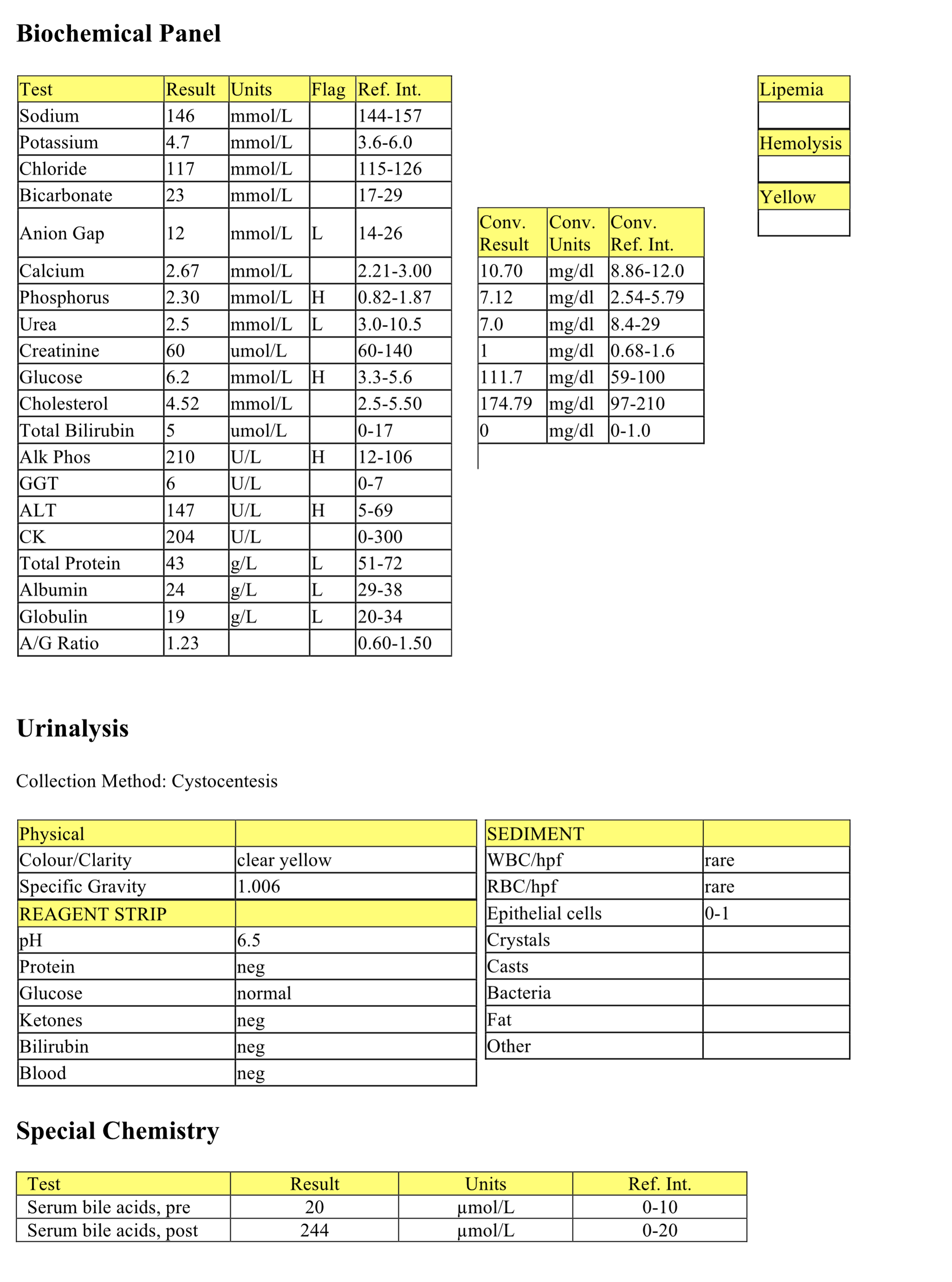
Case 2. Tigger
Tigger, a 6-year-old M(c) DSH cat, had a history of reduced food intake for 2 months, anorexia for 4 days, and vomiting for 1 day. Physical examination revealed yellow mucous membranes.
CBC
The erythrogram is unremarkable except for the presence of unclassified poikilocytosis. Increased poikilocytosis (especially echinoelliptocytes, which were not noted here) can be associated with hepatic disease in cats. The leukogram is generally unremarkable except for the presence of mild lymphopenia consistent with stress of illness. Protein is high normal suggesting dehydration, likely secondary to vomiting. The yellow plasma corresponds to hyperbilirubinemia (discussed below).
Biochemical Panel
Mild increases in sodium and chloride could be due to dehydration with water loss in excess of solute loss. Mild hyperkalemia may be due to decreased renal excretion associated with dehydration; however there is no azotemia to support severely reduced renal blood flow (discussed below). Mild hyperglycemia suggests stress as postprandial hyperglycemia is ruled out by the history of anorexia. Mild hypercholesterolemia is likely secondary to cholestasis, possibly with concurrent deranged lipid metabolism. Moderate hyperbilirubinemia is likely due to intrahepatic cholestasis in this case. ALP activity is very high, particularly for this species, and indicates increased synthesis of the enzyme in response to cholestasis. GGT activity is only mildly increased, perhaps because the cholestasis is secondary to accumulation of lipid within hepatocytes which then impinge on bile canaliculi. GGT activity may be more pronounced with disorders such as bile duct obstruction or ascending cholangiohepatitis with concurrent bile duct hyperplasia. Mildly increased ALT activity indicates mild hepatocellular injury. High normal albumin supports dehydration. Despite evidence for volume contraction, urea and creatinine concentrations are not increased. These results may be underestimated if urea synthesis is limited by lack of protein intake and/or hepatic dysfunction, and creatinine synthesis is limited by decreased muscle mass from chronic inappetence.
Urinalysis
The urine is not concentrated; however, Tigger had received fluid therapy before urine could be obtained. Bilirubinuria and bilirubin crystals in the urine are abnormal in cats and reflect hyperbilirubinemia which has exceeded the renal threshold. Moderate calcium oxalate dihydrate crystals may be seen in healthy cats and dogs and also with uroliths composed of calcium oxalate; further evaluation may be required if there are symptoms compatible with uroliths. 1+ protein should be monitored for persistence and a UPC considered if protein persists and the sediment is “inactive”. Trace glucose may relate to hyperglycemia, however at this time the serum glucose is not above the renal threshold. It is possible that this cat may have previously had stress hyperglycemia that reached a magnitude exceeding the renal threshold, hence causing mild glucosuria. Another possible explanation for the trace glucosuria is renal tubular injury whereby the renal tubules are unable to reabsorb glucose within the renal tubules. 3+ blood on the urine reagent strip and 2-4 RBCs/hpf indicate mild hematuria which cannot be interpreted since the method of urine collection is ”other”. For example, if urine had been collected by manual expression (categorized as “other”), hematuria could be iatrogenic.
Differentials considered in this case included hepatic lipidosis, cholangiohepatitis, bile duct obstruction, hepatic neoplasia, pancreatitis. The next steps required to establish a definitive diagnosis in such a case would include imaging of the abdomen to evaluate the liver and pancreas (size, presence of nodules/masses), FNA of liver, biopsy of the liver (and any other abnormal tissues) followed by histopathological examination.
- Tigger was diagnosed with hepatic lipidosis, which occurs in overweight cats that become inappetent or anorexic for whatever reason. Hepatic biopsy confirmed the diagnosis.
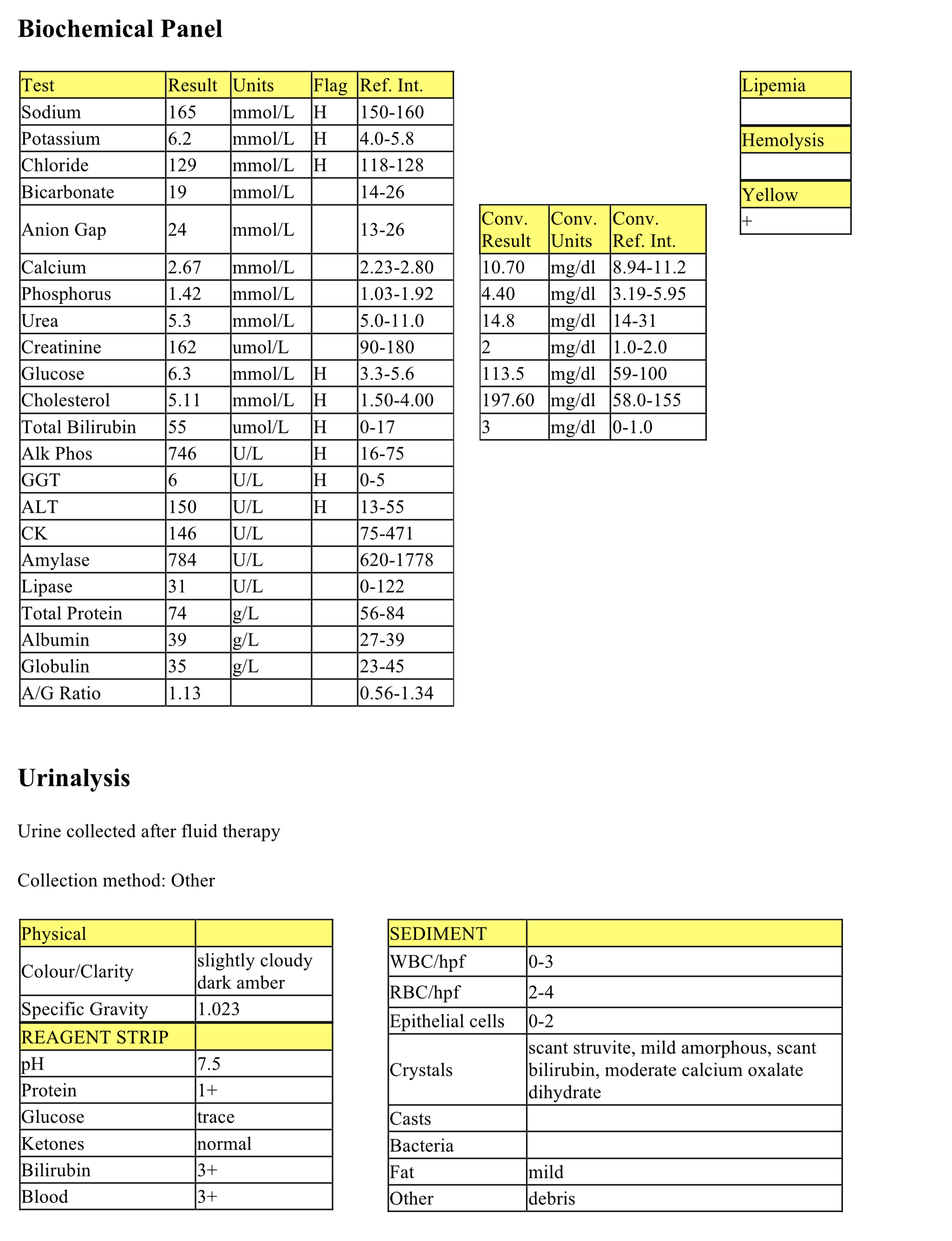
Case 3. Jade
Jade, a 7-month-old F Miniature horse, had a history of poor body condition and not eating or drinking for 3 days. On presentation, she was dehydrated, hypothermic, and weak.
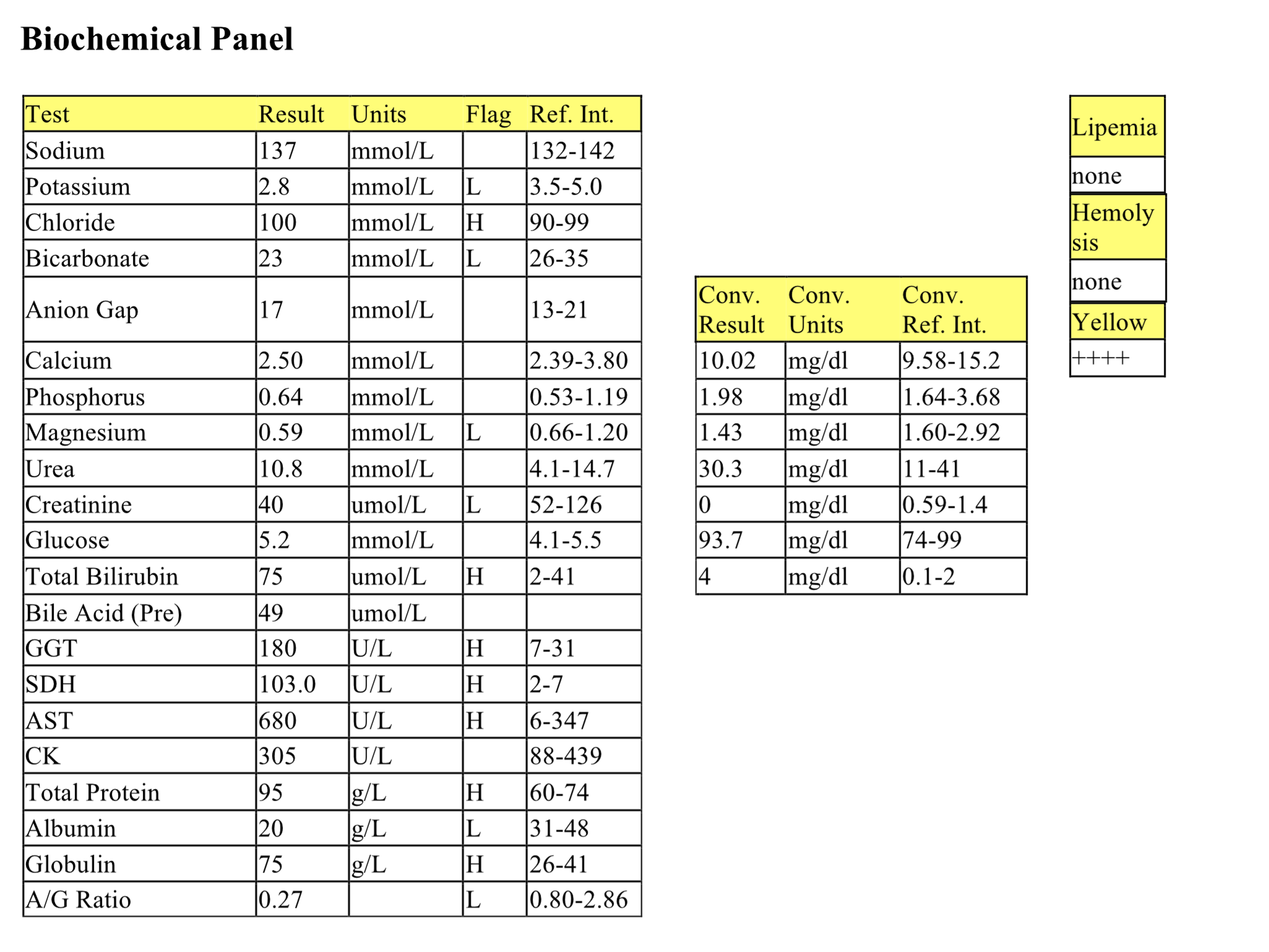
CBC
Mild anemia cannot be further classified given the species since horses rarely release polychromatophilic RBCs/reticulocytes into the peripheral circulation. However, underlying serious illness/inflammatory disease leading to nonregenerative anemia is likely in this case, given the history and other laboratory findings. Also, the anemia may be underestimated given the physical finding of dehydration. Increased rouleaux relates to hyperproteinemia. The presence of microcytes and unclassified poikilocytosis may be an incidental finding in young horses. The presence of macrocytes and microcytes on smear evaluation may be contributing to the increased RDW. The WBC count is low normal and the leukogram is characterized by a low normal neutrophil count with a mild left shift and toxic change. These findings suggest acute inflammation. Although these changes are subtle, the low normal mature neutrophil count is concerning; close monitoring of the CBC would be recommended to assess progression of the inflammation and the bone marrow response to the increased demand for neutrophils. Reactive lymphocytes generally indicate immunologic stimulation and can be seen post-vaccinal in young animals and with exposure to infectious/foreign agents. Dehydration may be responsible, at least in part, for the hyperproteinemia. The total protein to fibrinogen ratio is in the “grey zone” (15 – 20) for horses indicating that the high normal fibrinogen (1-6 g/L is normal for horses) could be due to absolute hyperfibrinogenemia, or dehydration, or both.
Biochemical Panel
Mild hypokalemia and hypomagnesemia may be due to lack of intake, however since approximately 30% of serum magnesium is bound to albumin, the hypomagnesemia may also relate to hypoalbuminemia. Mild hyperchloremic metabolic acidosis with a normal anion gap is classified as a secretory acidosis and indicates bicarbonate loss through either the intestinal tract or kidneys. Slightly decreased creatinine is consistent with low muscle mass. Mild hyperbilirubinemia and moderately increased GGT activity suggest cholestasis; anorexia also contributes to bilirubin elevations in horses. Elevations in AST (mild) and SDH (marked) activities indicate hepatocellular injury. Although AST can be released from both muscle and liver, a hepatic source is more likely since CK activity is within the RI. Marked hyperproteinemia is due to increased globulins, possibly from increased acute phase proteins, increased gammaglobulin synthesis from antigenic stimulation, or both. Hypoalbuminemia could be explained by several mechanisms: decreased synthesis as a negative acute phase protein; decreased synthesis from hepatic dysfunction; markedly decreased protein intake; or increased albumin loss (urinalysis not done). Baseline bile acid elevation is explained by decreased functional hepatic mass, biliary stasis, or portosystemic shunting of blood. Note that only one sample for bile acids is required in horses as they have no gall bladder for bile storage. The presence of cholestasis and hyperbilirubinemia confounds assessment of hepatic function based on bile acids.
- Jade was diagnosed with hepatic disease and possibly also hepatic dysfunction. She began seizuring the day following admission to the hospital and was euthanized. Necropsy revealed severe chronic hepatitis, periportal fibrosis, and biliary hyperplasia. The etiology was not determined although ingestion of various hepatotoxins, such as alsike clover, pyrrolizidine alkaloids, and mycotoxins, was considered. Terminal septicemia was also suspected and may explain the neutrophil response noted on the CBC.
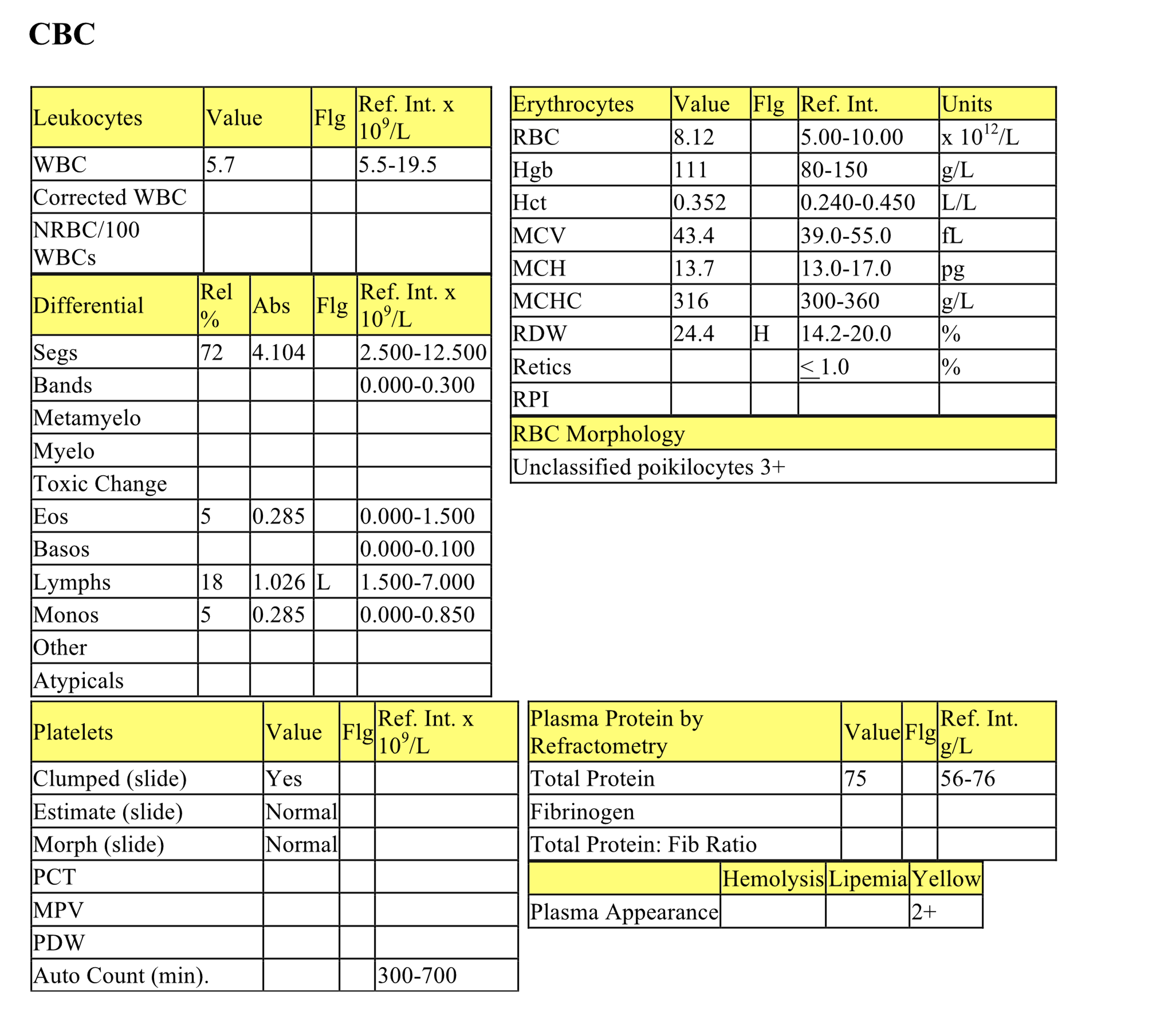
Case 4. Charles
Charles, an 11-year-old M(c) DSH cat, had a history of anorexia and not drinking for 3 days, and weight loss. Physical examination revealed yellow mucous membranes.
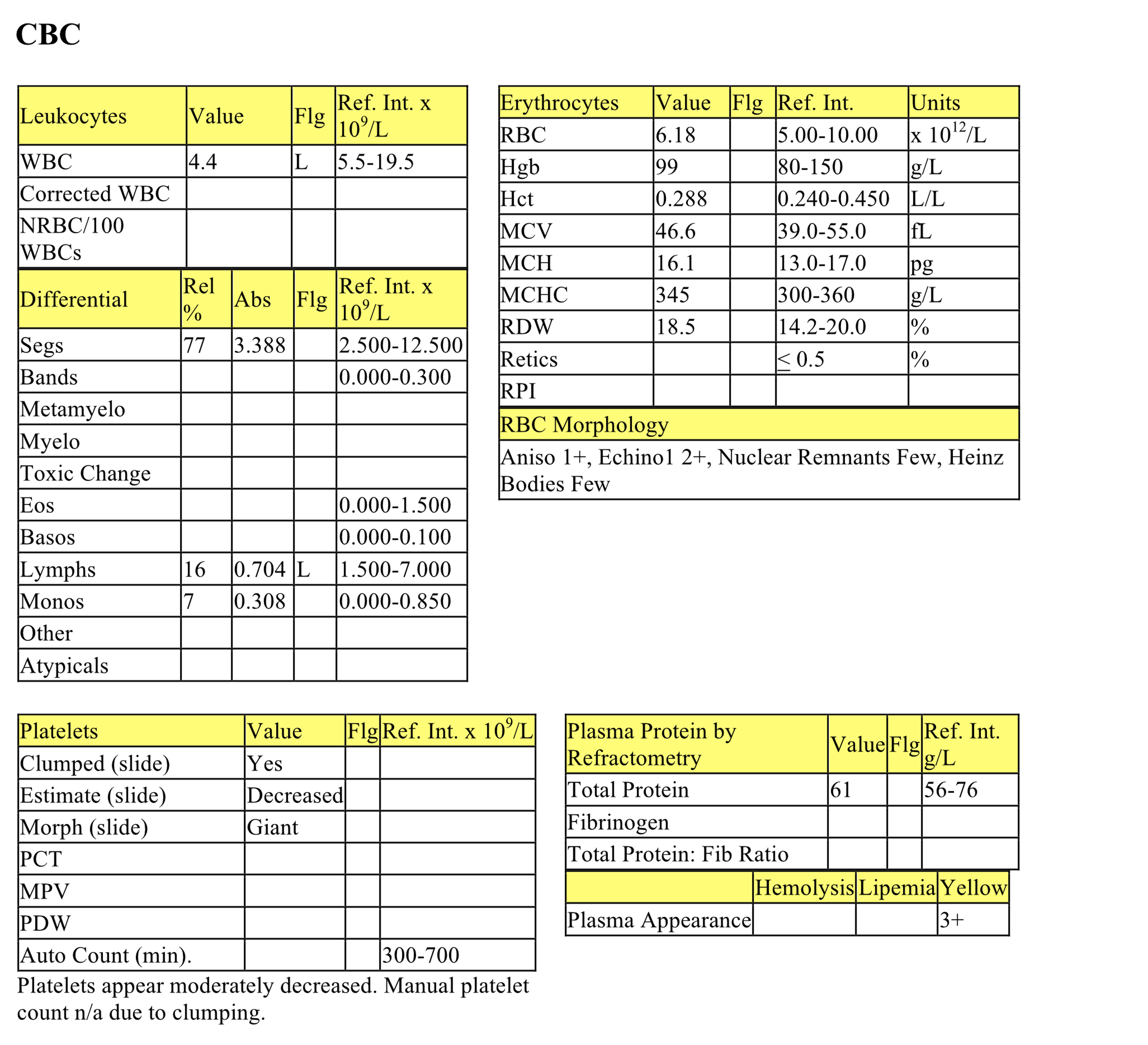
CBC
The erythrogram is unremarkable. There is a mild leukopenia which is entirely due to a moderate stress lymphopenia. The plasma is yellow from hyperbilirubinemia; increased erythrocyte breakdown would not be suspected as a cause of hyperbilirubinemia given the normal hematocrit. Platelets are clumped, but they may be decreased and should be re-evaluated.
Biochemical Panel
The mildly decreased bicarbonate is not associated with an increased anion gap, which suggests bicarbonate loss by the kidneys or intestinal tract. Low creatinine indicates reduced muscle mass. Very mild hyperglycemia relates to stress. Marked hyperbilirubinemia and mildly increased GGT activity indicate cholestasis. The moderate to marked increase in ALT activity is a result of hepatocellular injury. Mild hypoalbuminemia may relate to decreased hepatic synthesis, increased loss, or severely restricted protein intake.
- Charles has evidence of cholestasis and hepatocellular injury. The pattern of hepatic enzyme changes is not typical of hepatic lipidosis where ALP activity is often increased to the greatest degree. Cholangiohepatitis, another differential diagnosis, is usually accompanied by an inflammatory leukogram. Acute biliary obstruction should be considered. Charles underwent surgery to visualize the liver and obtain a biopsy. The liver was uniformly enlarged and yellow. Histologic examination revealed large lymphocytes with prominent nucleoli diffusely scattered throughout the biopsy section. Lymphosarcoma was diagnosed and Charles was euthanized. A necropsy was not done. Although lymphosarcoma had likely been developing within the liver for a long time, bile flow in the distal biliary tract may have very acutely become impeded by the neoplastic process. Severe hyperbilirubinemia and clinical signs of illness may develop very quickly under these circumstances. This might also explain the lack of increase in ALP activity and only mildly increased GGT activity despite the marked hyperbilirubinemia.
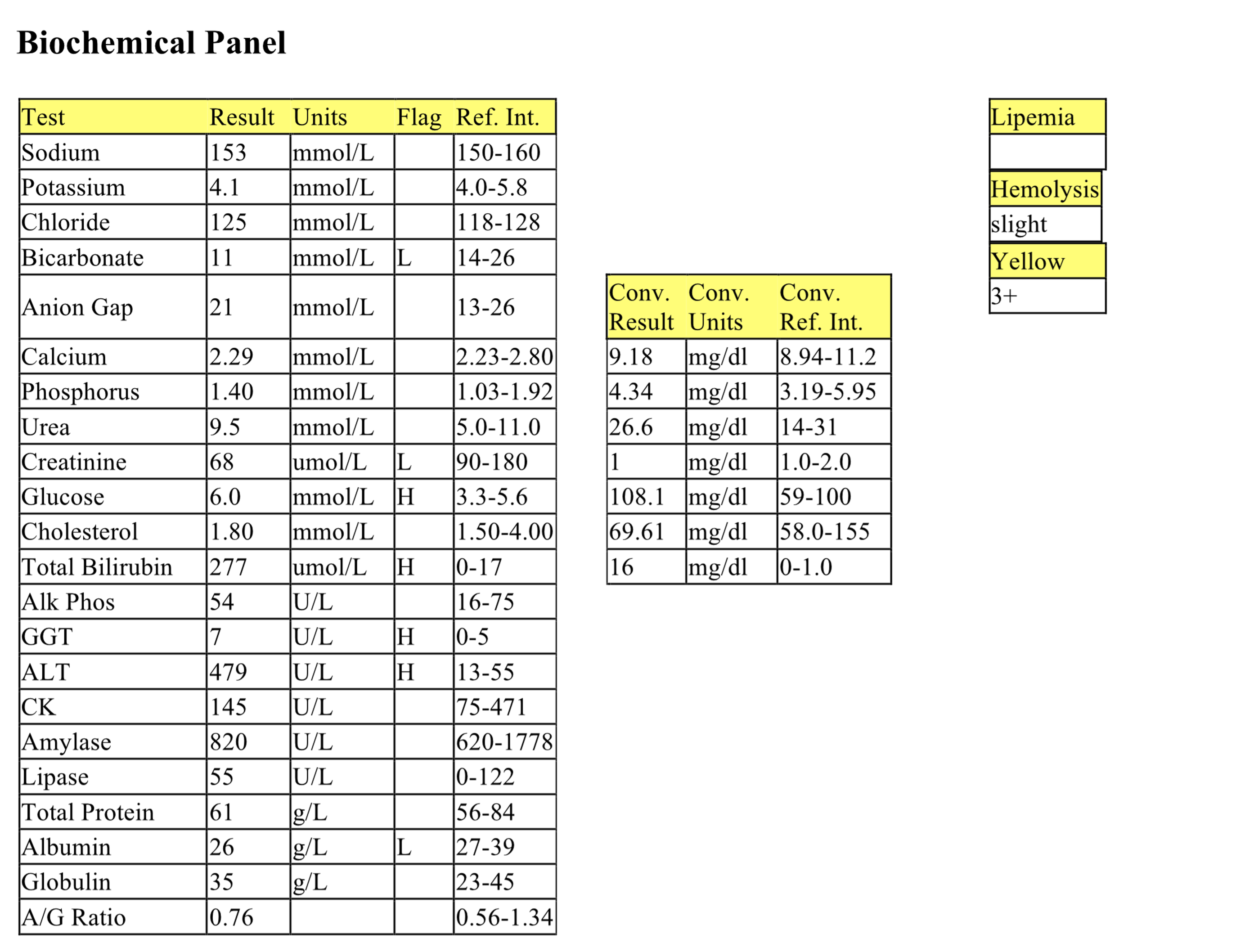
Case 5. Ferdinand
Ferdinand, a 10-year-old M(c) Shetland Sheepdog, was presented with a decreased appetite and decreased water intake. Ferdinand was lethargic on physical examination but did not appear to have abdominal pain.
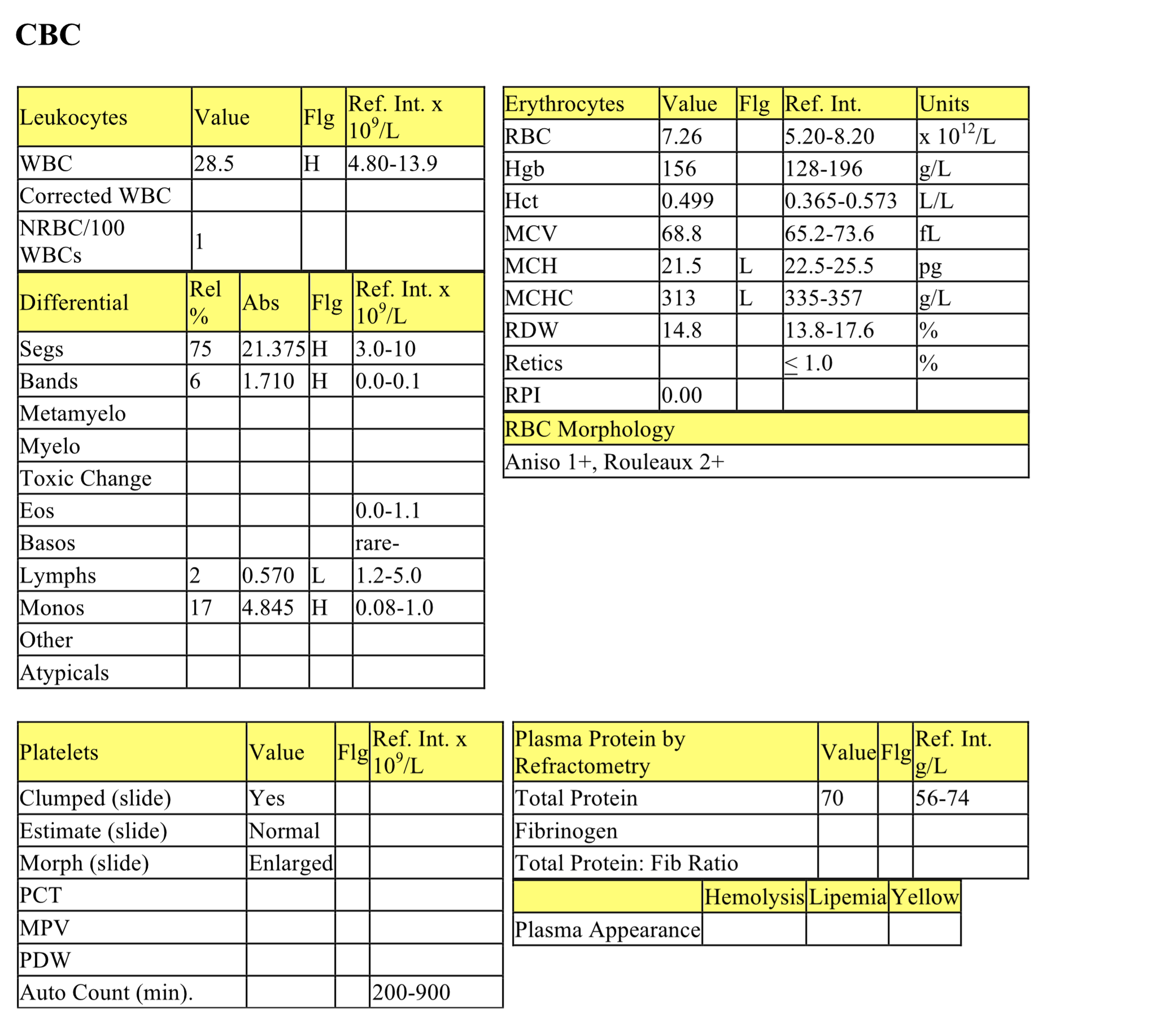
CBC
The erythrogram is unremarkable except for increased rouleaux, which does not correlate with increased protein. Moderate leukocytosis is characterized by a moderate neutrophilia, mild/moderate left shift and moderate monocytosis. There is also a moderate lymphopenia. The leukogram changes are consistent with established inflammation and stress. In addition, monocytosis may signal increased demand for phagocytic activity.
Biochemical Panel
Reduced intake and increased loss from the gastrointestinal tract may explain the mild hyponatremia. The serum was not separated from the cells before submission to the laboratory, therefore, in vitro glycolysis probably explains the low glucose. Mild hypercholesterolemia and hyperbilirubinemia, and moderate increases in ALP and mildly increased GGT activities are consistent with cholestasis. Mild hepatocellular injury is indicated by the mild increase in ALT activity. Mild hypoalbuminemia could result from decreased albumin synthesis as a negative acute phase protein or as a result of hepatic dysfunction. Markedly decreased protein intake is less likely, and urinalysis would be required to evaluate the possibility of renal protein loss. Mild increase of globulins may be due to increased synthesis of globulins secondary to inflammation.
- The inflammatory leukogram and biochemical changes referable to the liver suggest a focus of inflammation involving the hepatobiliary tract. Fine needle aspirates of the liver contained bile casts representing canalicular plugs, and increased numbers of neutrophils which were admixed within hepatocyte clusters. Direct smears of gall bladder contents contained amorphous, acellular blue material consistent with bile. Inflammatory cells were not seen. A very small amount of abdominal fluid was obtained and nucleated cell count and protein could not be determined. However, the cytospin smear revealed high numbers of macrophages and reactive mesothelial cell Many of the macrophages contained blue granular material consistent with bile. Bile peritonitis was diagnosed and Ferdinand underwent surgery. A ruptured gall bladder was found and cholecystojejunostomy performed. The rupture was thought to be due to cholecystitis as the gall bladder wall was thickened and friable. Cholecystitis and cholangiohepatitis may have an increased incidence in Shetland Sheepdogs. Ferdinand recovered.
Average erythrocyte size in femtoliters (measured or calculated PCV or Hct÷RBC).
Granulocyte with fine, inconspicuous cytoplasmic granules and a segmented nucleus; important in phagocytosis and killing of bacteria.
Granulocyte with large, round, pink to orange (eosinophilic) cytoplasmic granules and an often bi-lobed nucleus; important in host response to allergens and defense against parasites.
Mononuclear, non-phagocytic leukocyte responsible for humoral (B lymphocyte) and cell-mediated (T lymphocyte) immune responses.
Increase in the number of monocytes in peripheral blood.
Difference between unmeasured anion and cation concentrations, calculated using the formula: (Na+ + K+) minus (Cl- + HCO3-.)
Concurrent decreased concentration of albumin and globulins.
Association of lipid with protein for lipid transport.
All tests on the complete blood count (CBC) that evaluate erythrocytes, including morphologic examination on the peripheral blood smear.
Increases serum urea and/or creatinine.
Cellular proliferation- increased number of normal cells.
Anucleate (in mammalian species), immature erythrocyte containing cytoplasmic RNA and ribosomes which are precipitated by staining with new methylene blue.
“Stack” of red blood cells resembling a roll of coins; prominent in equine and often feline blood. Formation increases as negative charges between RBCs decrease (e.g. with increased plasma proteins).
Release of less mature neutrophil stages (bands, metamyelocytes, myelocytes) from the marrow into the peripheral blood in response to inflammation.
Cytoplasmic abnormalities seen in neutrophils that have not matured normally in the bone marrow. Abnormalities include retention of primary granules, vacuolation, darker staining due to retention of ribosomes, and deposits of rough endoplasmic reticulum (Döhle bodies).
Organ responsible for production of hemopoietic cells; found in the medullary cavity, especially the ends of long bones (e.g. femur) and flat bones (e.g. the pelvis, sternum.)
Immunologically stimulated lymphocyte that typically has darkly staining cytoplasm
Process that adds acid (H+) to the blood or removes base (HCO3-); blood pH may or may not be decreased.
Red blood cell (RBC); an anucleate (in mammalian species) cell containing hemoglobin needed for oxygen transport. Typically shaped like a bi-concave disk.
Volume of erythrocytes per liter of whole blood. Reported as L/L (calculated: MCV x RBC count). Equivalent to PCV (%) determined by centrifugation of blood in a microhematocrit tube
An anucleate (in mammalian species) cytoplasmic fragment arising from a megakaryocyte; vital for primary hemostasis.
Solid malignant lymphoid tumor.
Technique used to obtain samples for cytologic evaluation, using suction.
Cell lining body cavities that may exfoliate into body cavity fluids when there is inflammation or accumulation of excess fluid for other reasons; mesothelial cells can become phagocytic.

